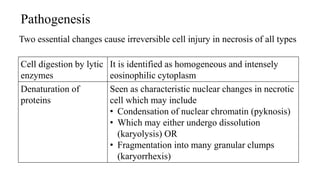
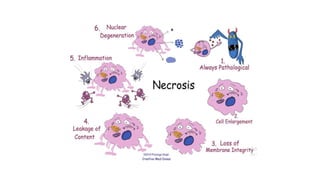
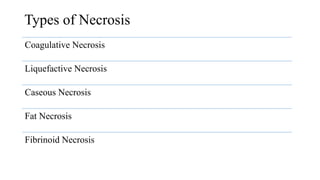
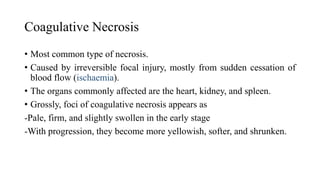
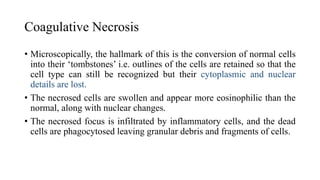
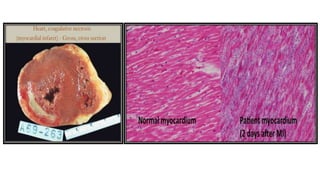
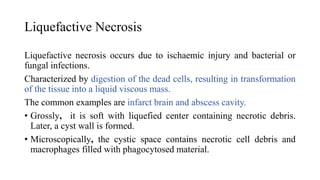
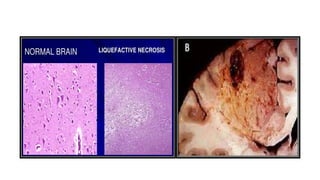
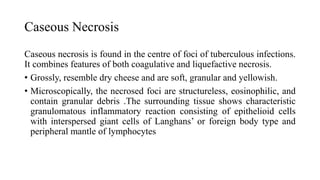
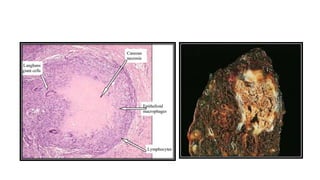
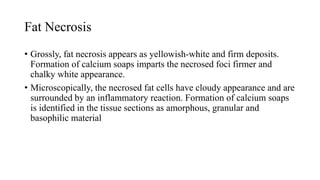
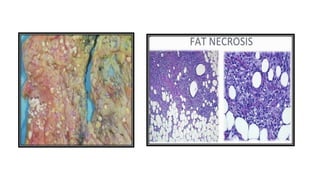
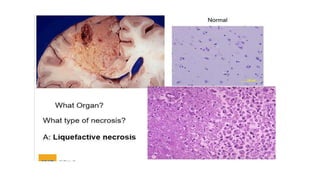
Necrosis is the death of cells and living tissue. It is caused by factors that damage cells such as lack of blood supply, toxins, or infection. There are several types of necrosis including coagulative, liquefactive, and caseous necrosis. Coagulative necrosis occurs when blood flow is cut off, causing cells to die and leave behind outlines. Liquefactive necrosis causes cells to break down into liquid debris, as seen in brain infarcts. Caseous necrosis is seen in tuberculosis and resembles soft cheese. Overall, necrosis involves the irreversible death of cells and tissue.