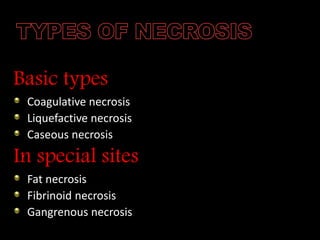
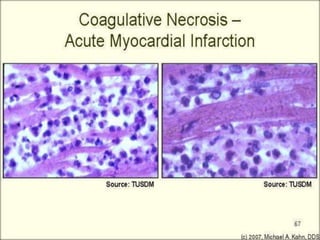
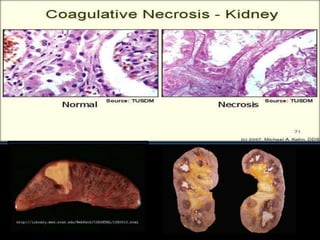
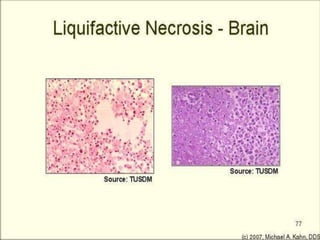
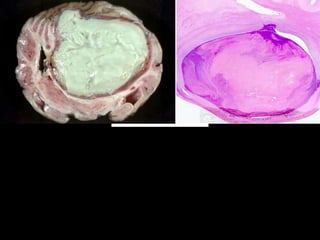
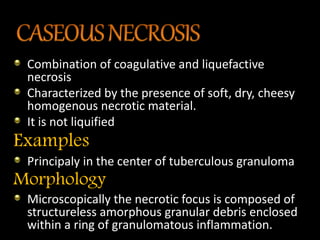
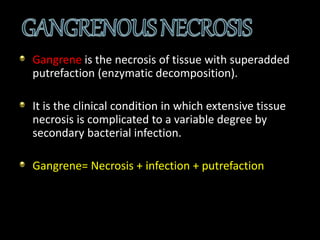
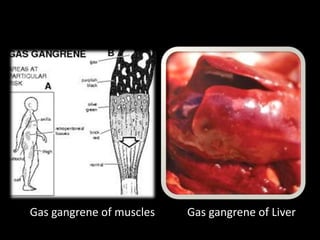
Necrosis begins with cell impairment and loss of homeostasis, leading to cell death. There are several types of necrosis including coagulative, liquefactive, and caseous. Coagulative necrosis preserves cell structure while liquefactive and caseous necrosis involve enzymatic degradation and liquification/softening of tissue. Gangrene involves extensive tissue necrosis complicated by secondary bacterial infection and putrefaction.