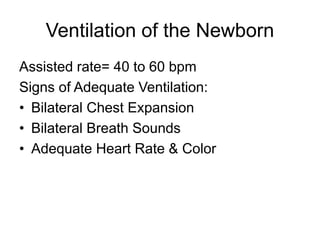
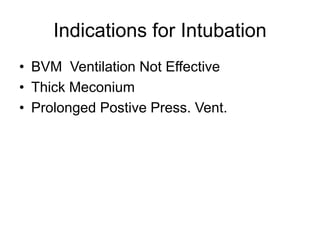
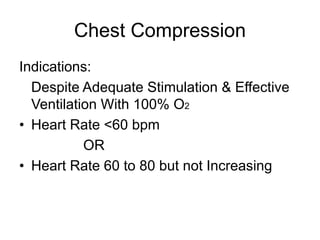
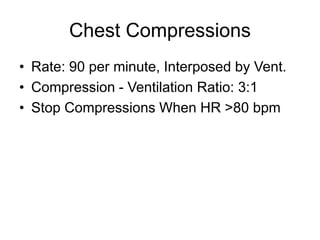
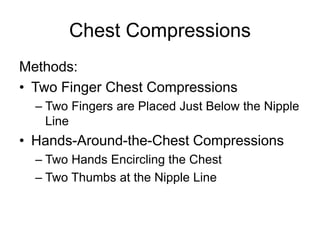
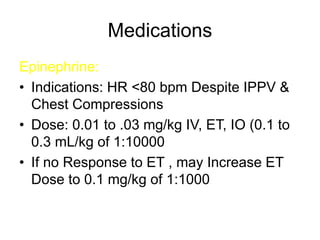
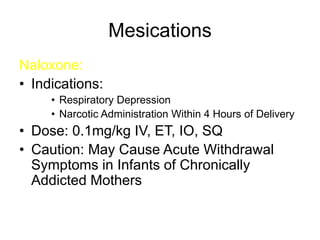
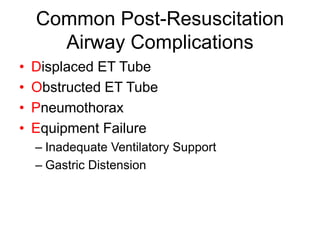
This document discusses neonatal resuscitation and care. It begins by defining a neonate and outlining the rapid physiological changes that must occur for an infant to transition from intrauterine to extrauterine life. It then describes the risks for neonatal difficulties at birth and outlines the priorities, equipment, and techniques for resuscitation. These include providing oxygen, ventilation, chest compressions, and medications as needed. The document concludes by discussing components of initial routine neonatal care like screening, physical assessment, prophylaxis, encouraging parent-infant interaction, and preventing heat loss.