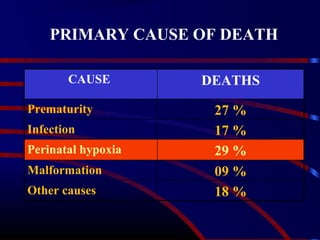
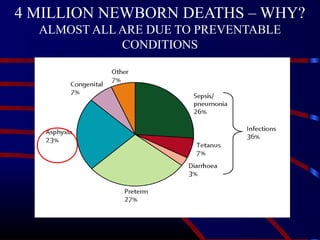
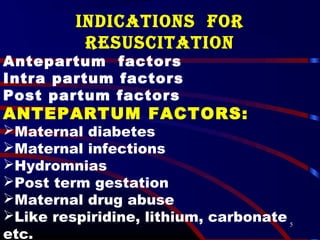
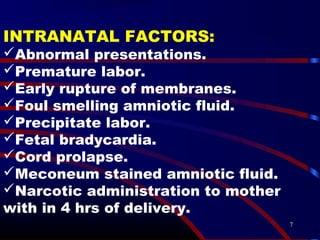
1. Newborn resuscitation is critical to prevent the 4 million newborn deaths that occur annually, nearly all due to preventable conditions like prematurity, infection, and perinatal hypoxia.
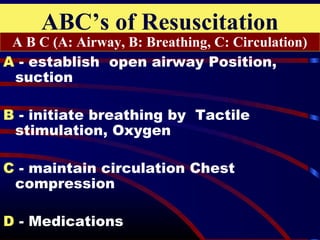
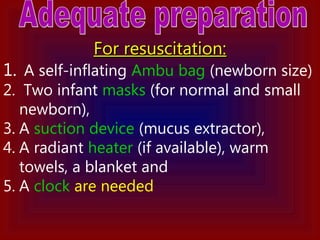
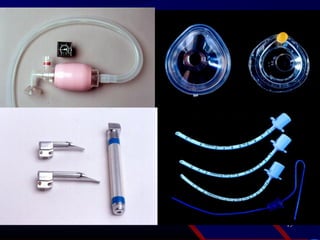
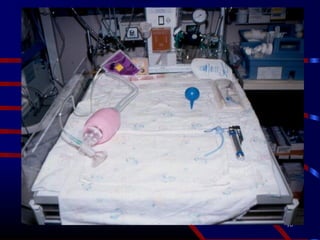
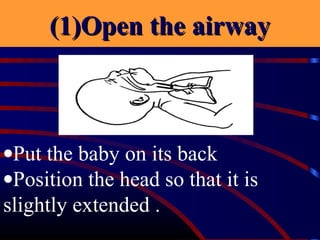
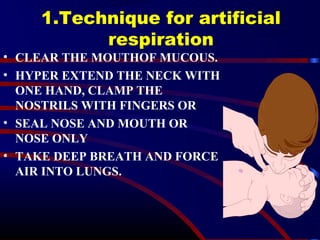
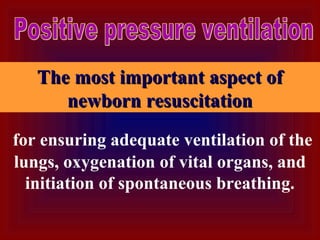
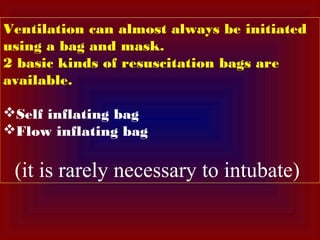
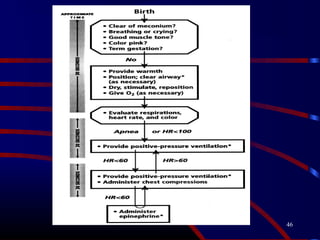
2. Proper newborn resuscitation follows the ABCs - clear the airway, establish breathing, and maintain circulation. It requires anticipating need at every birth and having equipment ready like a self-inflating bag, masks, and suction device.
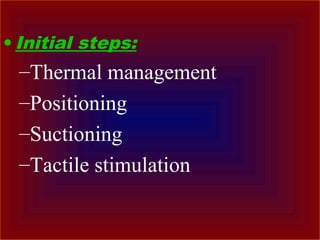
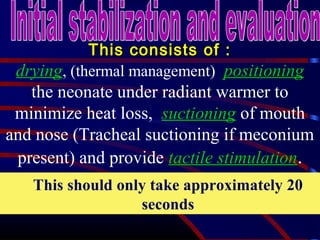
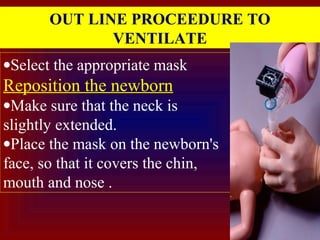
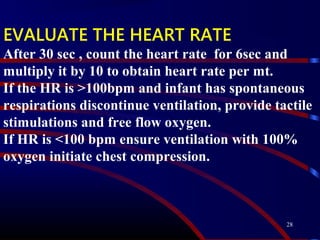
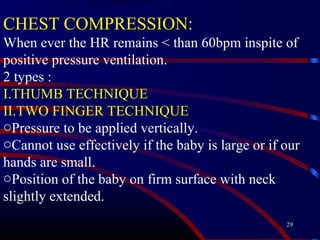
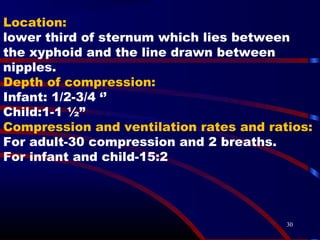
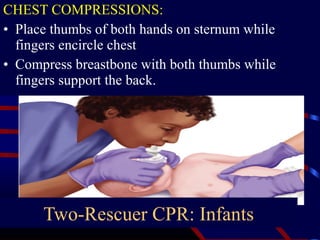
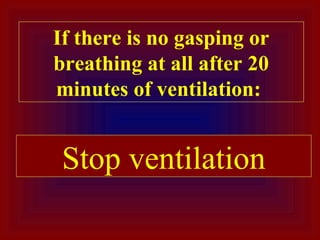
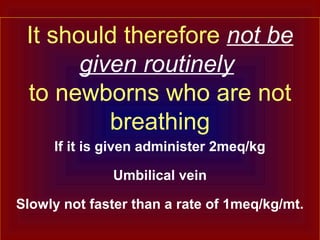
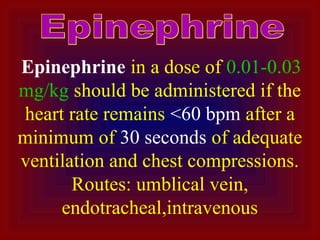
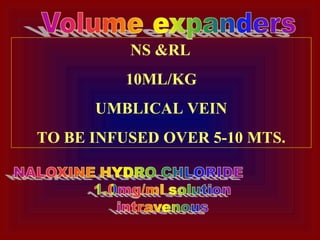
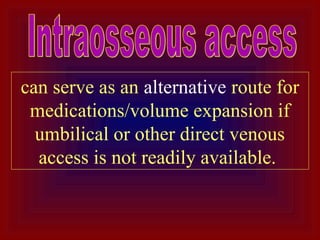
3. Steps include drying, positioning, suctioning if needed, and tactile stimulation followed by ventilation if not breathing. If the heart rate is slow, initiate chest compressions and provide medications like epinephrine if needed. Maintaining