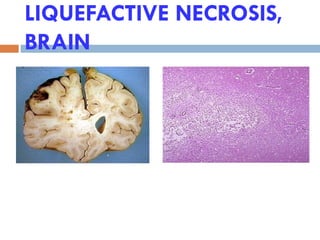
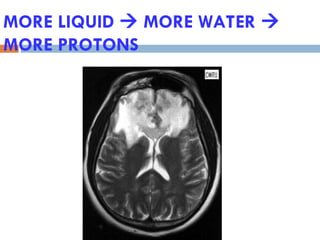
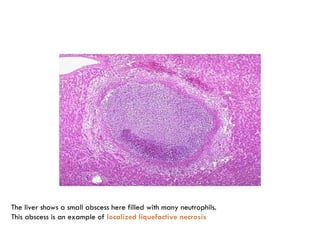
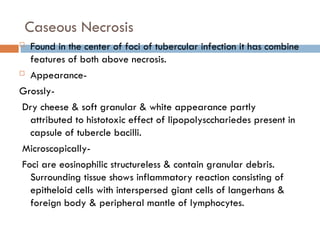
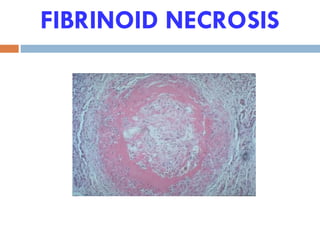
The document discusses cell death mechanisms, highlighting autolysis, apoptosis, and necrosis, each with distinct characteristics and implications. Autolysis is the self-digestion of cells, apoptosis is programmed cell death involved in various physiological and pathological processes, while necrosis refers to cell death due to injury with associated tissue changes. It details different types of necrosis, including coagulative, liquefactive, caseous, fat, and fibrinoid necrosis, along with their causes, morphological features, and examples.