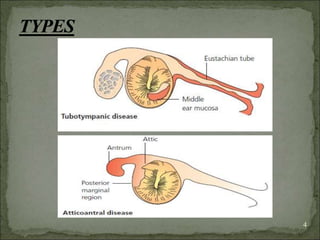
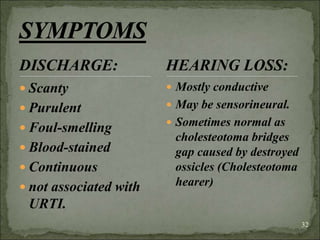
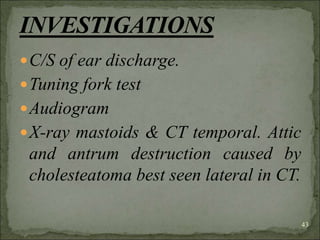
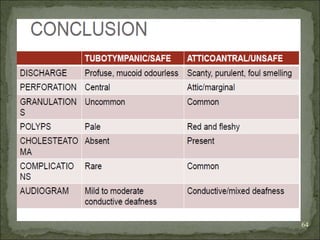
1. Chronic suppurative otitis media (CSOM) is a long-standing middle ear infection characterized by ear discharge and permanent perforation of the eardrum. It is more common in developing countries and affects people of all ages and sexes.
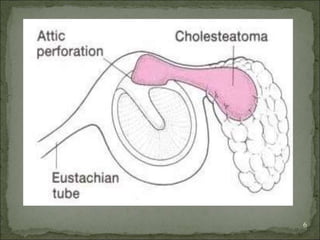
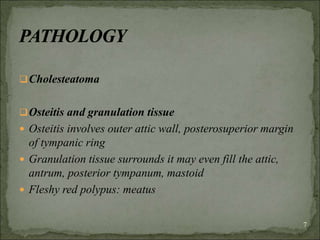
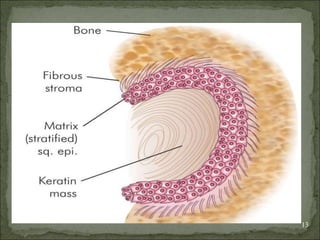
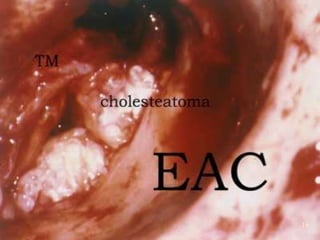
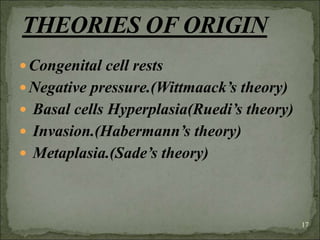
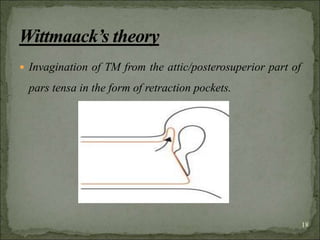
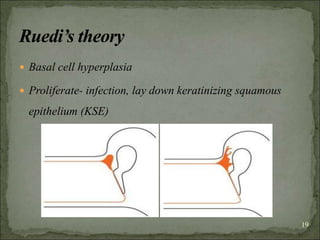
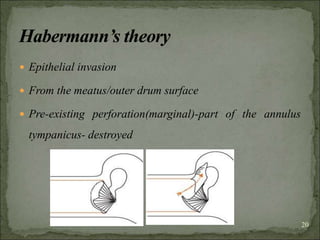
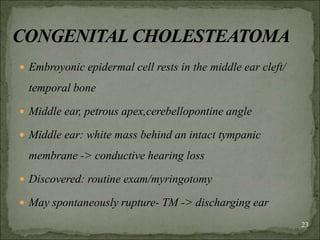
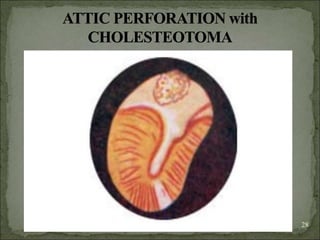
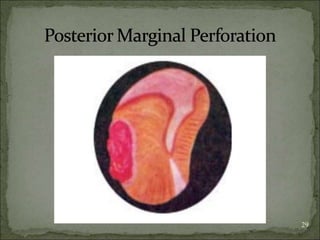
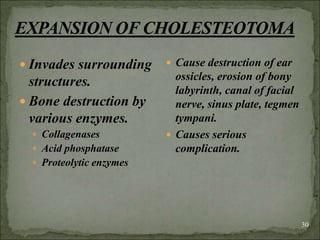
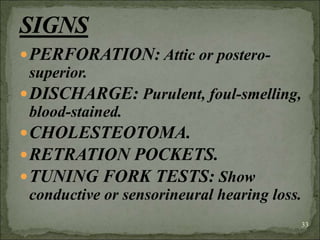
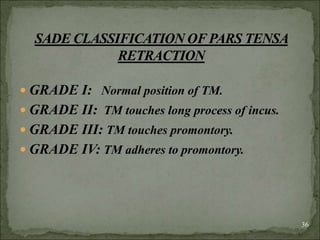
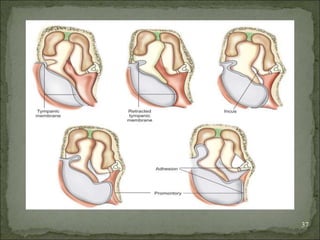
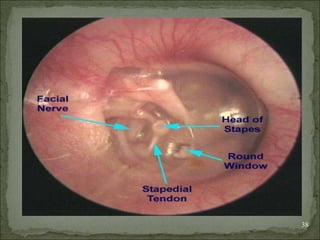
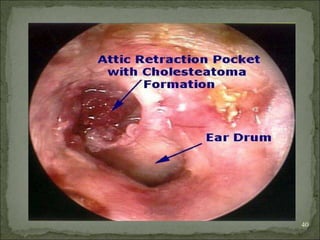
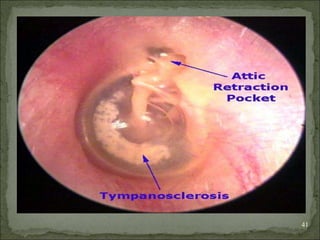
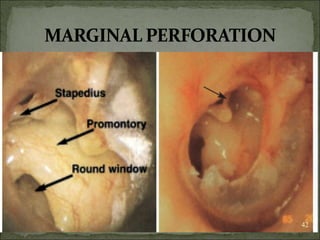
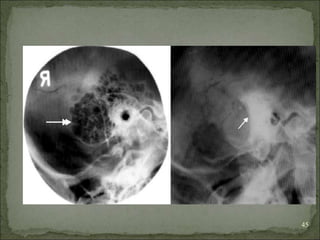
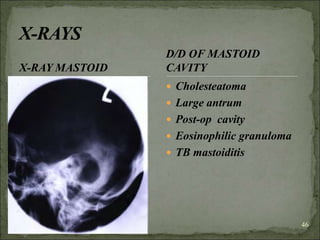
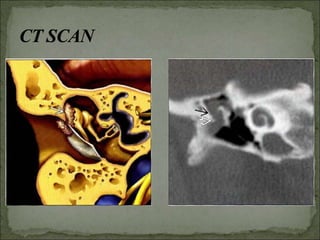
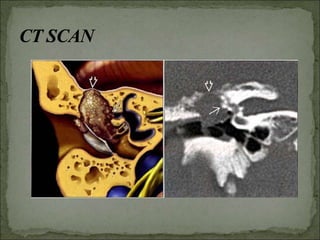
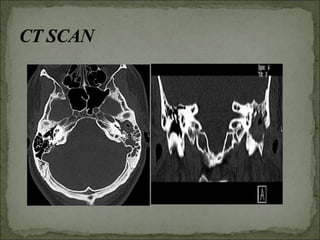
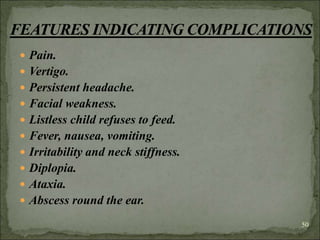
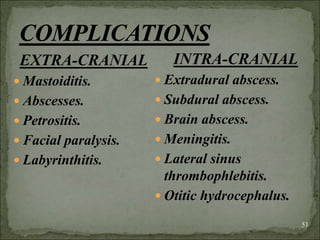
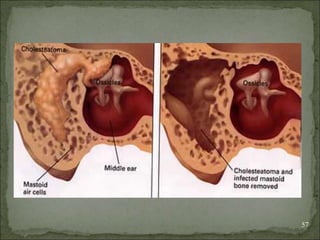
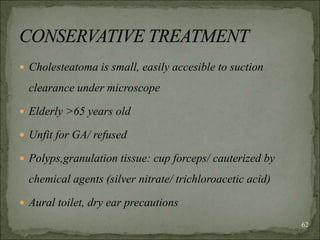
2. Cholesteatoma is a type of CSOM where the disease spreads to the bony walls of the middle ear, posing risks of dangerous complications. It is associated with a buildup of skin cells (cholesteatoma), inflammation (osteitis), and granulation tissue in the middle ear.
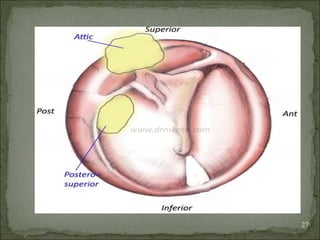
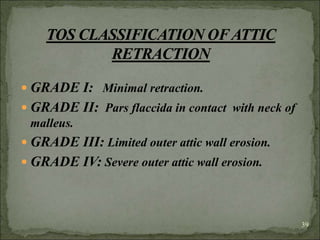
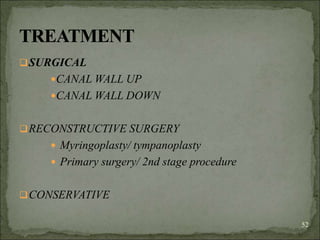
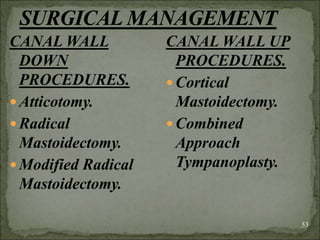
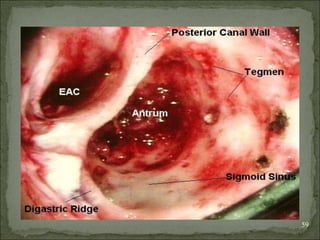
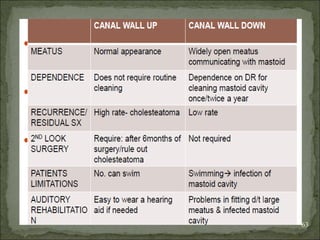
3. Treatment options include surgical procedures like canal wall up or canal wall down mastoidectomies to remove