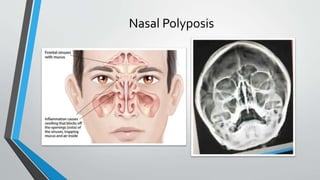
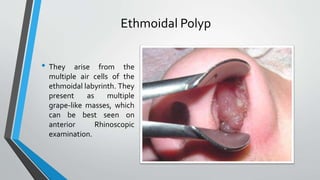
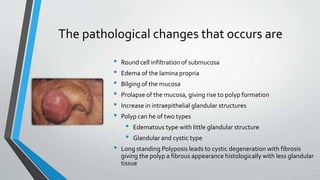
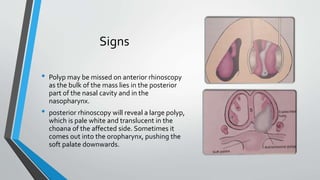
The document discusses nasal polyposis, an inflammatory condition characterized by the formation of nasal polyps, which are soft, jelly-like overgrowths of mucosa. It outlines the types, etiology, incidence, clinical features, pathogenesis, and treatment options for nasal polyps, emphasizing the importance of endoscopic surgery and medical treatment post-surgery. Additionally, it highlights the antrochoanal polyp, its characteristics, symptoms, and recommended surgical intervention.