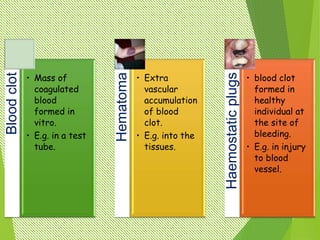
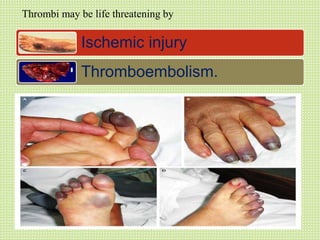
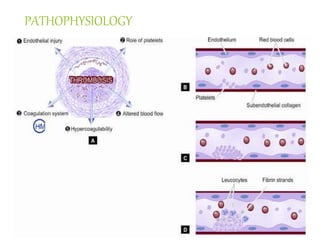
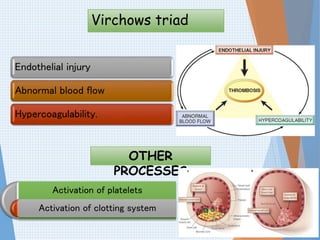
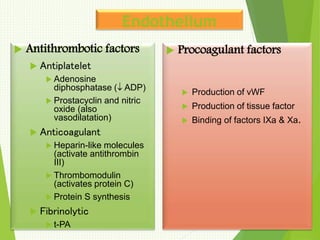
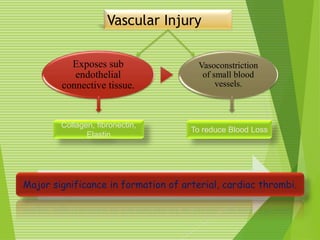
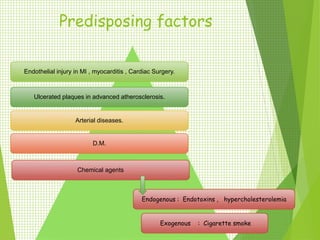
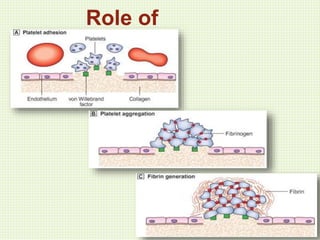
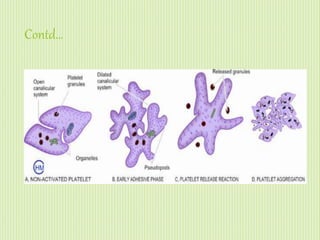
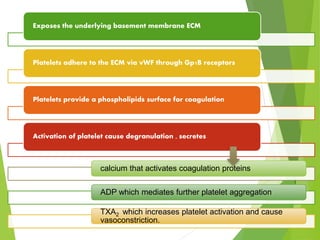
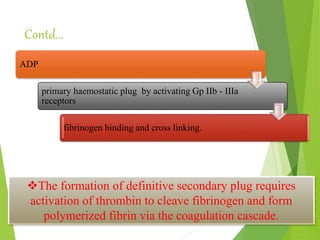
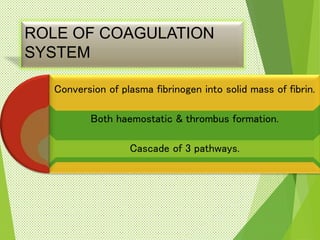
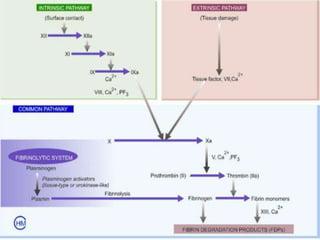
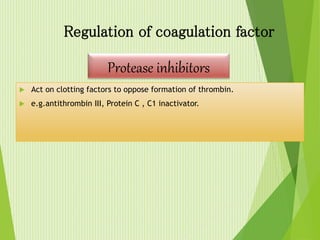
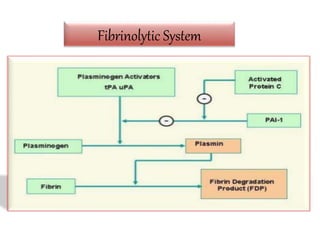
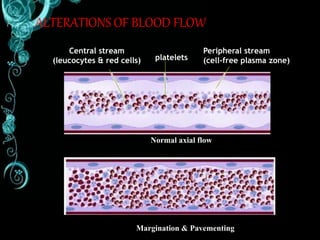
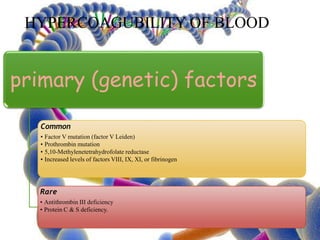
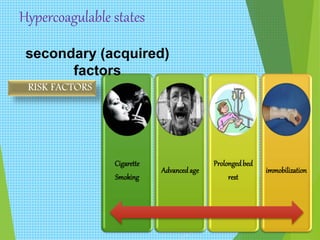
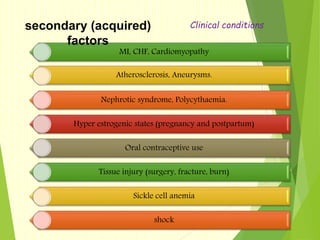
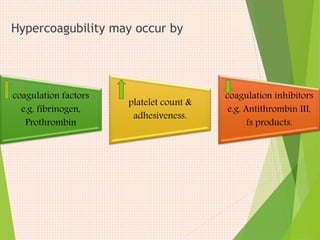
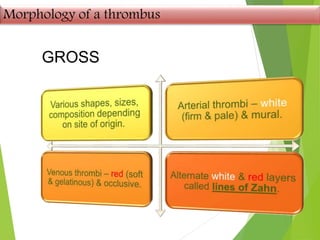
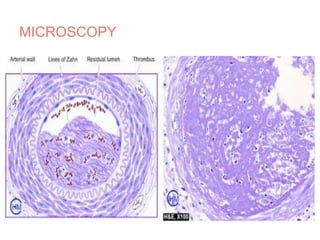
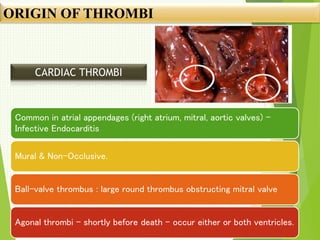
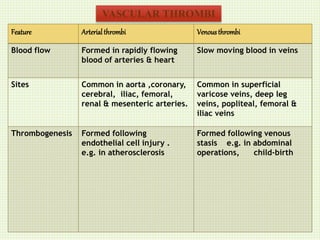
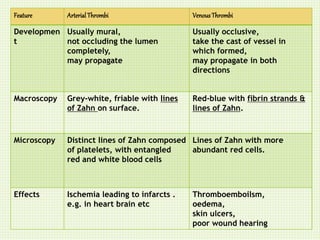
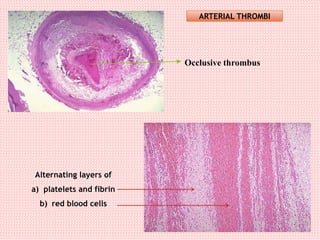
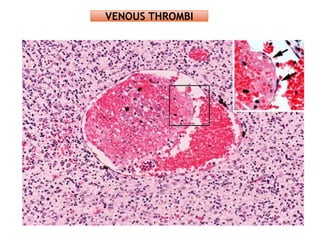
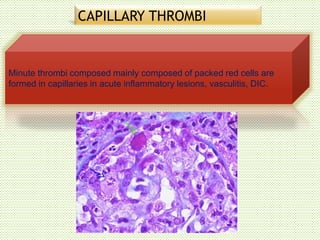
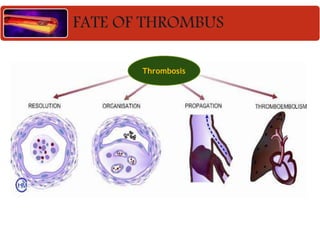
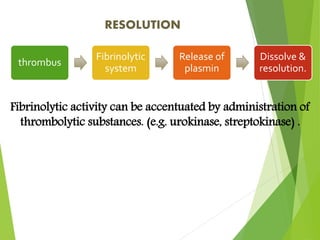
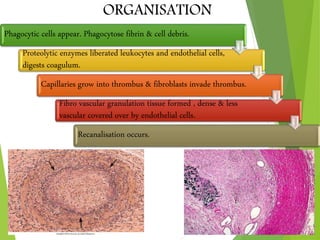
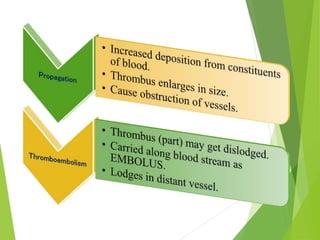
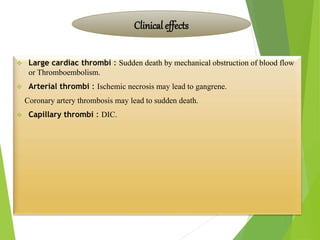
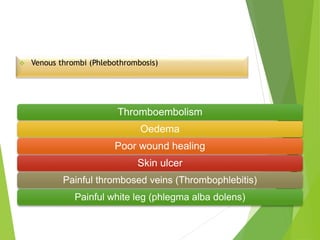
The document discusses thrombosis, including the process of thrombus formation, types of blood clots, and associated pathophysiological mechanisms like Virchow's triad. It describes the roles of platelets and the coagulation system in hemostasis and thrombus formation, along with various predisposing and risk factors, such as endothelial injury and hypercoagulability. Additionally, it covers the morphology, effects, and potential fates of thrombi, along with the clinical implications of venous and arterial thrombi.