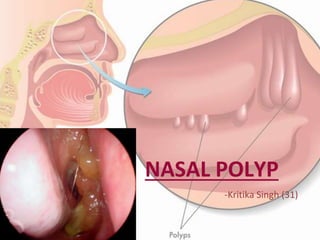
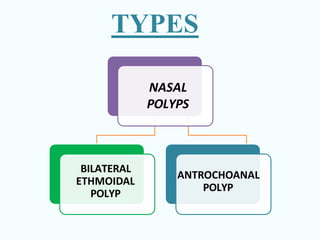
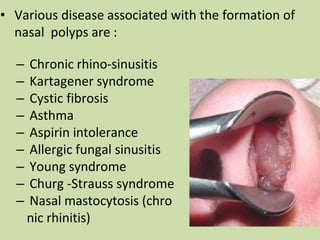
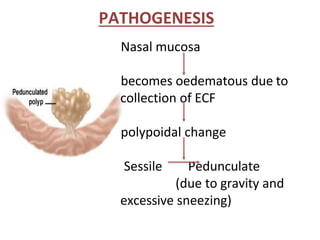
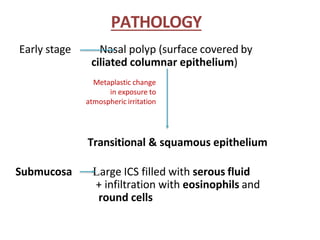
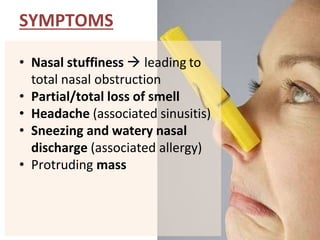
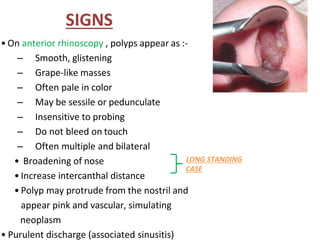
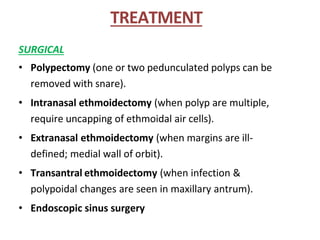
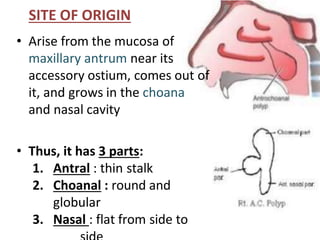
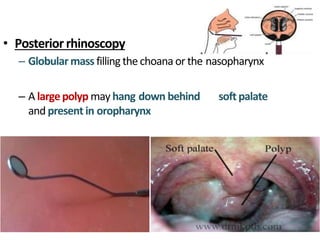
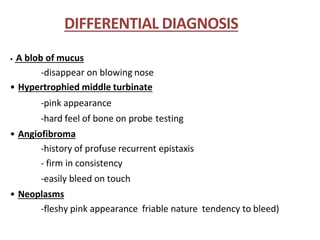
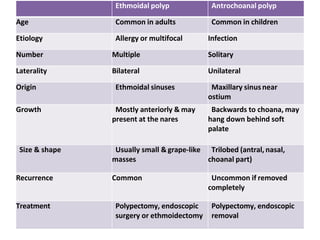
Nasal polyps are non-neoplastic masses that occur in the nasal or sinus mucosa, commonly associated with inflammatory conditions like rhino-sinusitis, cystic fibrosis, and asthma. Symptoms include nasal obstruction, loss of smell, and sinusitis-related headaches, with diagnosis requiring clinical examination and imaging. Treatment options range from conservative measures like antihistamines to surgical interventions such as polypectomy and endoscopic sinus surgery.