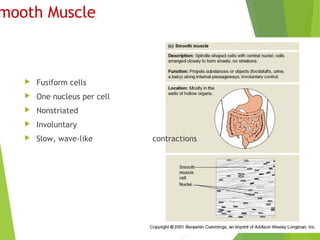
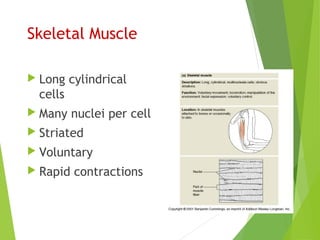
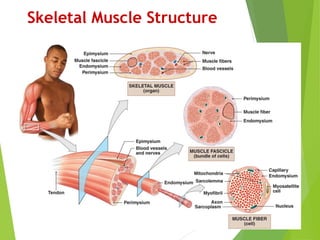
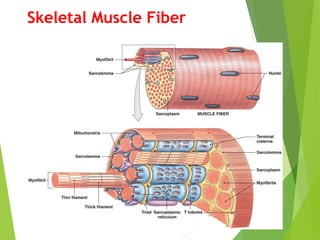
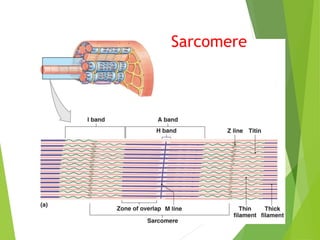
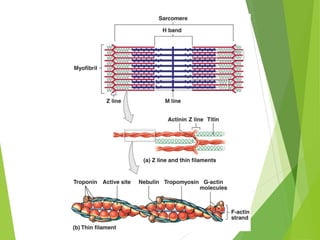
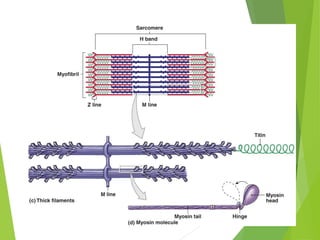
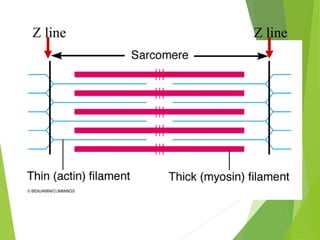
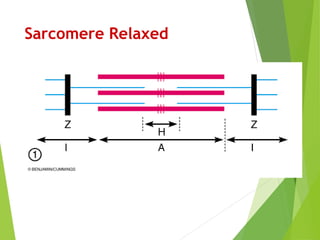
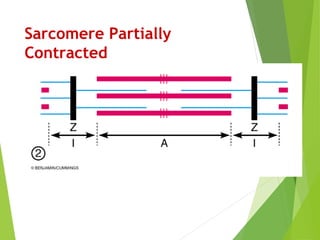
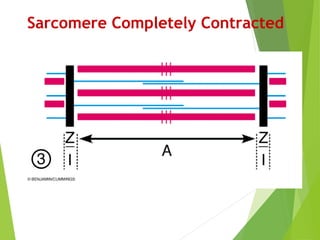
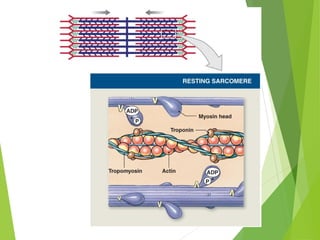
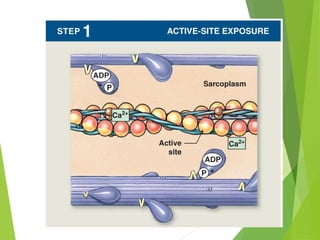
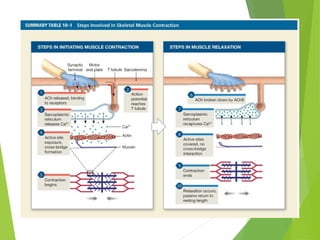
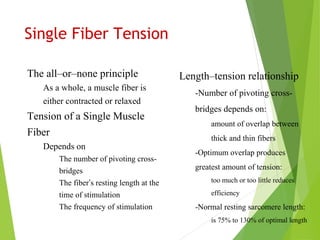
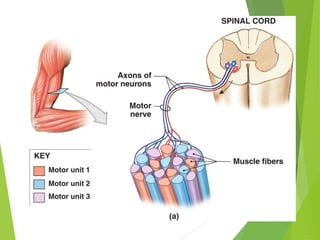
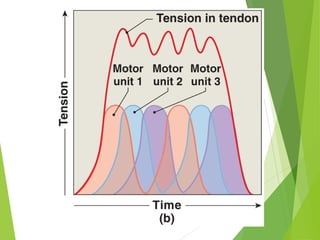
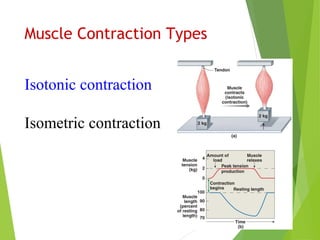
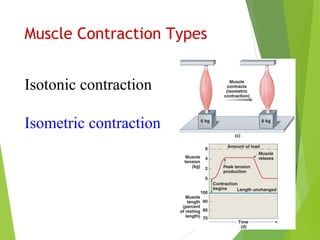
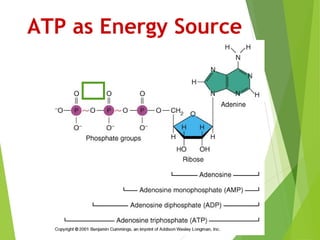
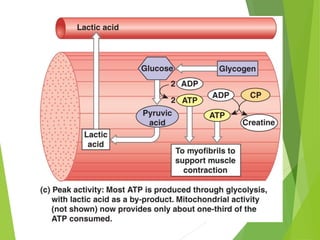
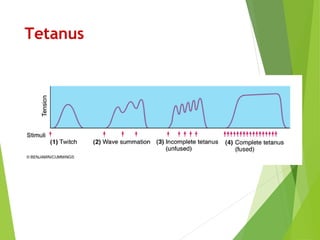
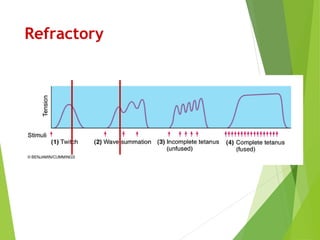
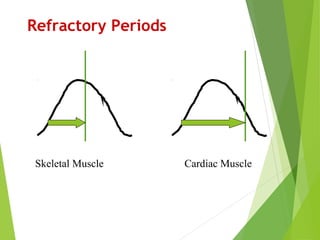
This document discusses the three main types of muscle tissue - skeletal, cardiac, and smooth muscle. It describes their structural and physiological characteristics, including that skeletal muscle is striated and voluntary, cardiac muscle is striated and involuntary, and smooth muscle is non-striated and involuntary. The document also examines the structure of skeletal muscle fibers down to the sarcomere level and explores muscle contraction types, the role of ATP as an energy source, and factors that influence muscle tension and can lead to fatigue.