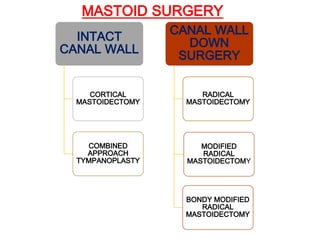
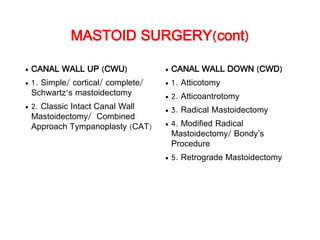
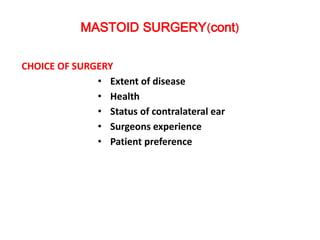
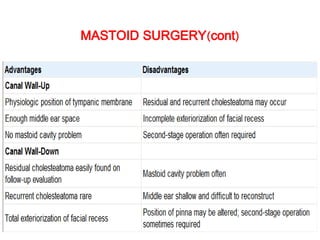
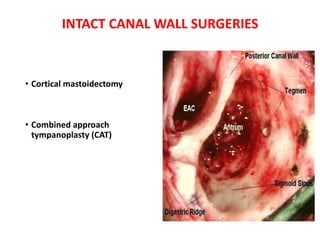
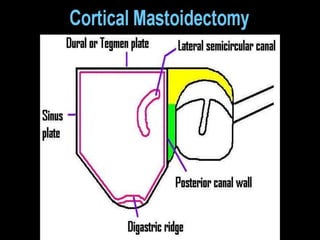
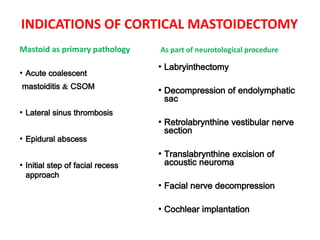
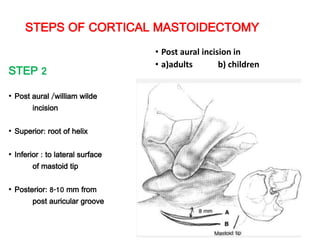
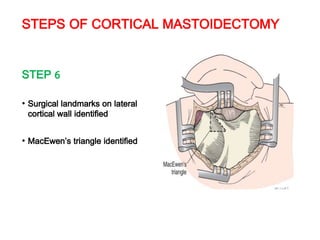
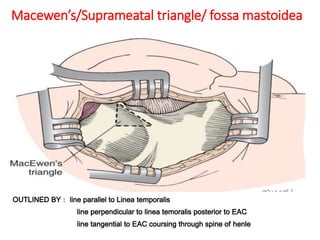
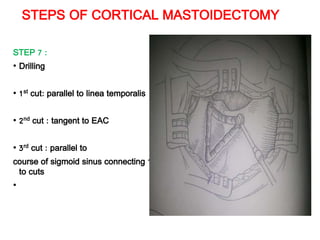
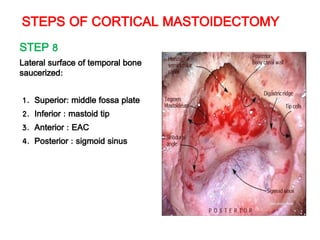
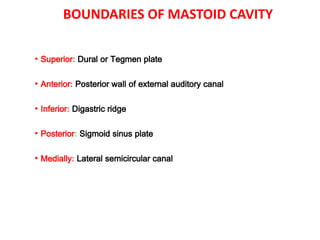
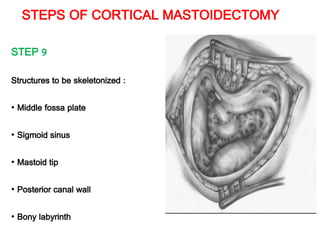
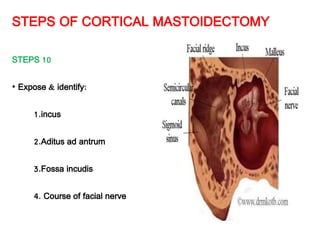
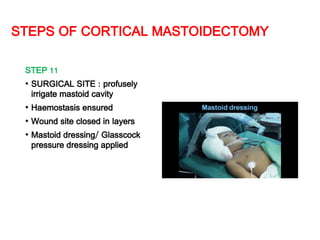
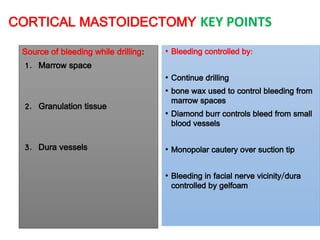
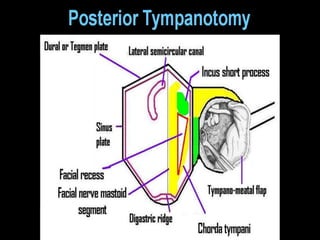
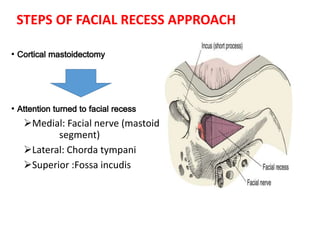
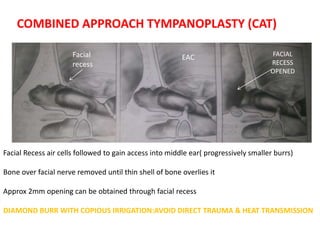
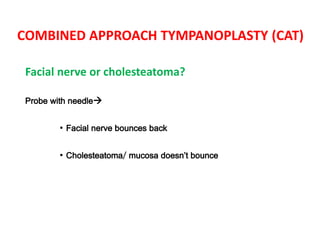
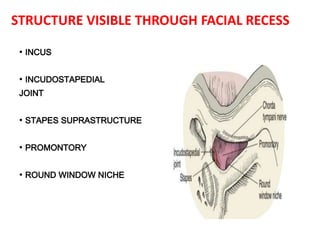
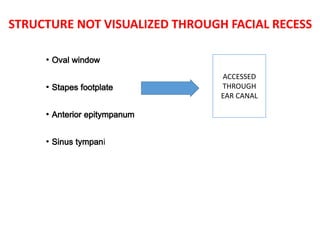
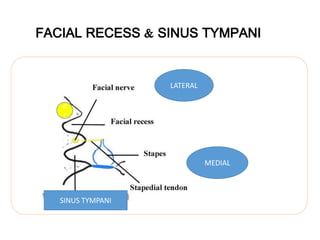
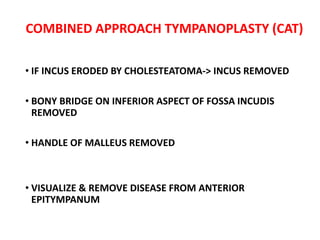
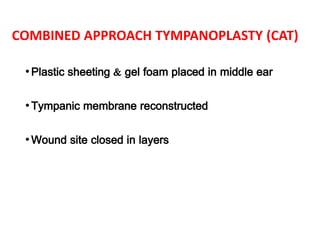
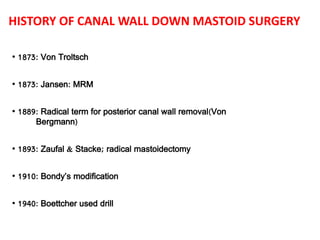
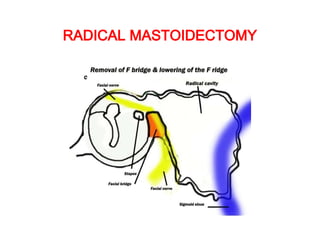
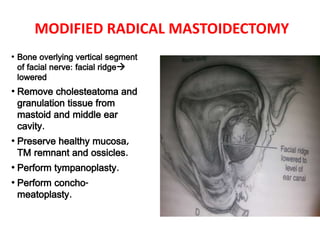
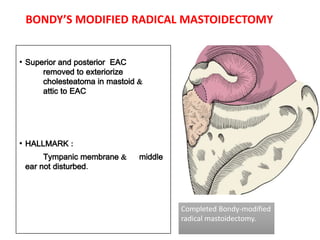
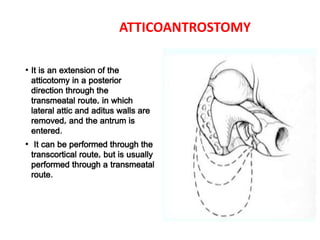
This document discusses different surgical procedures for chronic suppurative otitis media (CSOM), including cortical mastoidectomy, combined approach tympanoplasty (CAT), and canal wall down procedures like radical and modified radical mastoidectomy. It outlines the objectives, indications, surgical steps, and key points for cortical mastoidectomy and CAT. These intact canal wall surgeries aim to eradicate disease while preserving the ear canal. Canal wall down procedures are indicated for more extensive disease and create a common cavity in the mastoid, middle ear, and ear canal.