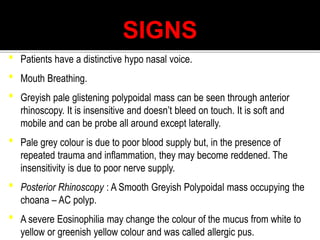
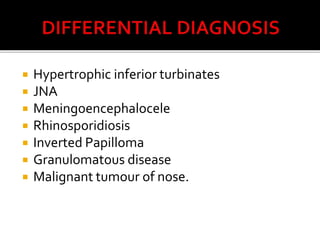
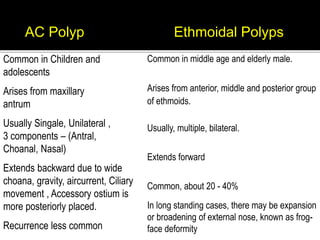
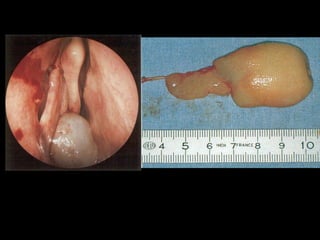
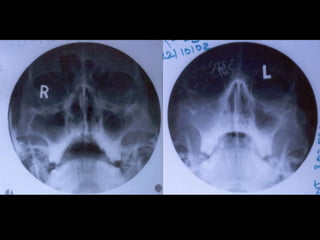
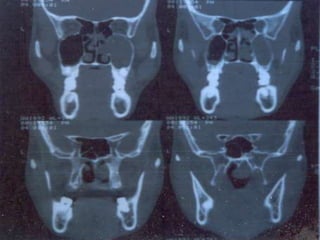
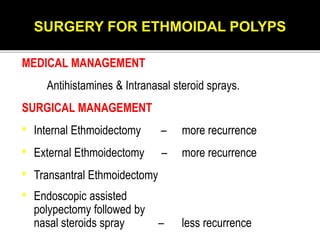
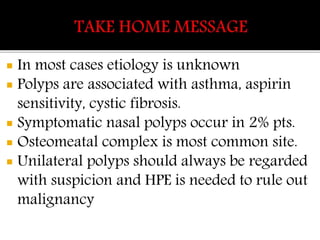
This document discusses nasal polyps, including their definition, types, pathogenesis, clinical features, investigations, and management. There are two main types of nasal polyps - ethmoidal and antrochoanal polyps. The pathogenesis involves mucosal reactions, poorly developed sinus blood supply, and sinus anatomy. Clinical features include nasal obstruction, loss of smell, and sneezing. Investigations include CT scans and endoscopy. Management consists of steroids, polypectomy, and sinus surgery.