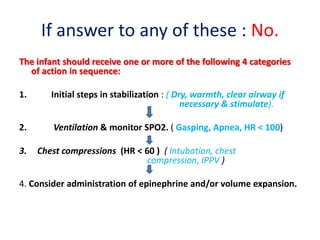
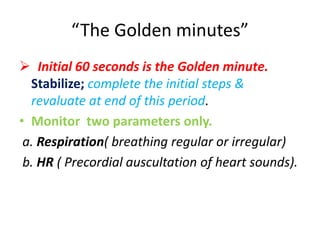
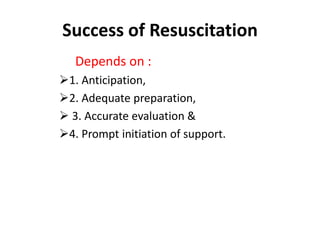
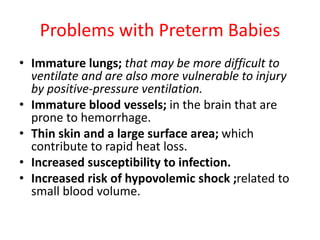
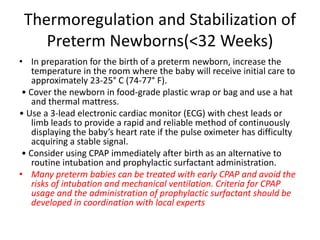
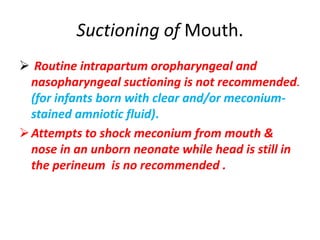
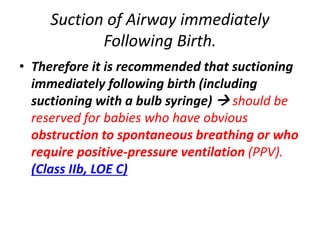
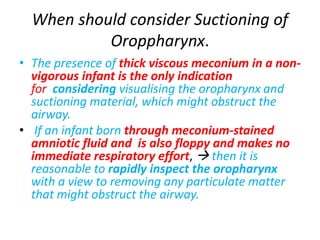
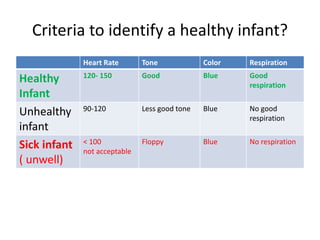
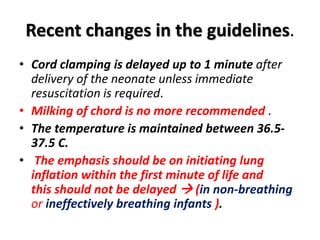
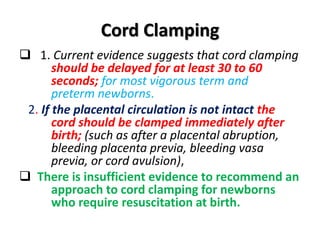
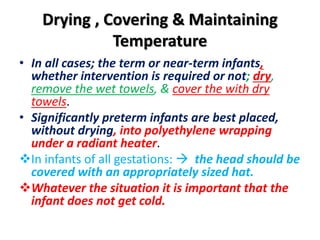
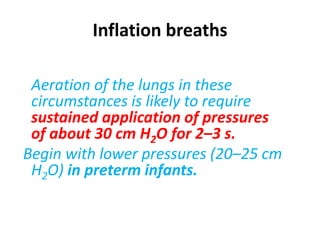
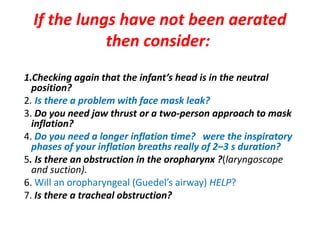
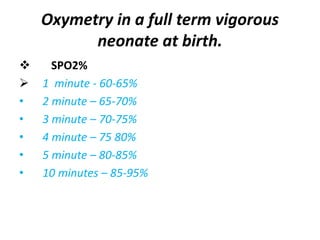
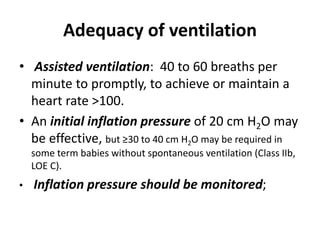
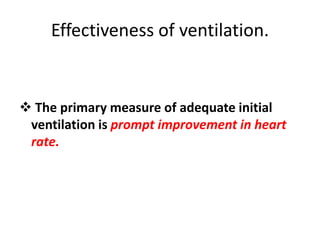
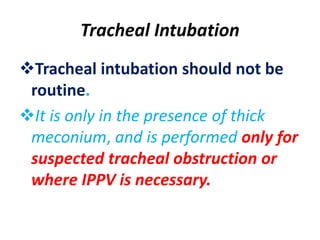
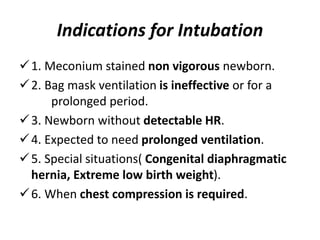
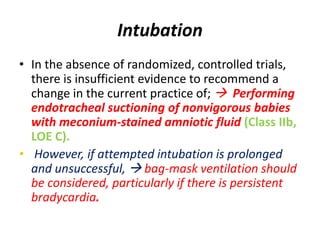
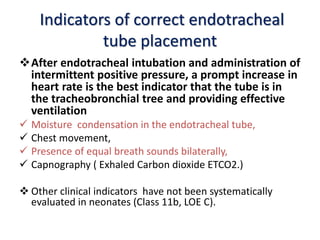
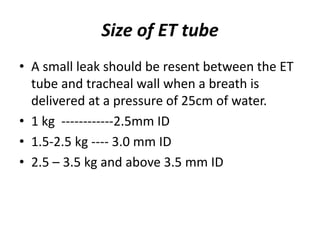
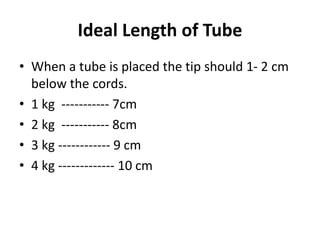
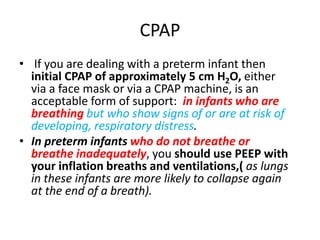
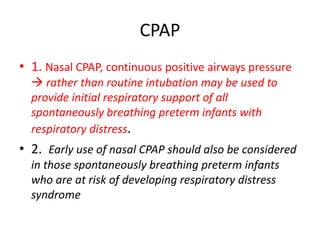
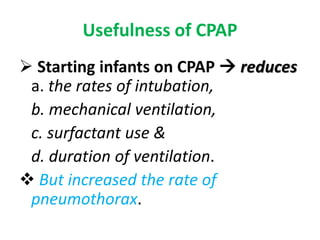
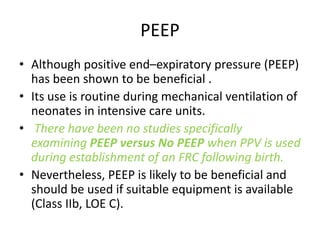
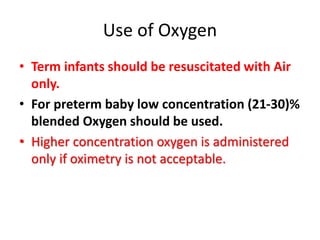
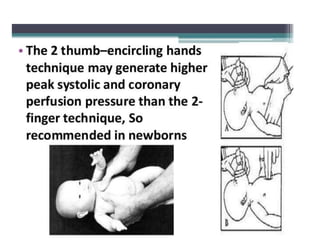
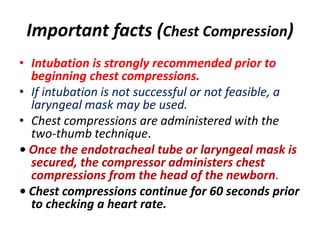
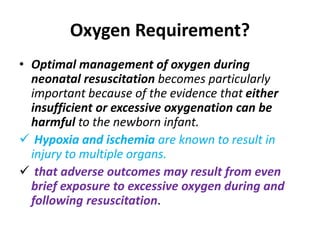
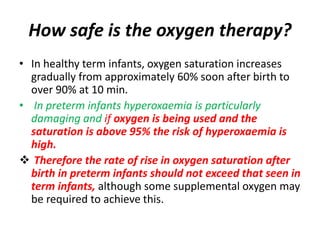
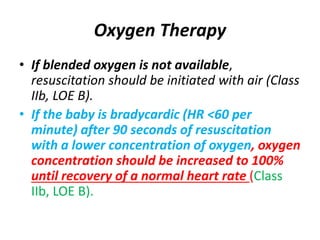
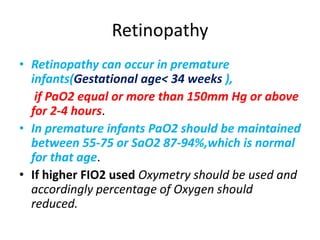
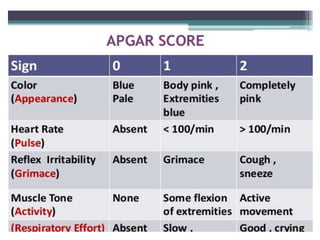
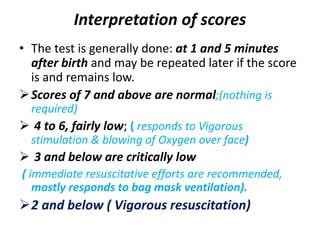
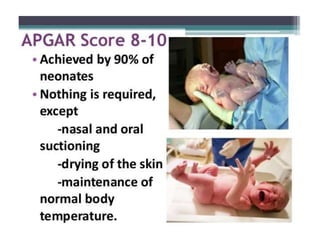
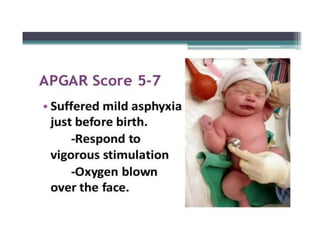
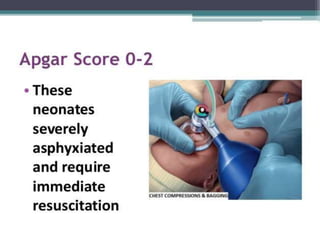
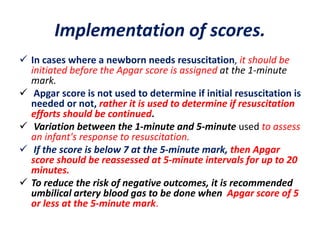
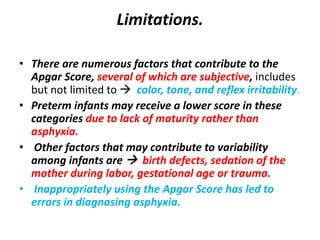
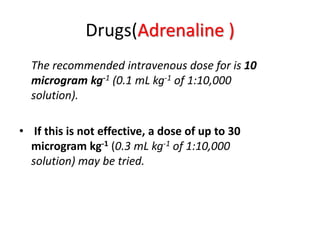
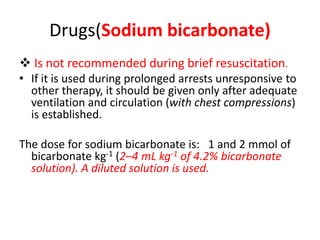
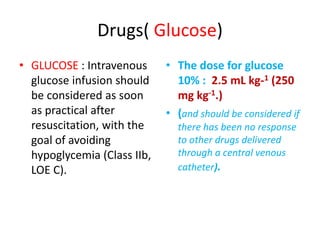
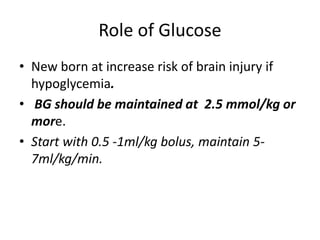
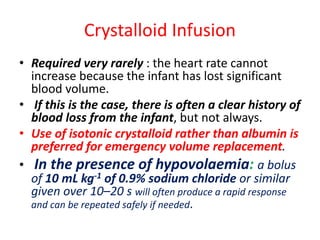
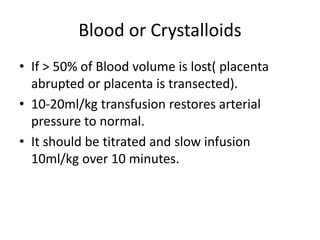
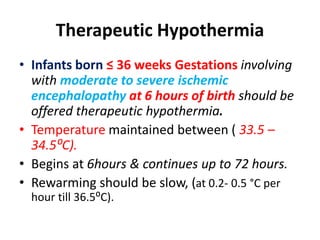
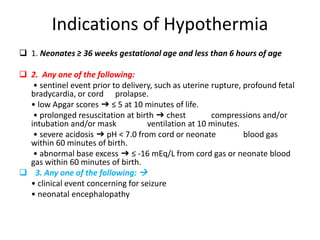
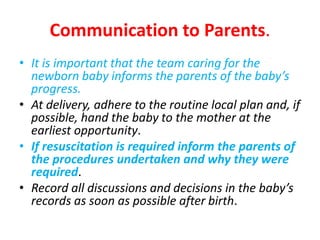
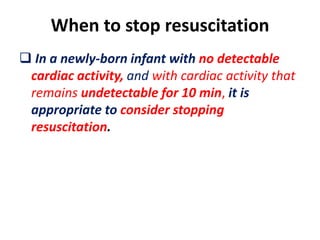
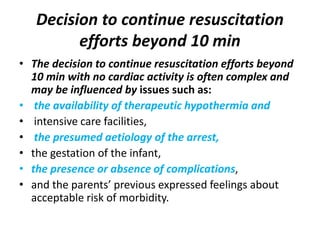
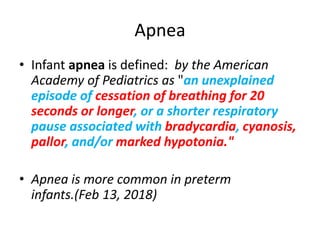
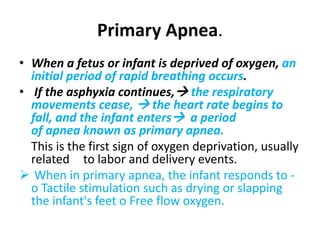
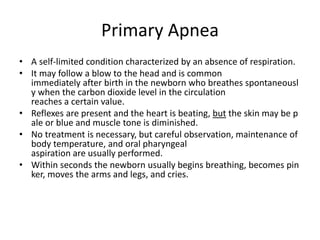
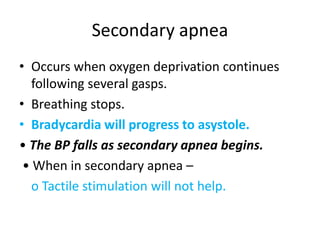
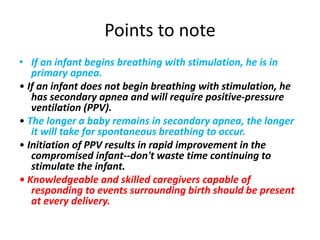
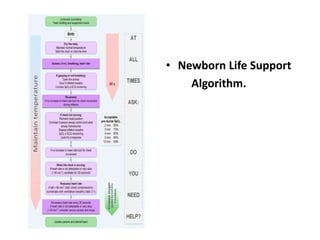
The document provides guidelines for neonatal resuscitation, emphasizing that most newborns require minimal or no intervention. It outlines key steps in assessing the need for resuscitation, initial stabilization procedures, and criteria for managing preterm infants, including using CPAP and avoiding unnecessary suctioning. Additionally, it includes recommendations on oxygen therapy, chest compressions, and post-delivery care to ensure the infant's health and stability.