Embed presentation
Download as PDF, PPTX


























Necrosis is the morphologic changes that follow cell death in living tissues. It can be caused by ischemia, physical agents, chemical agents, or immunological injury. The main types of necrosis include coagulative necrosis, liquefactive necrosis, caseous necrosis, fat necrosis, and fibrinoid necrosis. Coagulative necrosis preserves tissue architecture with denatured proteins and enzymatic digestion of cells. Liquefactive necrosis results in a liquid viscous mass. Caseous necrosis is a type of coagulative necrosis seen in tuberculosis that leaves cheesy white tissue.
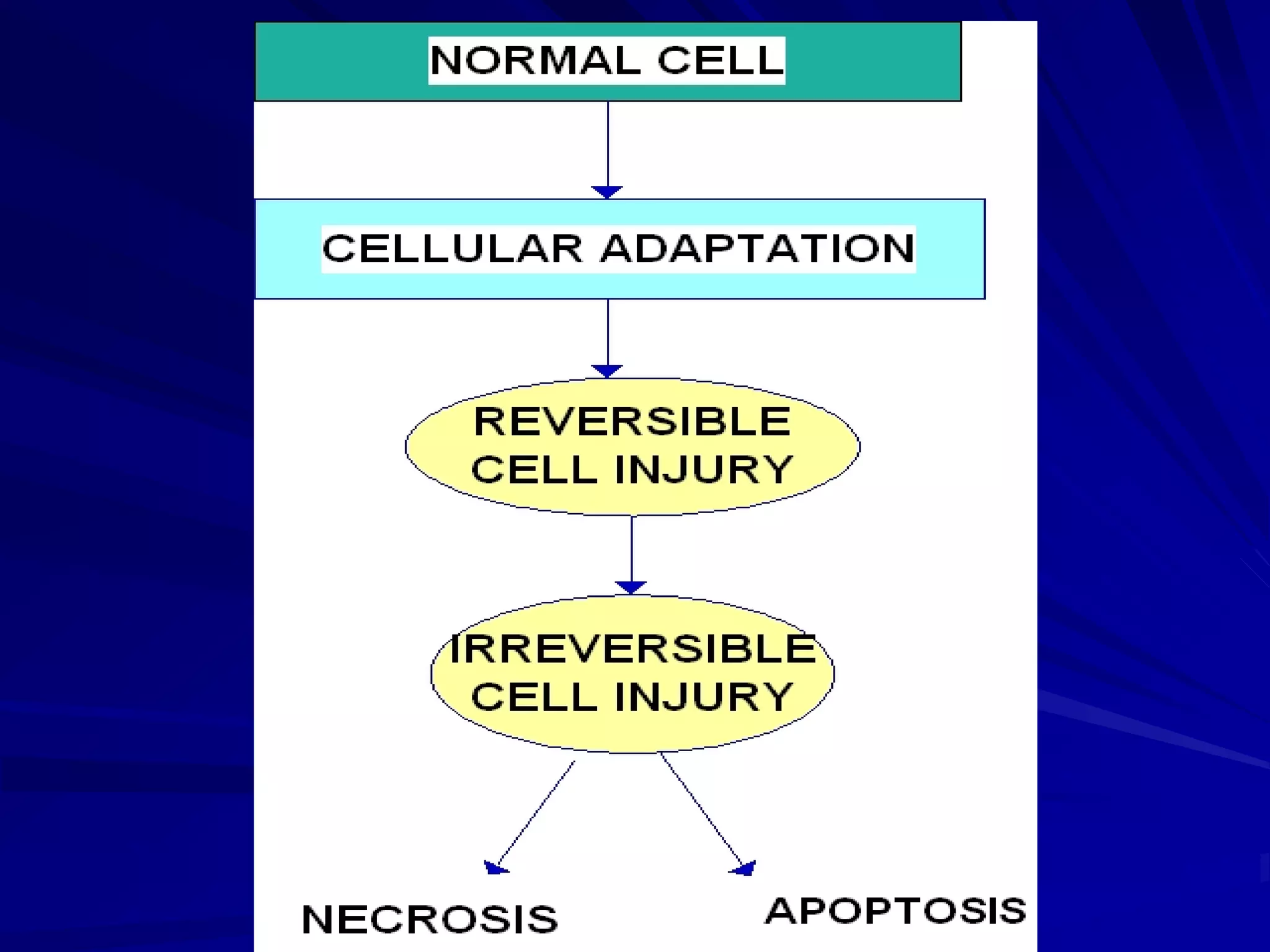
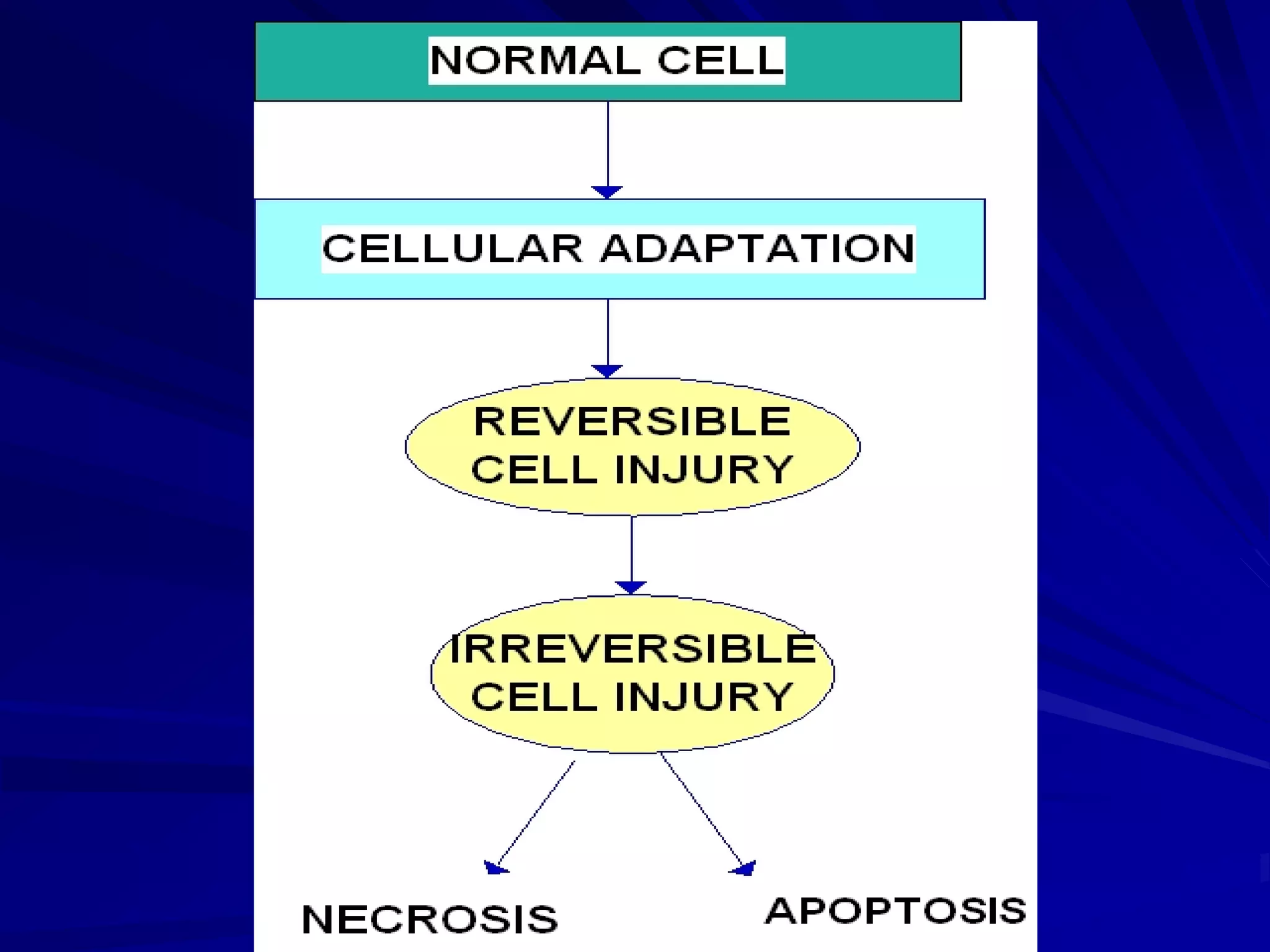
Definition of necrosis as changes following cell death, with causes including ischemia and immunological injuries.
Pathogenesis includes protein denaturation and cell digestion; morphology involves cytoplasmic and nuclear changes.
Classification of necrosis into seven types including coagulative, liquefactive, and caseous necrosis.
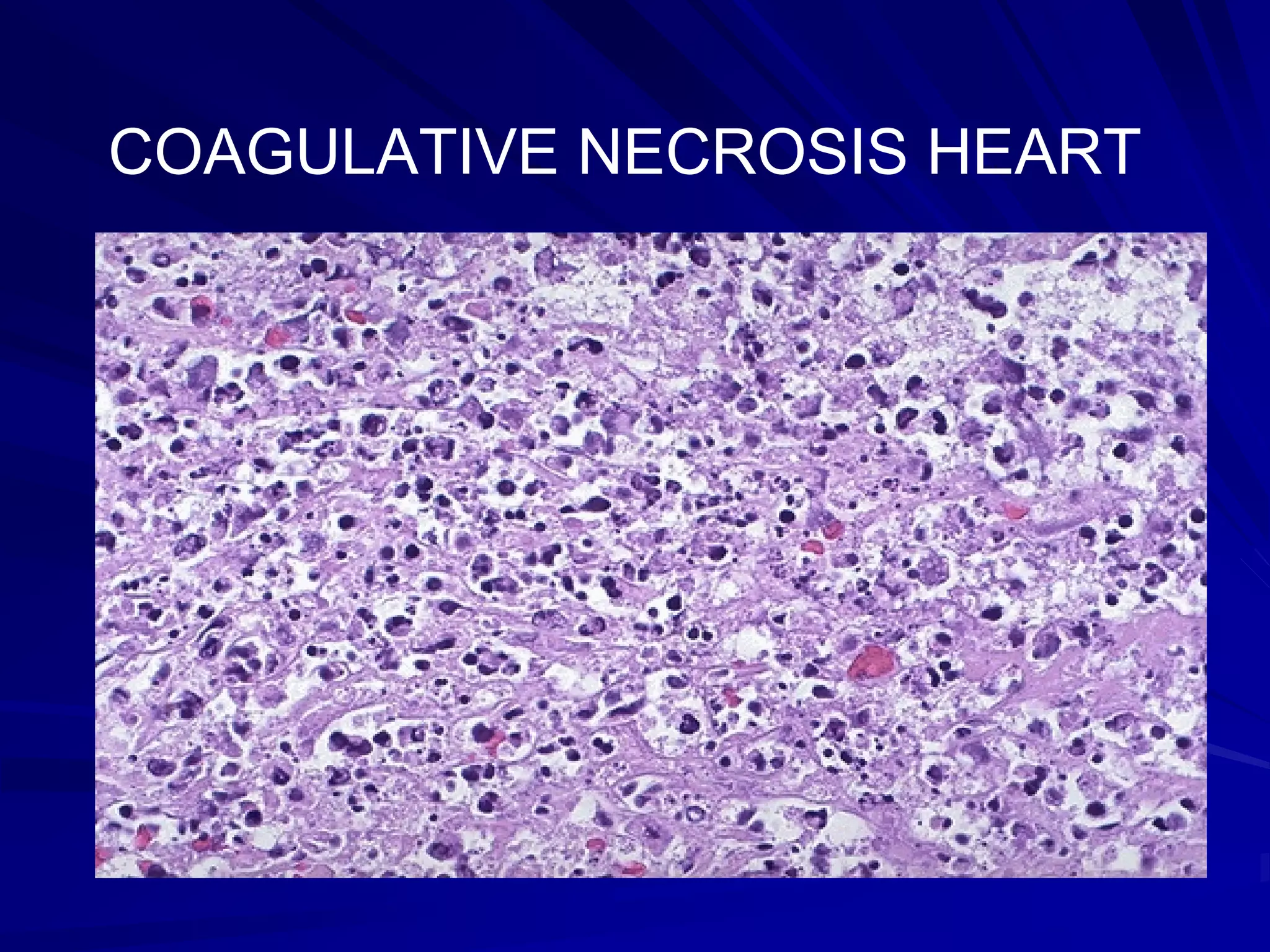
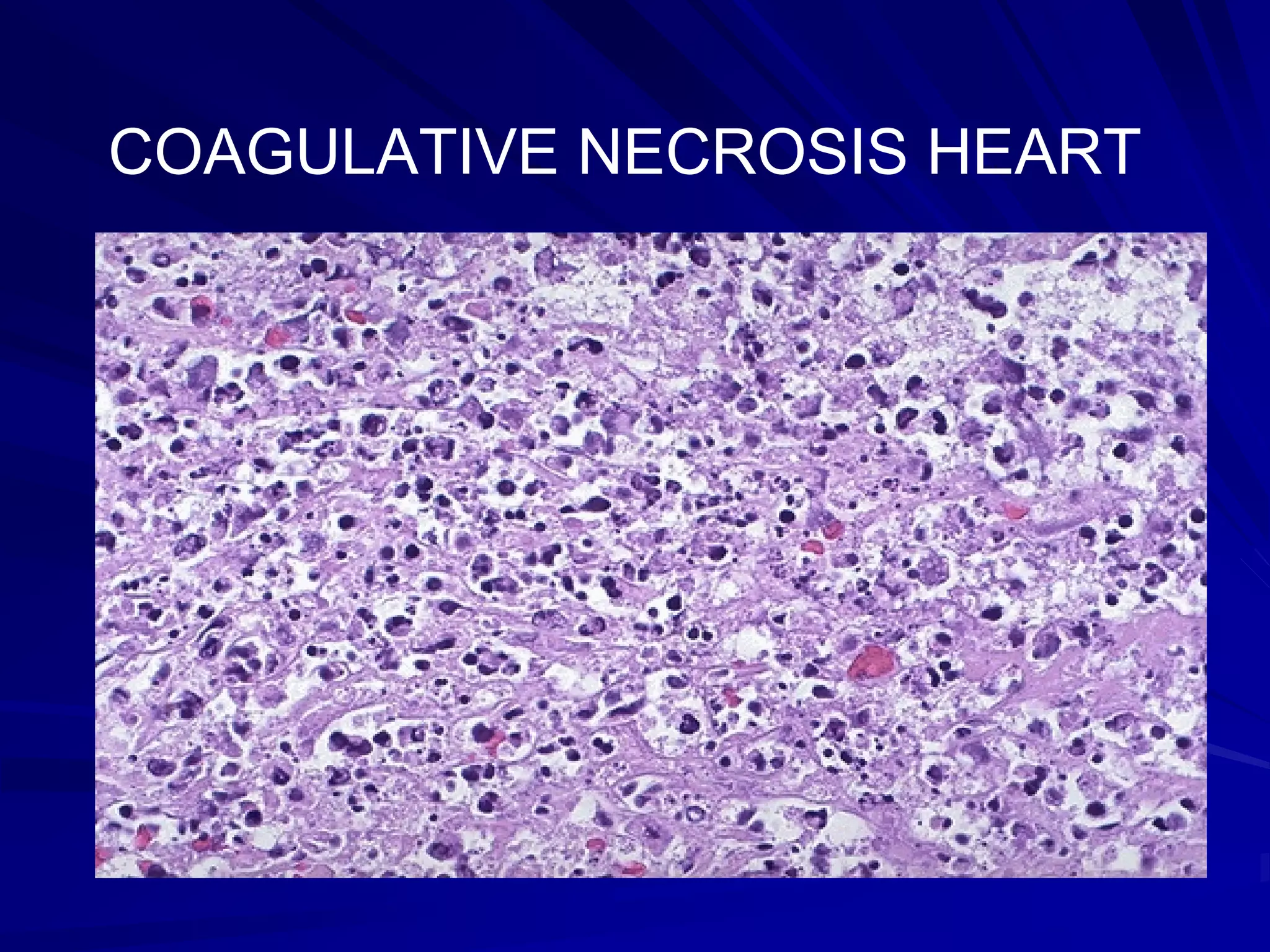
Coagulative necrosis features firm tissue, preserved architecture, and examples in heart and kidney.
Liquefactive necrosis results in a viscous mass, often seen in the brain and abscess formations.
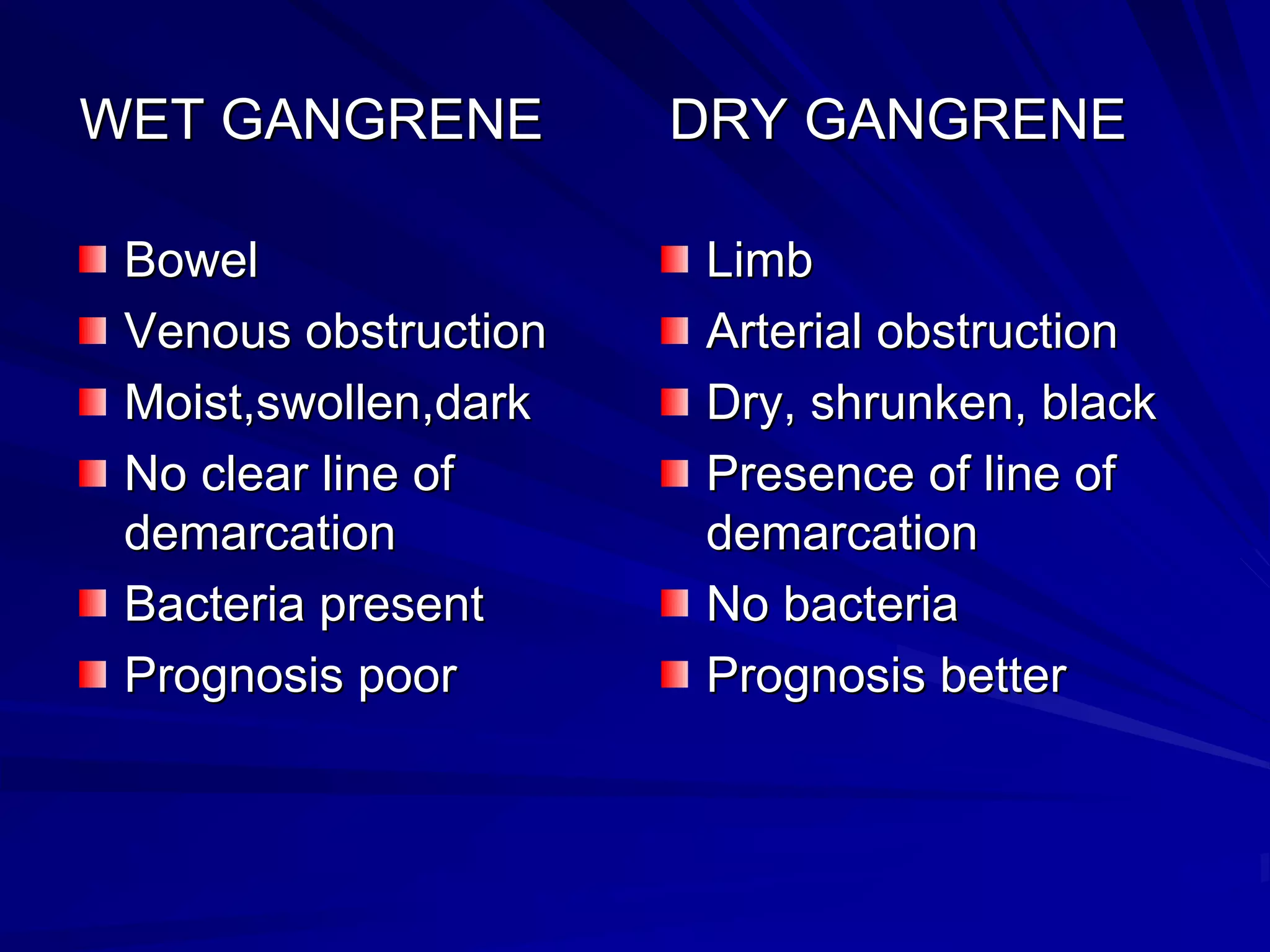
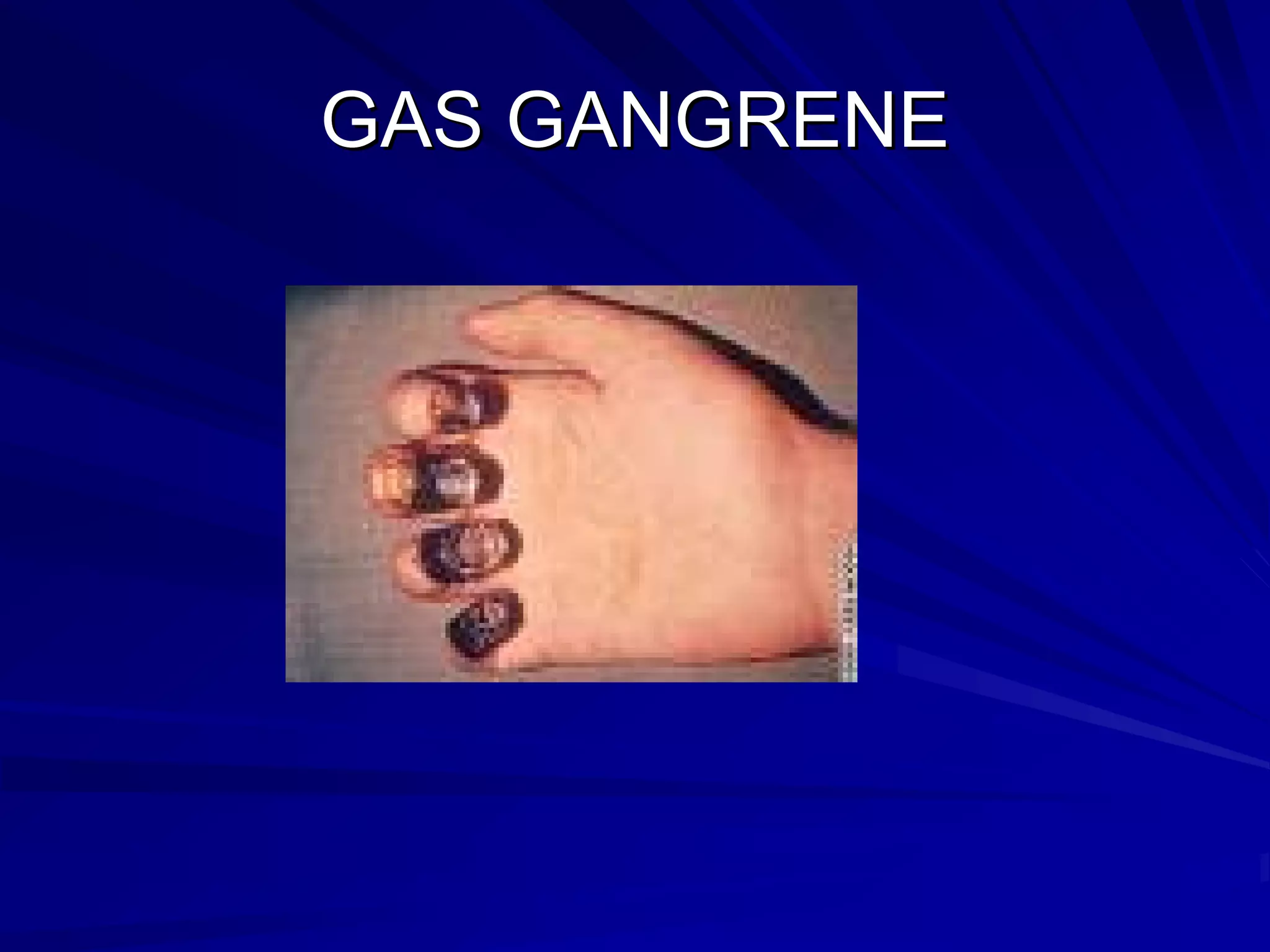
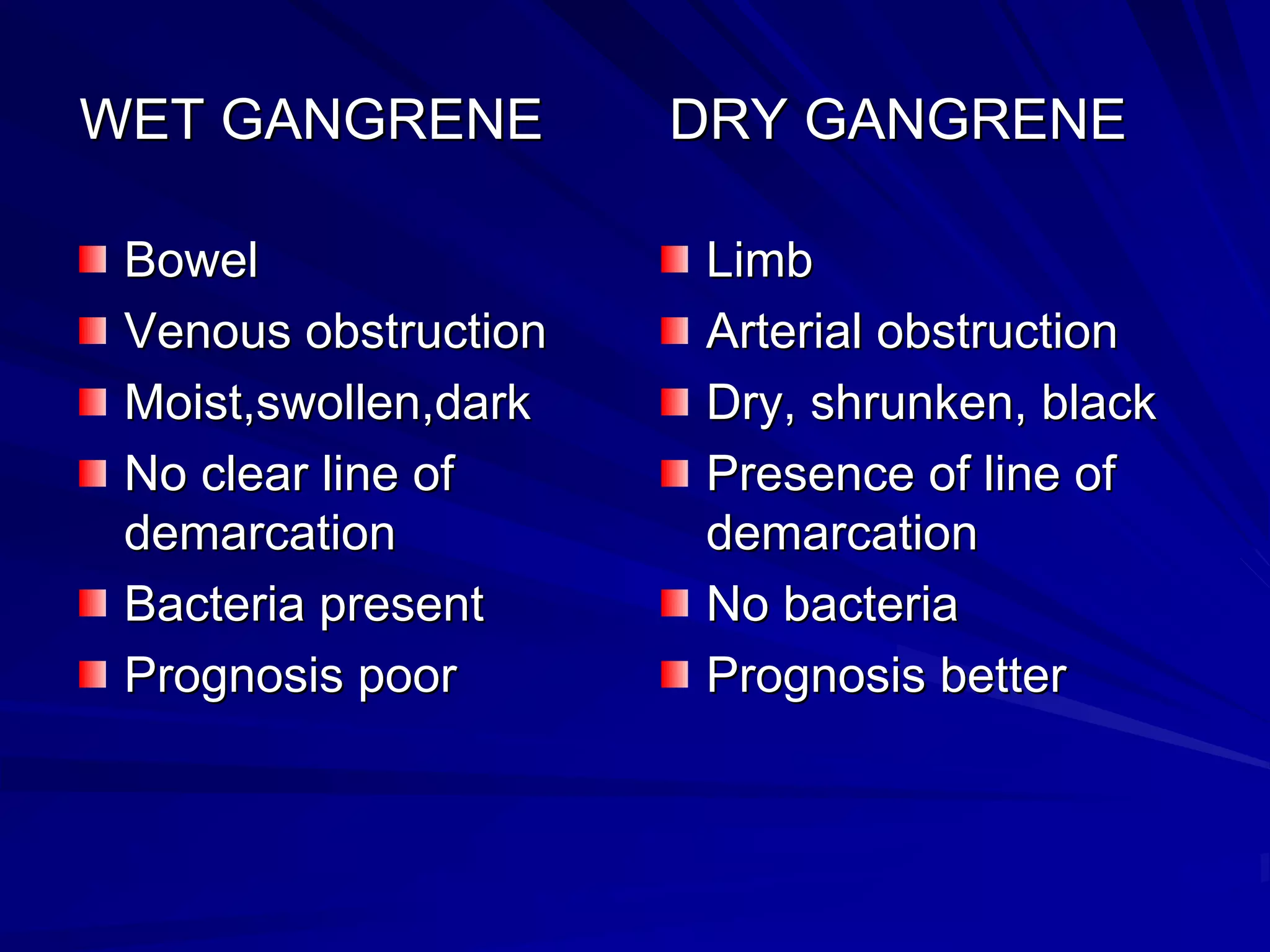
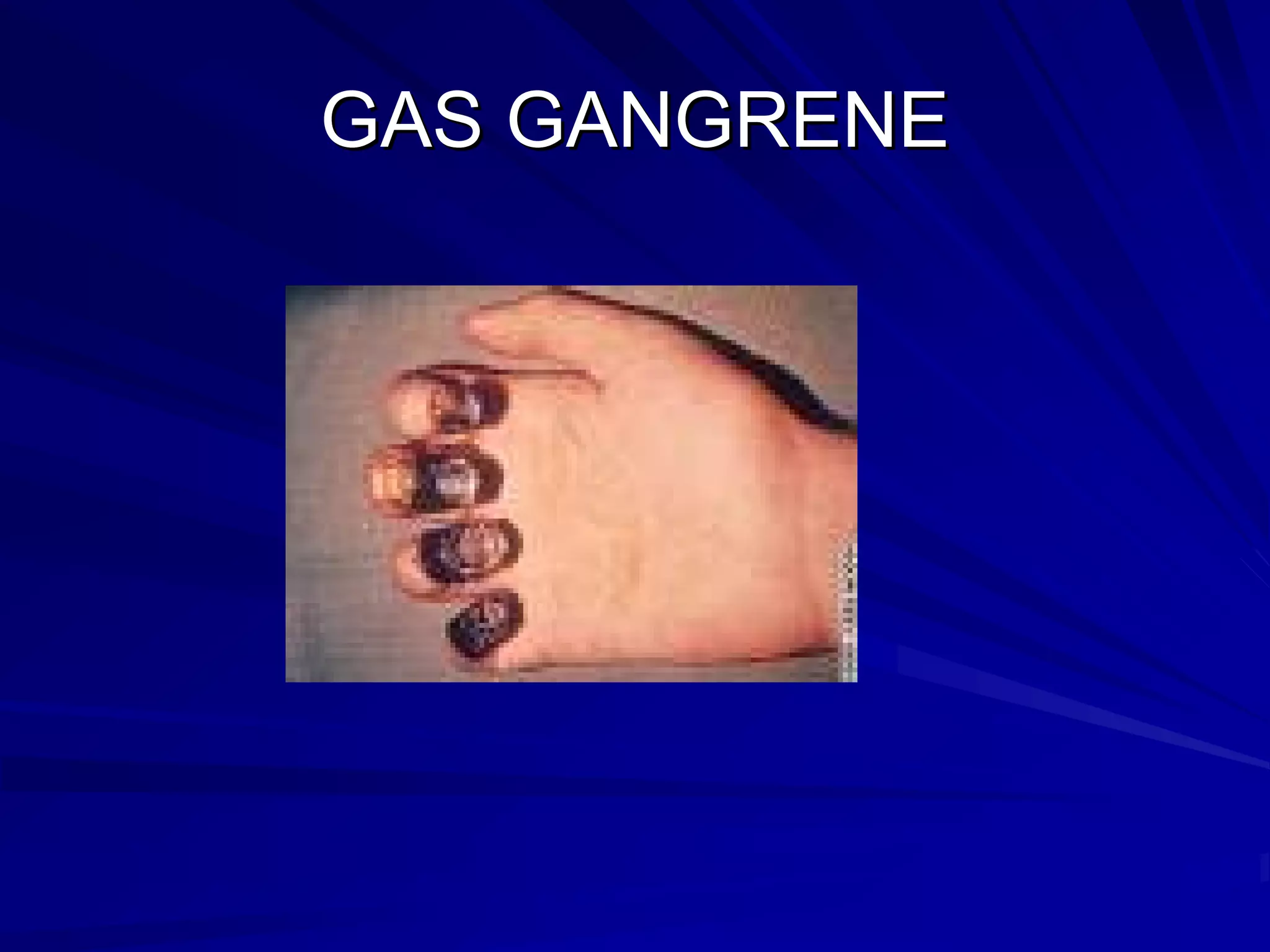
Gangrenous necrosis includes wet, dry, and gas gangrene, with specific examples and characteristics.
Wet gangrene occurs in moist tissues like intestines, associated with conditions like diabetic foot.
Dry gangrene affects toes due to arterial issues, with marked features of dryness and better prognosis.
Gas gangrene is caused by anaerobic bacteria in moist tissue, notably within muscles and colon.
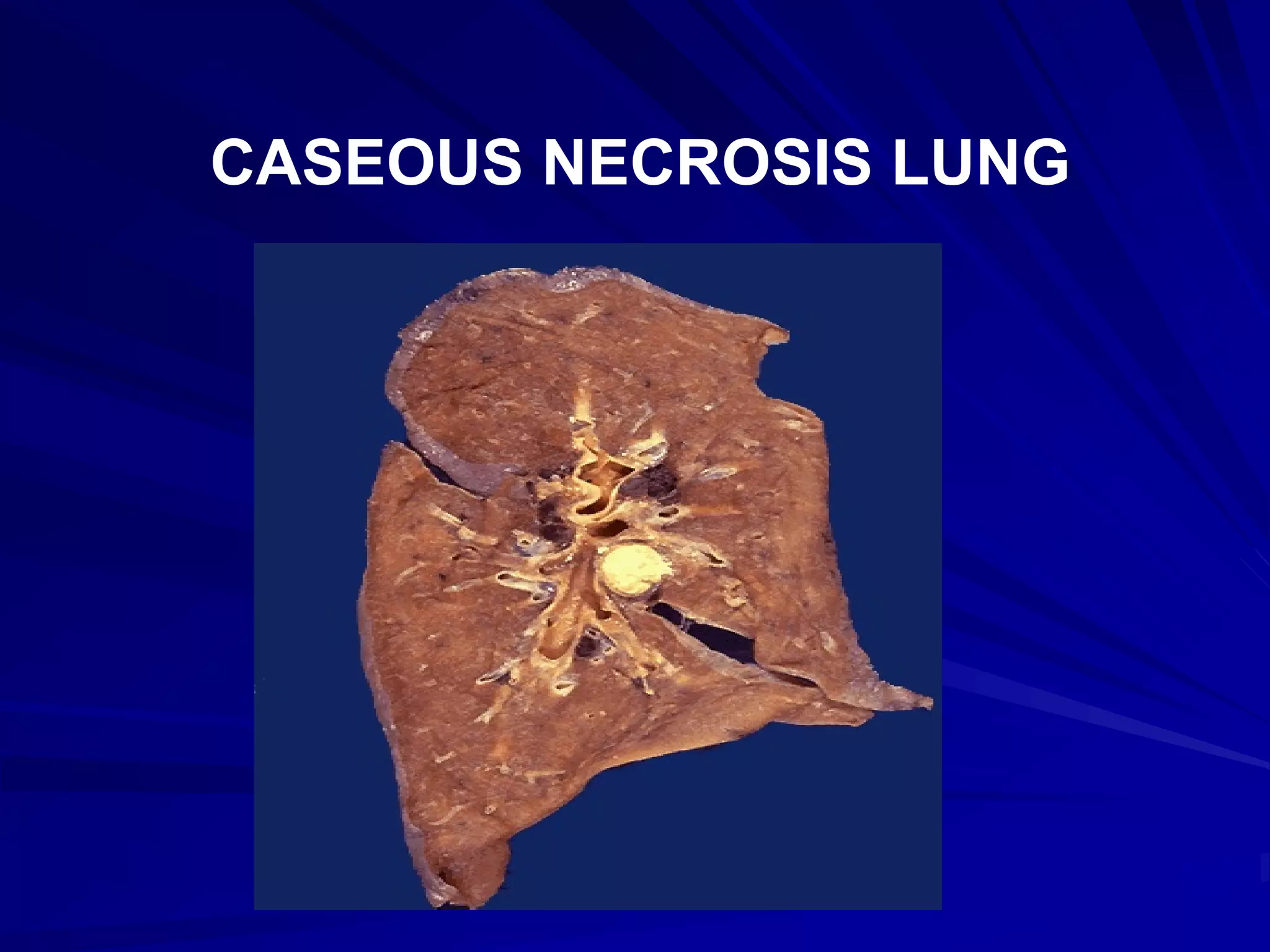
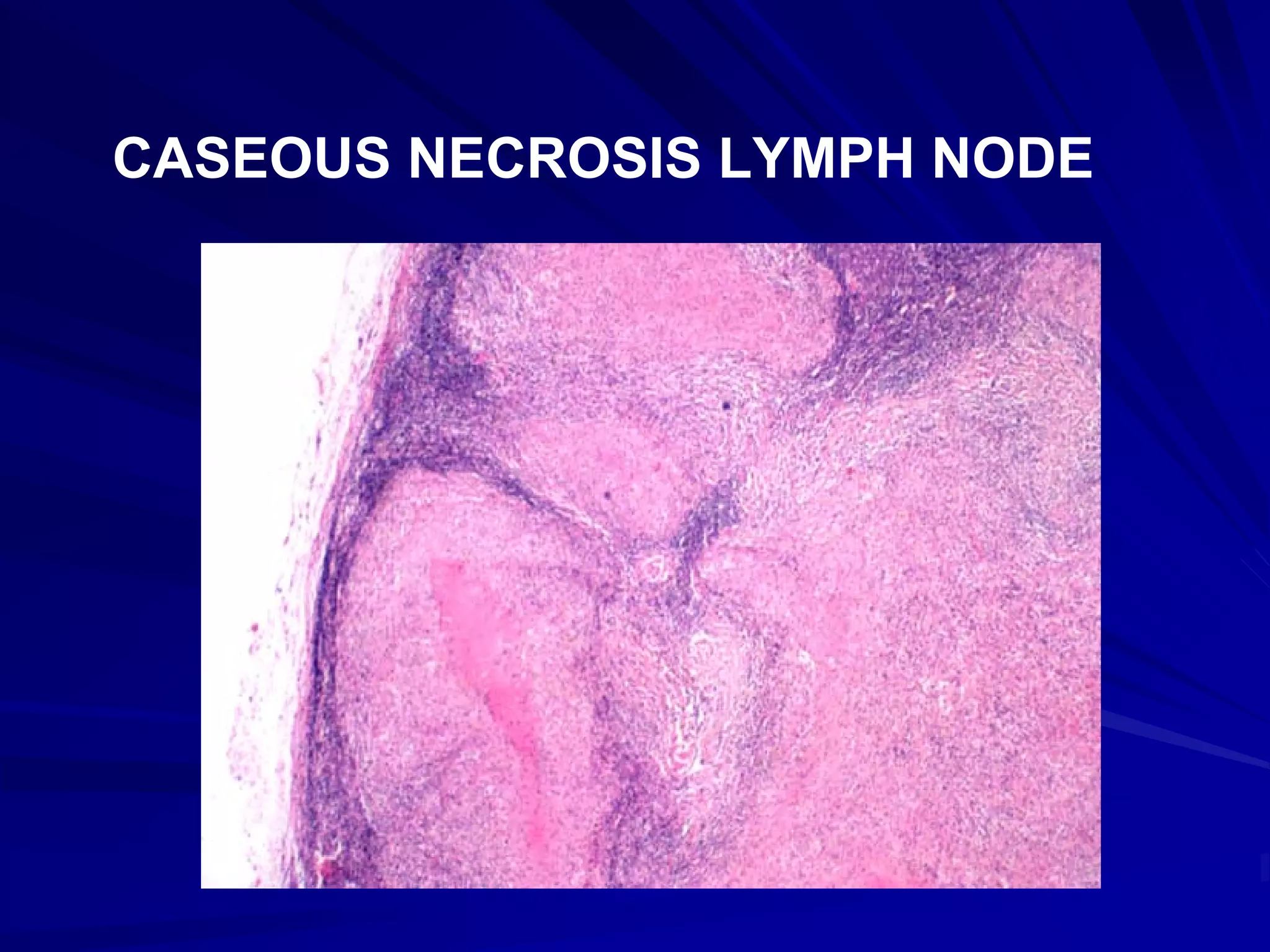
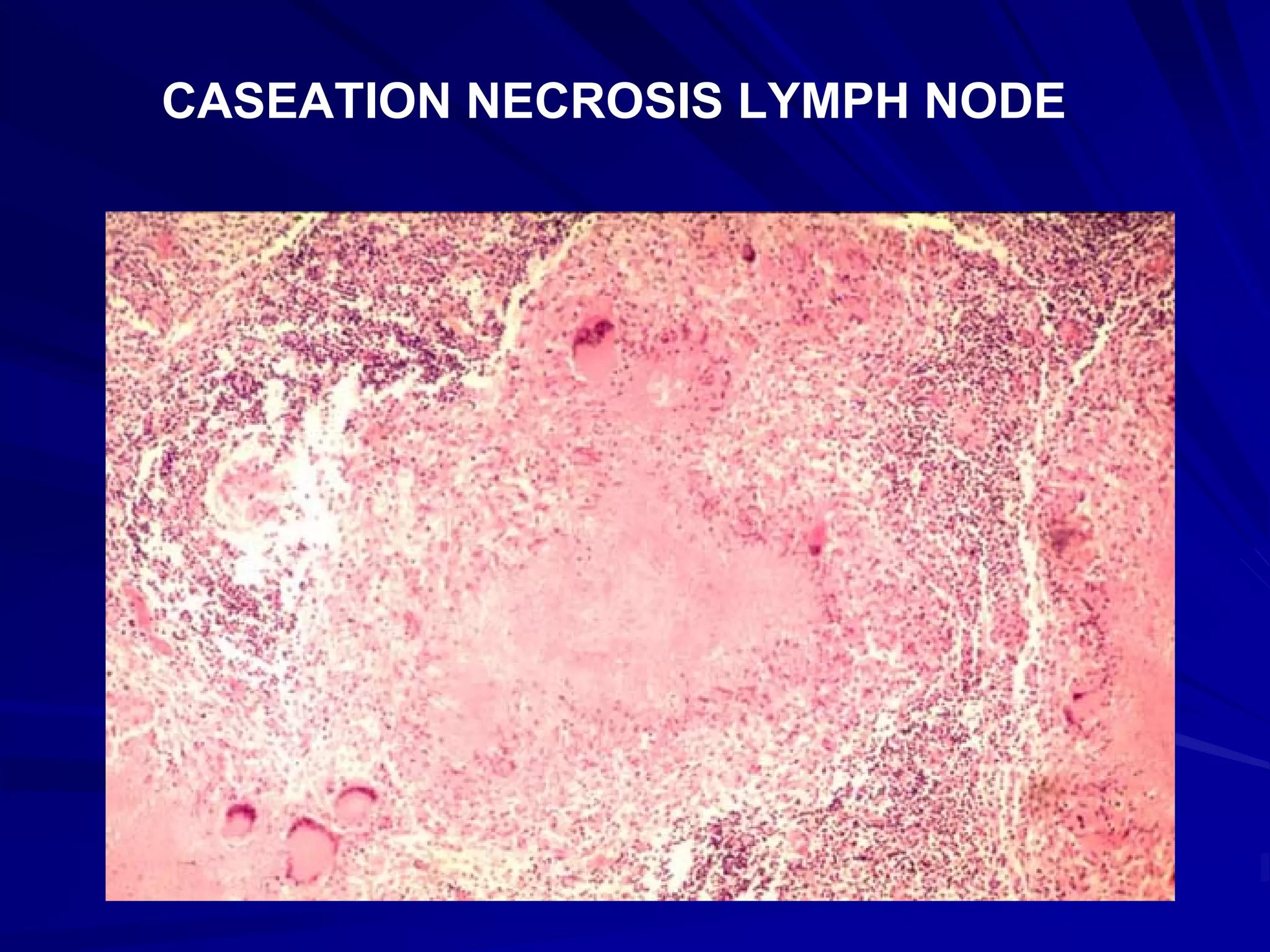
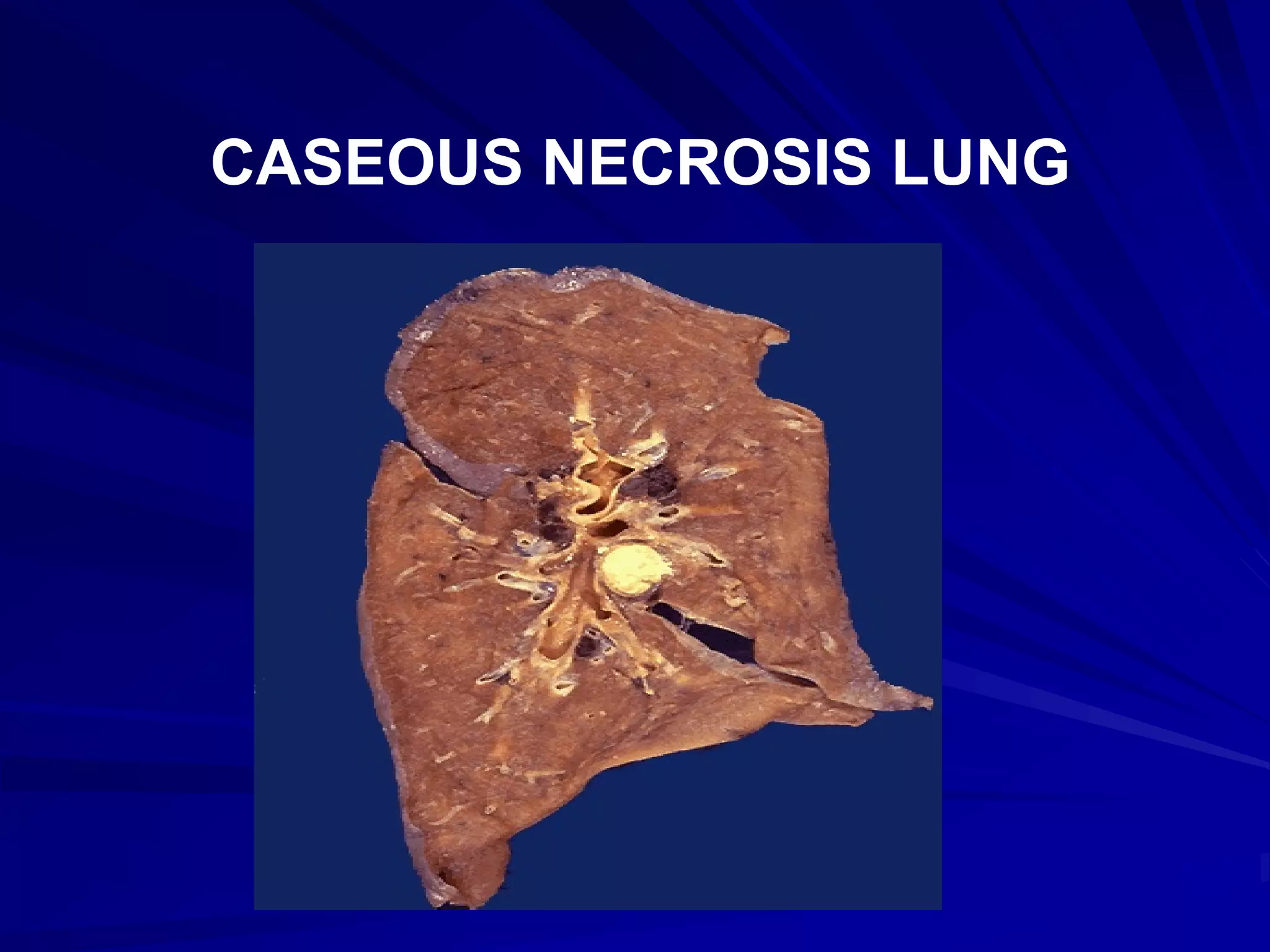
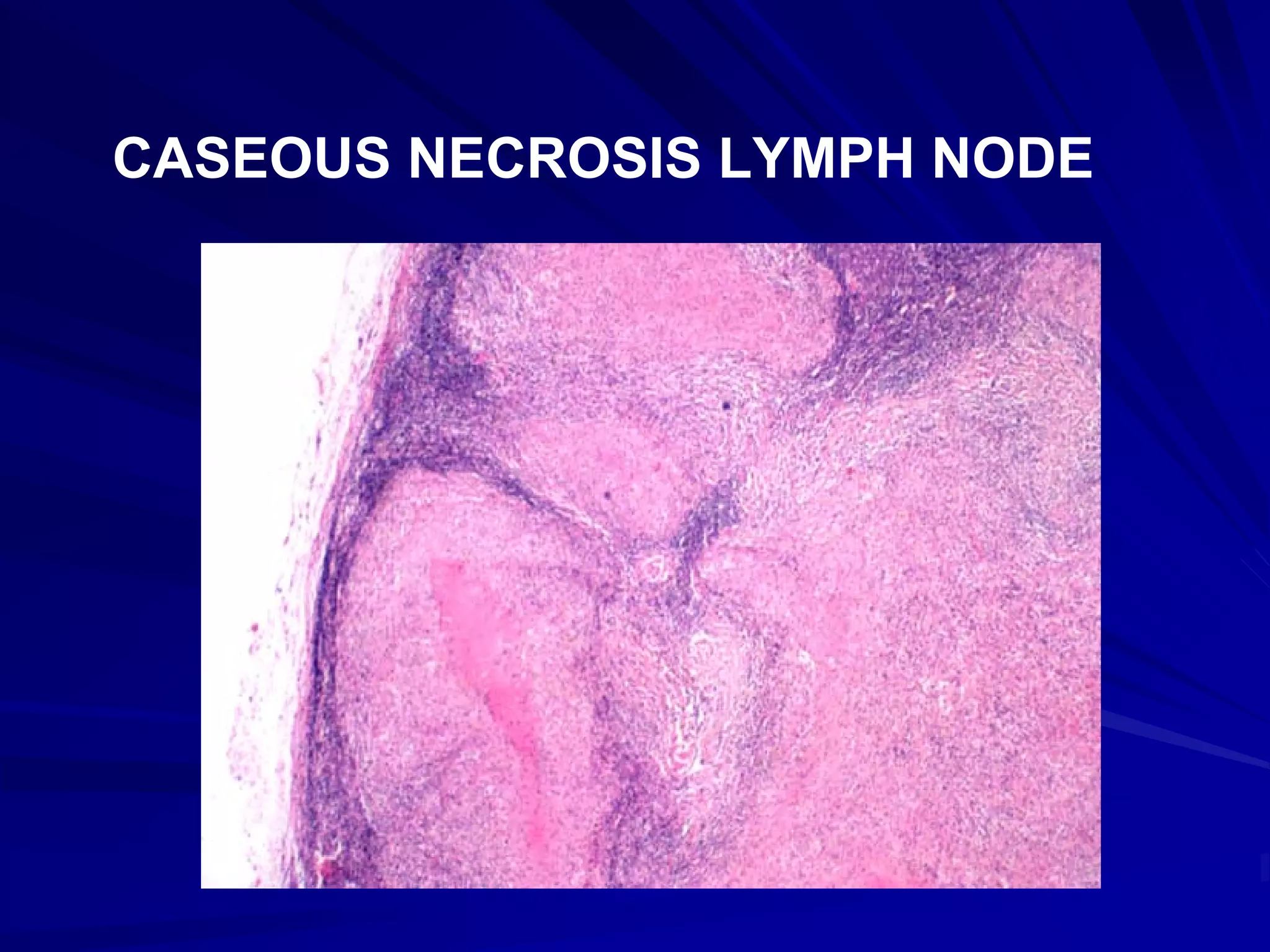
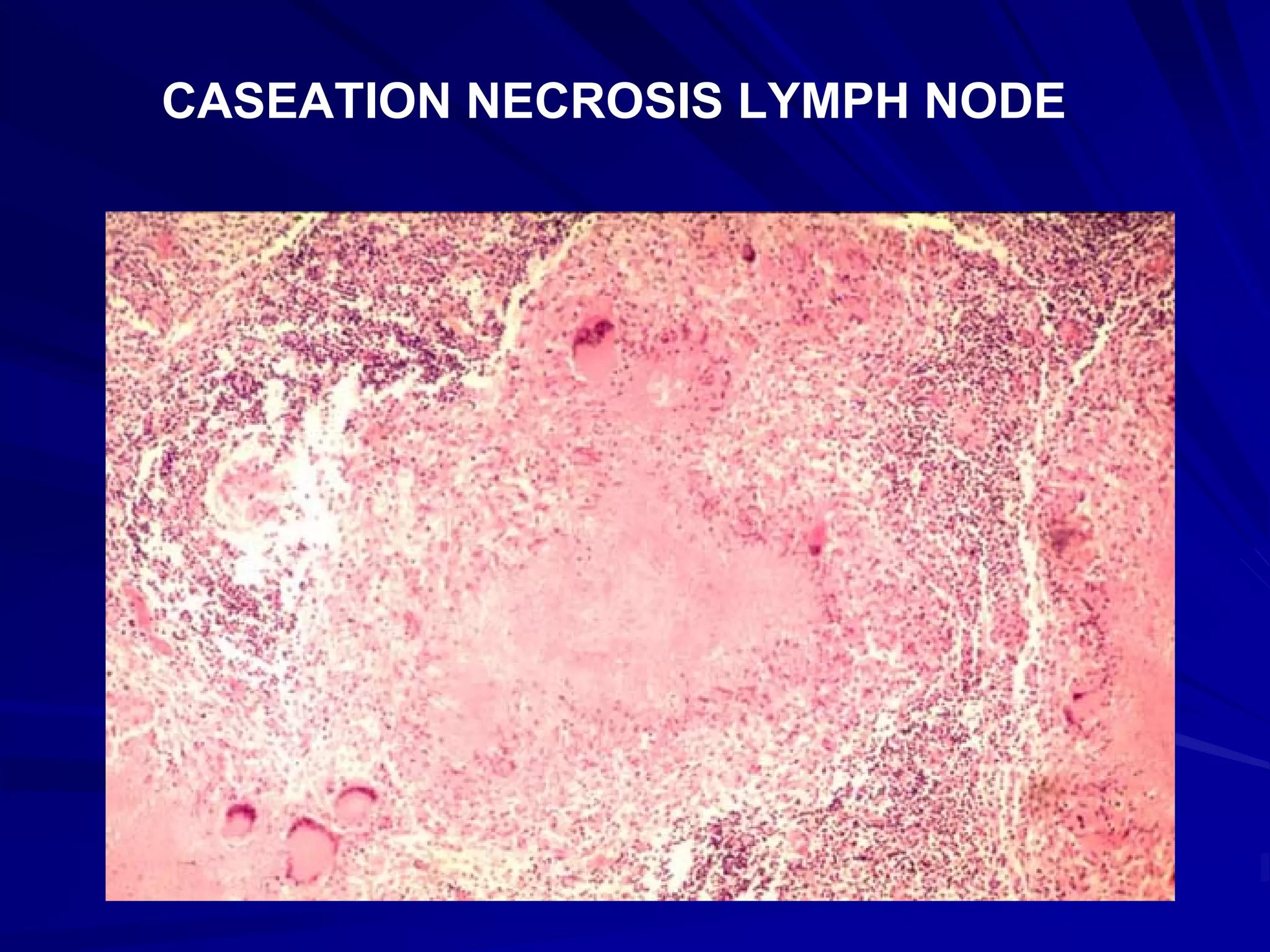
Caseous necrosis resembles coagulative necrosis but is associated with tuberculosis, showing cheesy appearance.
Caseous necrosis visuals in lung and lymph nodes illustrate architecture preservation with cheesy texture.
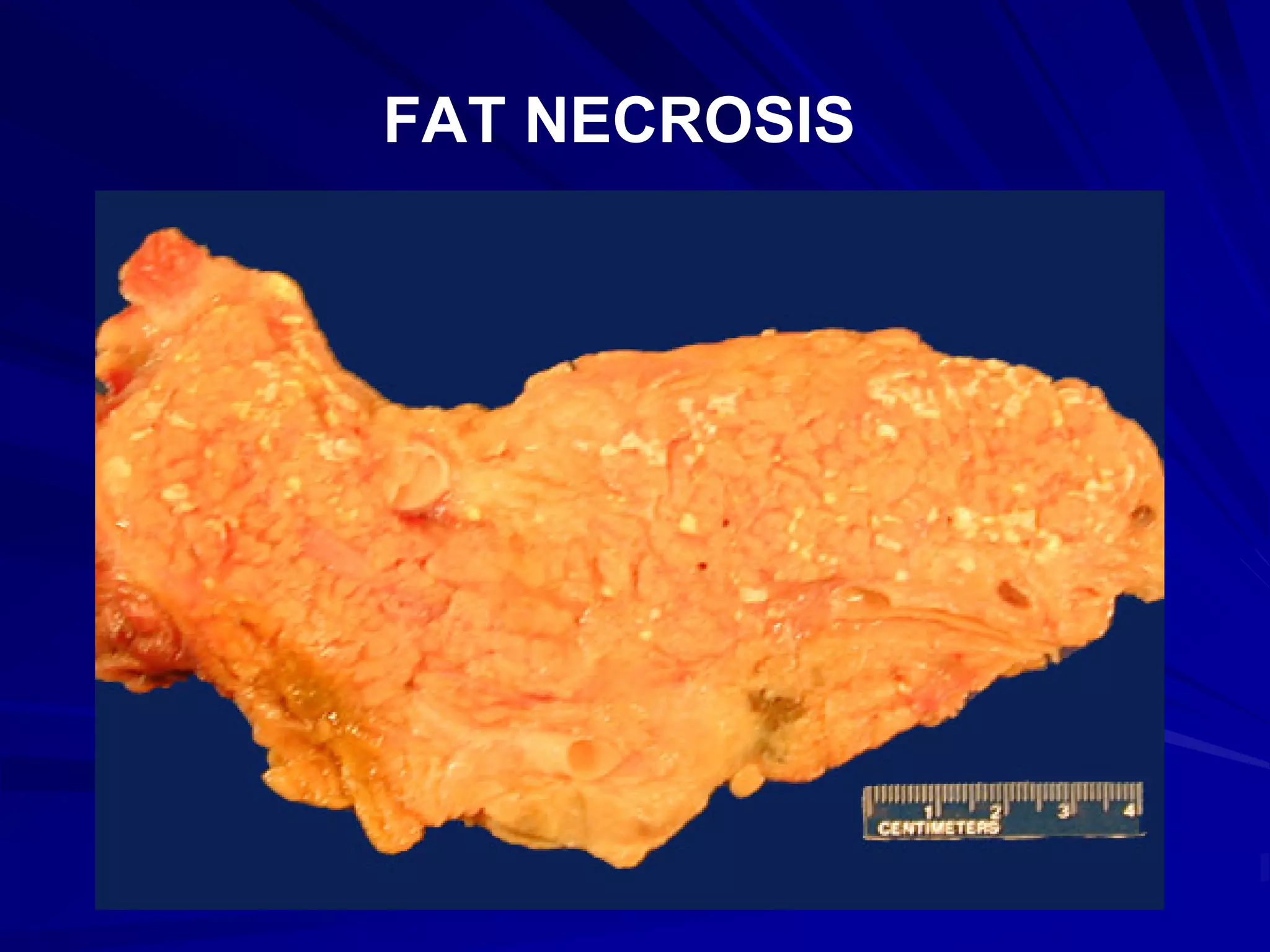
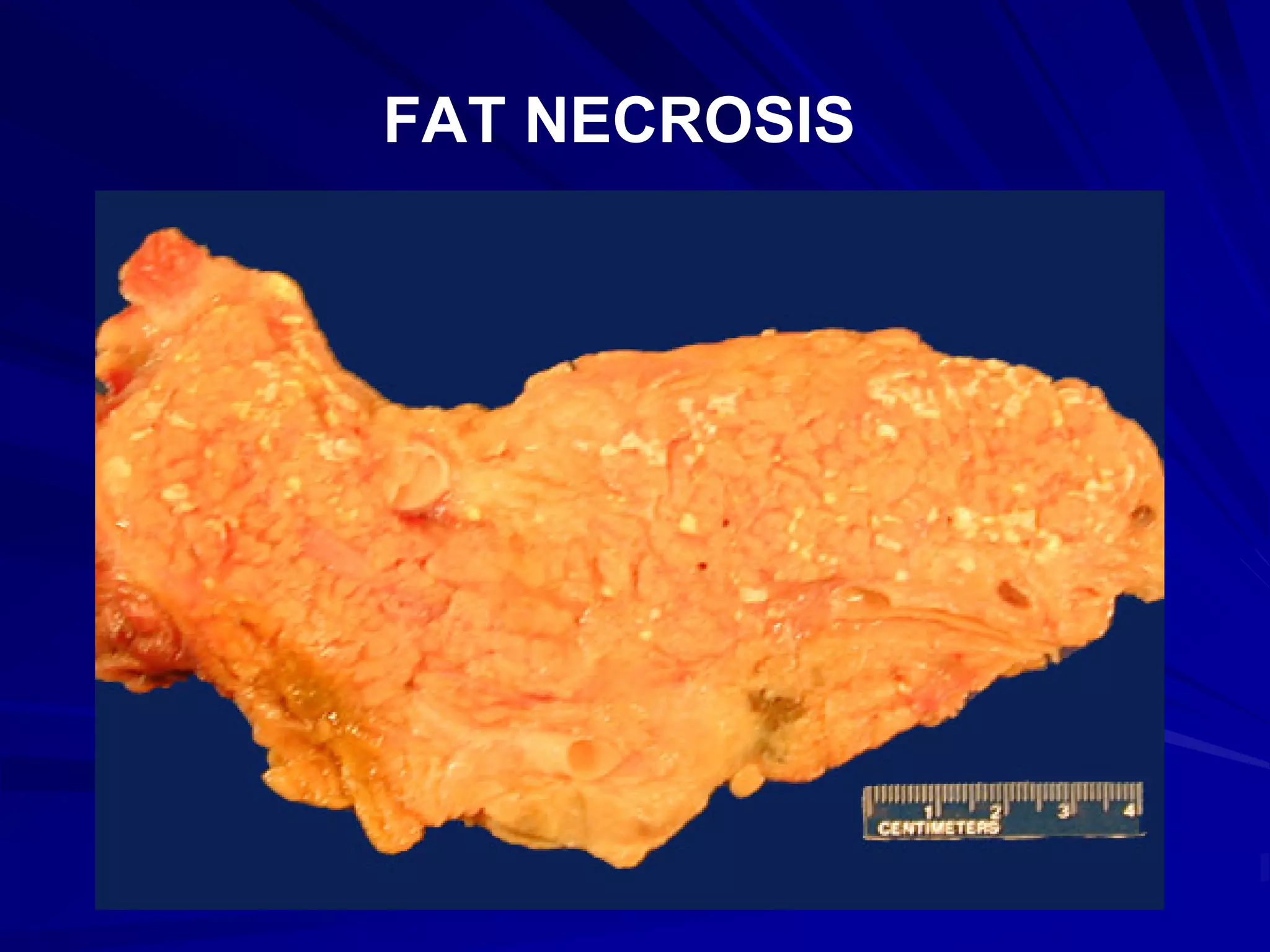
Fat necrosis is linked to pancreatitis with visible chalky areas and outlines of necrotic cells.
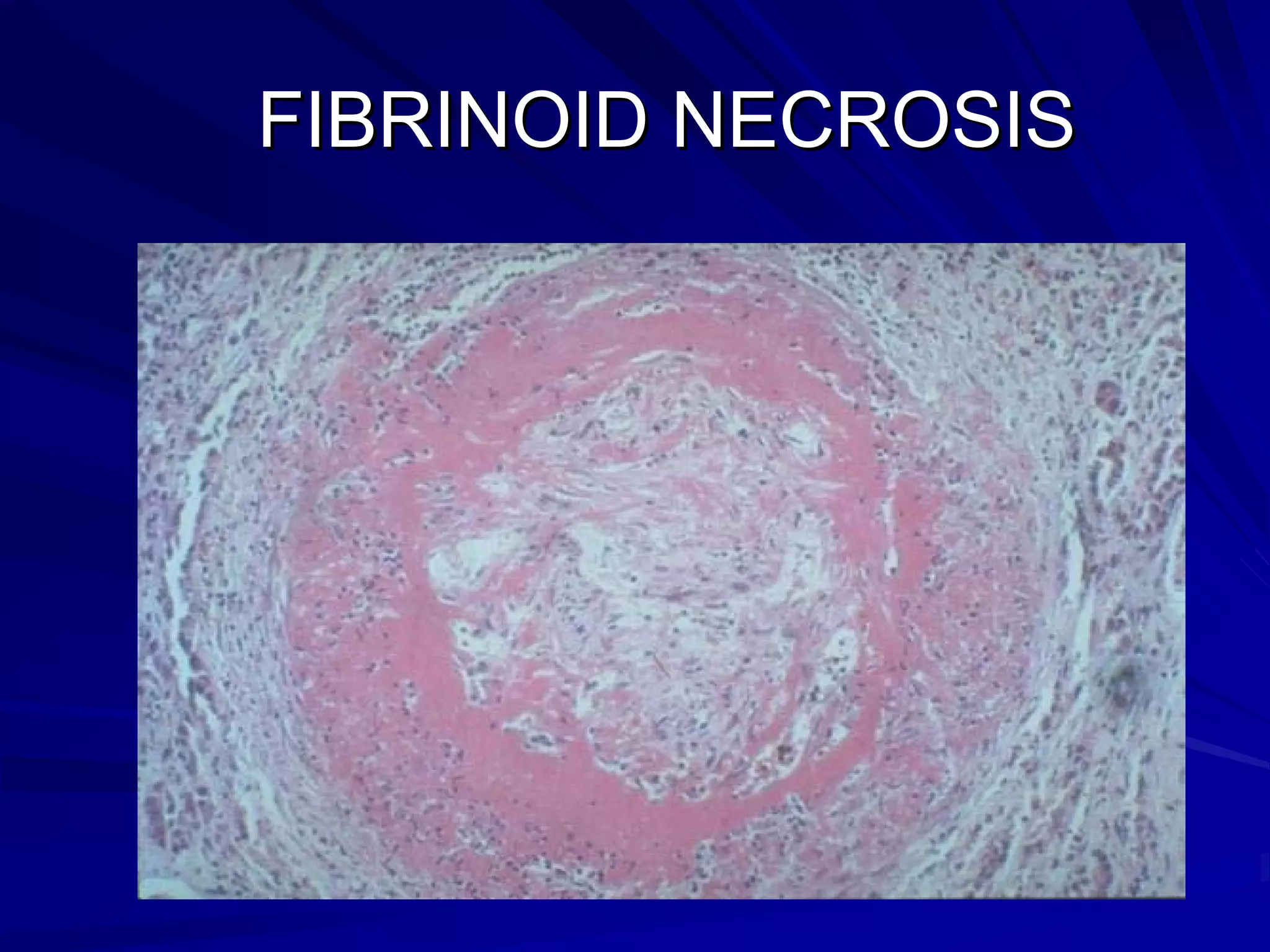
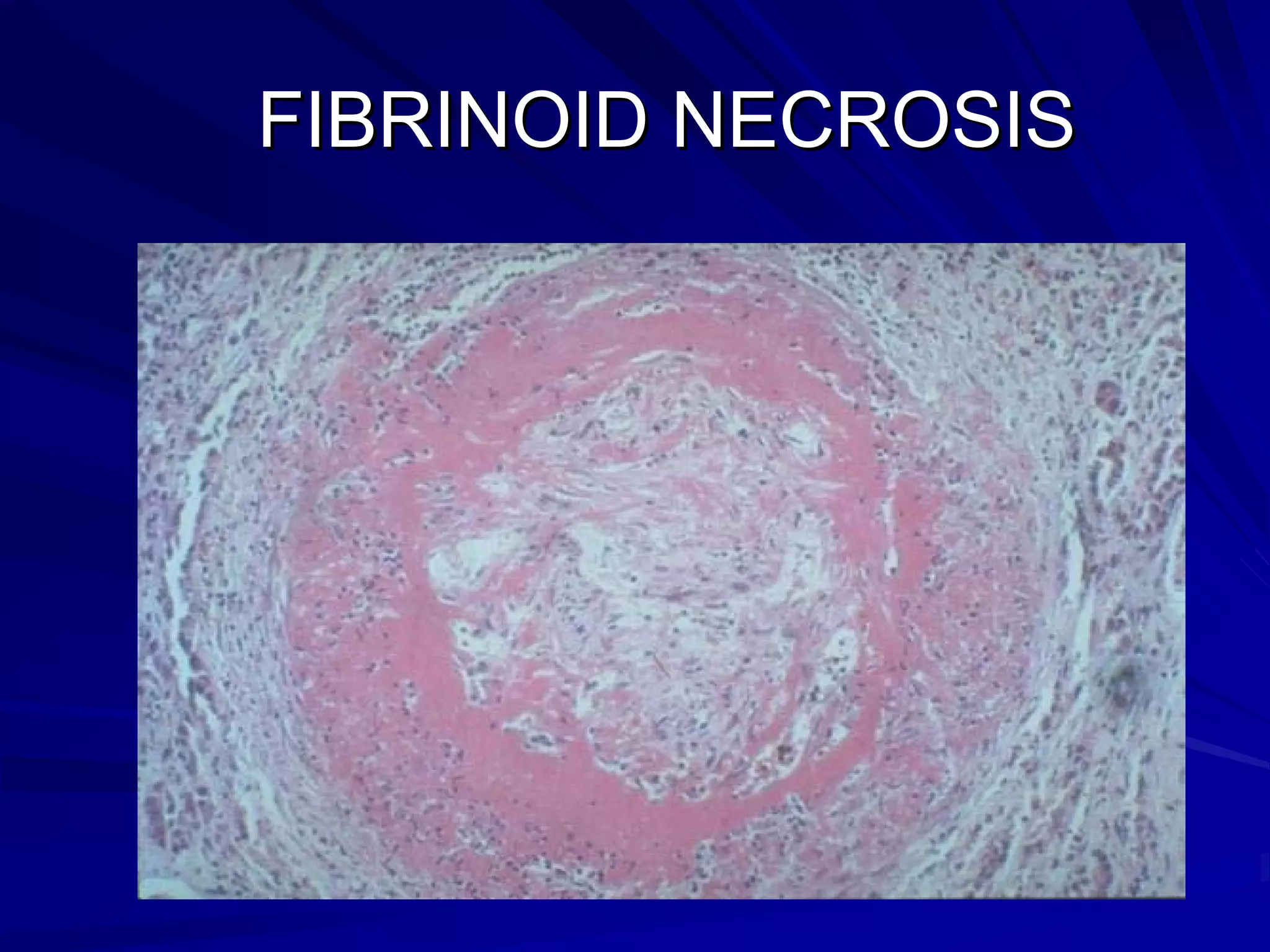
Fibrinoid necrosis involves fibrin deposition, seen in immune injuries; linked to hypertension and ulcers.