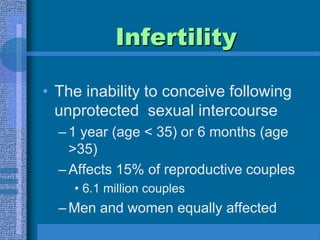
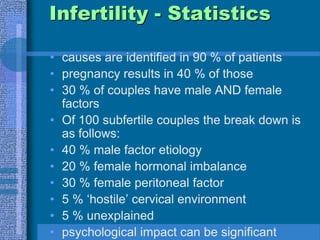
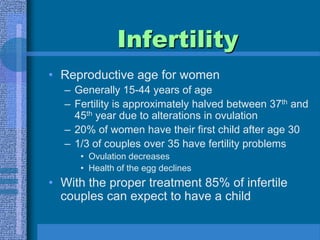
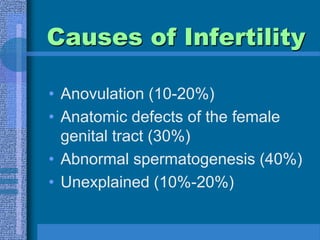
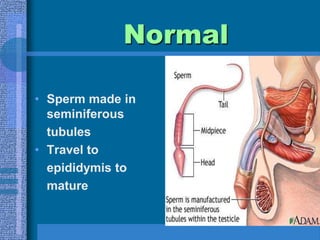
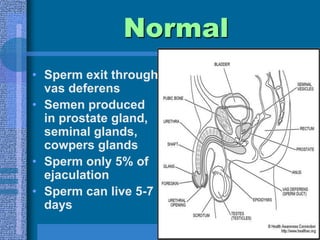
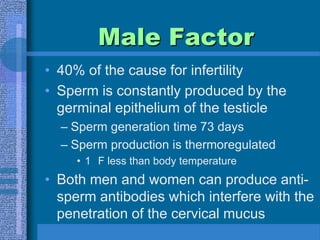
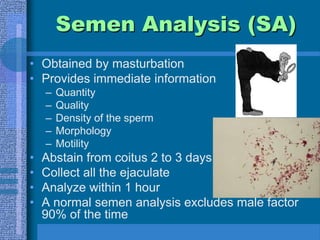
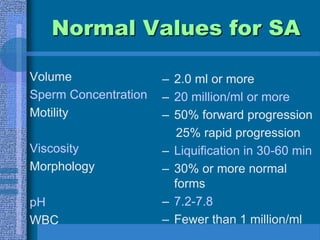
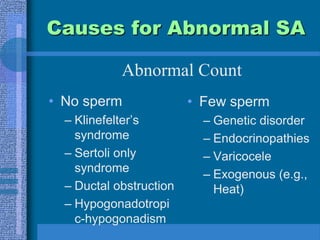
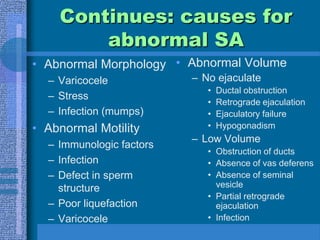
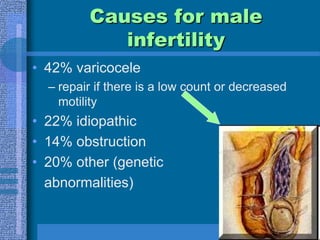
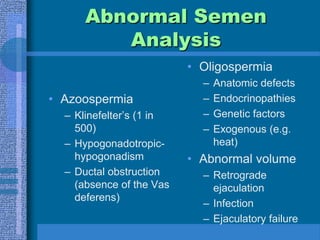
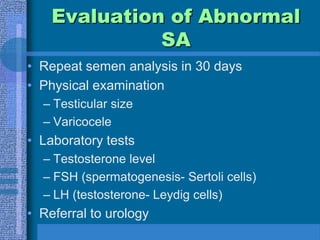
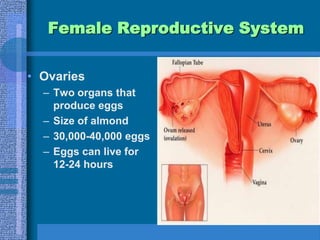
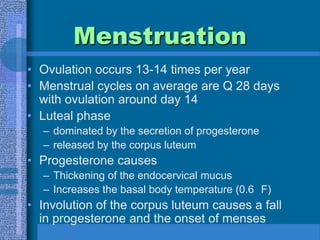
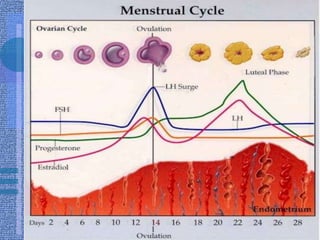
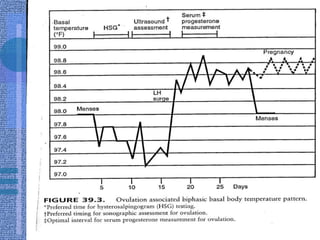
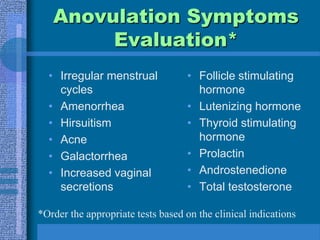
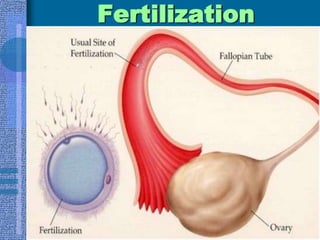
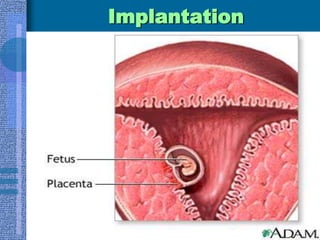
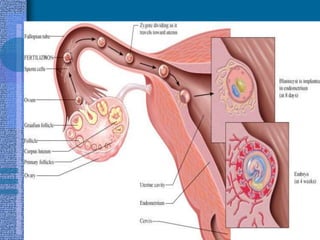
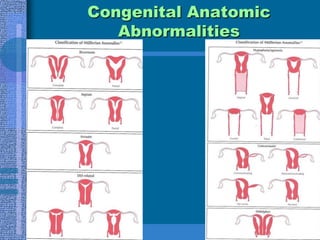
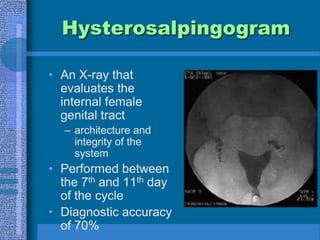
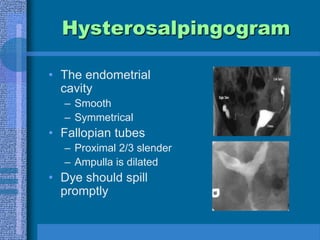
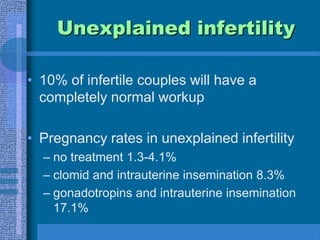
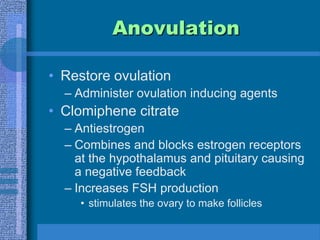
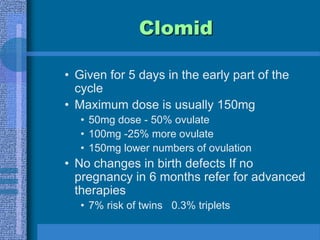
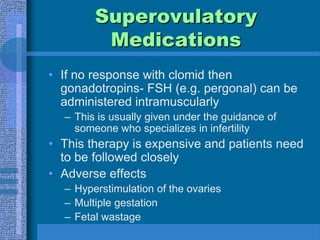
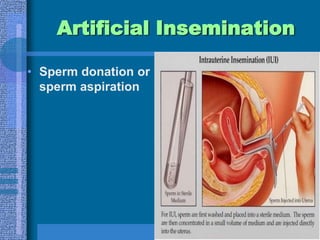
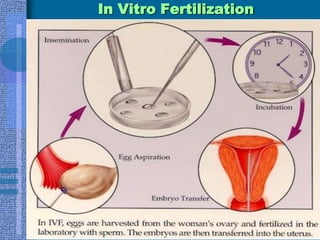
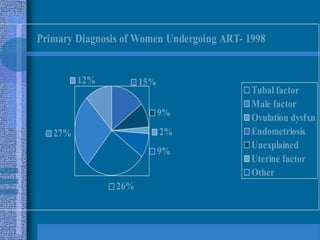
This document discusses infertility, including its definition, causes, evaluation, and treatment options. It begins by defining primary and secondary infertility and outlining the requirements for conception. Common causes of infertility for both men and women are then described. The document provides details on evaluating infertility, including medical history, physical exams, lab tests, and procedures like semen analysis and hysterosalpingography. Treatment options are covered, such as ovulation induction, surgery, assisted reproductive technologies like IUI, IVF, and surrogacy. The emotional impact of infertility is also addressed.