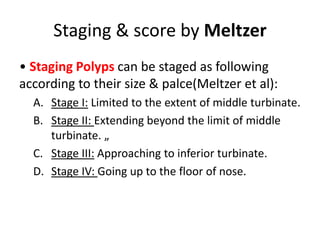
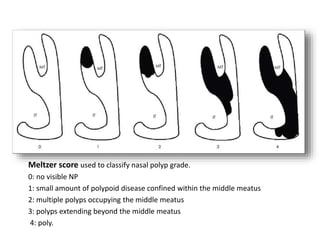
Nasal polyps are non-cancerous growths that develop on the nasal passages or sinuses due to chronic inflammation. They are most commonly caused by asthma, allergies, or recurring sinus infections. Nasal polyps typically appear as soft, teardrop-shaped masses that hang down from the nasal lining. Treatment involves nasal corticosteroids, oral corticosteroids, antibiotics, and surgery to remove polyps. Endoscopic sinus surgery is often required for large or recurring polyps.