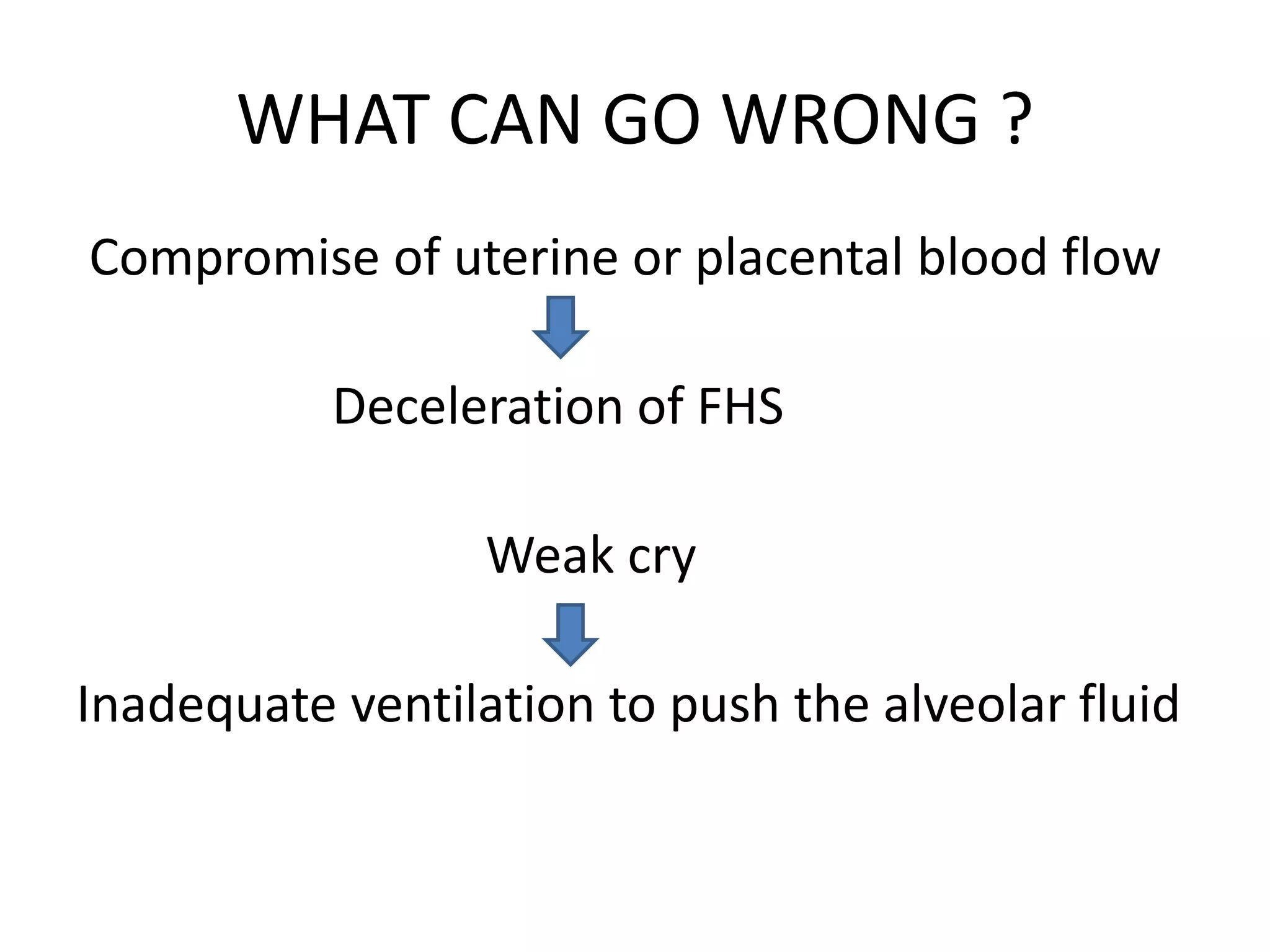
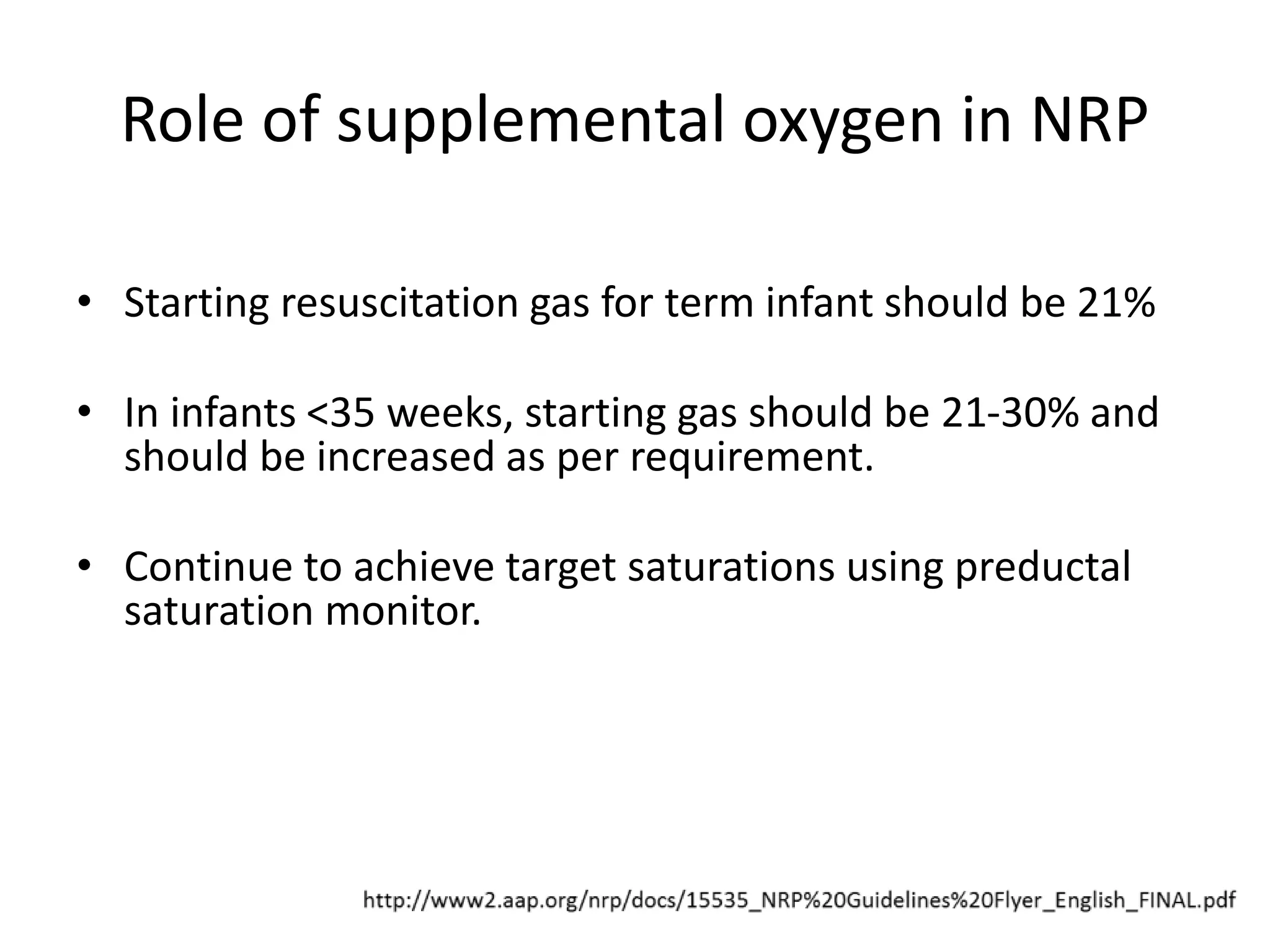
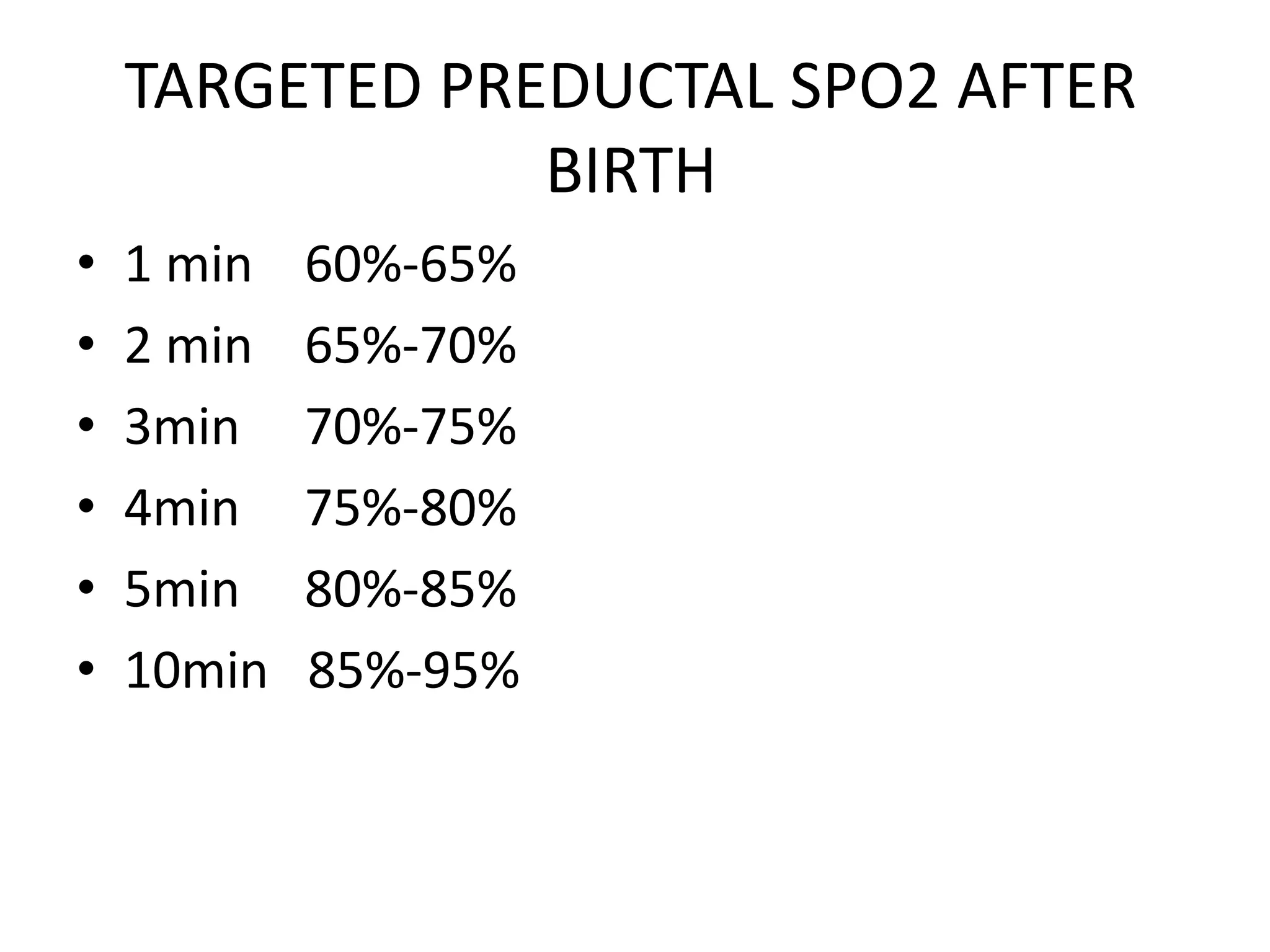
This document summarizes the key points of neonatal resuscitation as presented by Dr. Himanshu Dave. It discusses the history and principles of neonatal resuscitation, the initial steps and assessments of resuscitation, positive pressure ventilation and intubation techniques, chest compressions and medications, special considerations for scenarios like meconium staining and hypothermia treatment, and guidelines for when resuscitation efforts should be stopped. The document provides detailed clinical guidelines and recommendations for neonatal resuscitation based on the latest evidence and standards from organizations like the International Liaison Committee on Resuscitation.