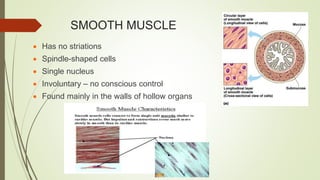
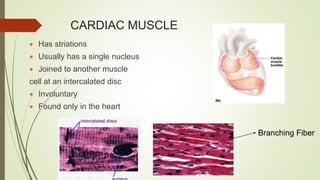
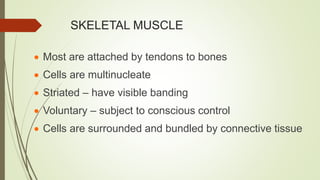
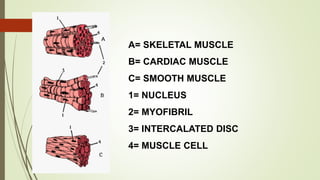
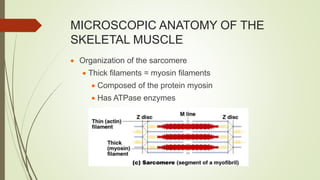
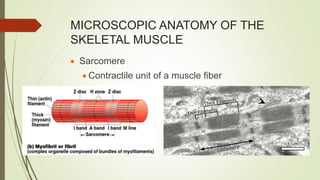
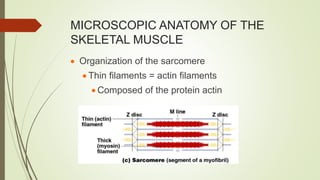
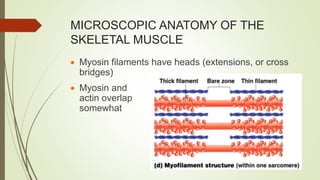
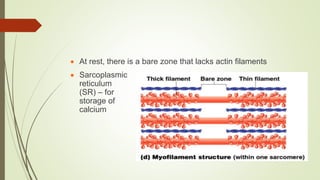
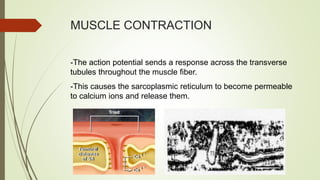
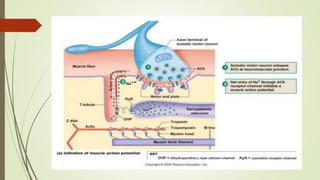
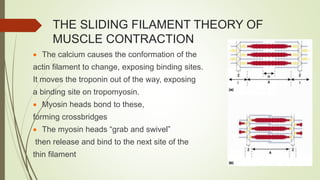
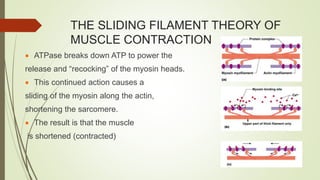
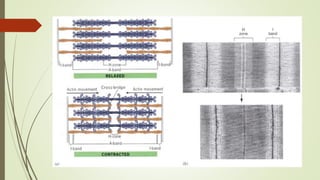
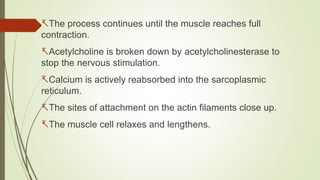
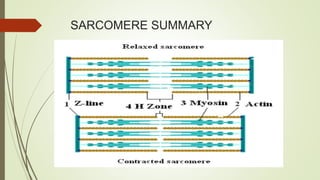
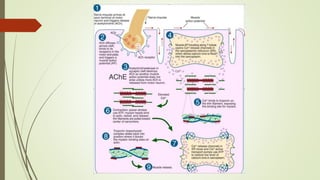
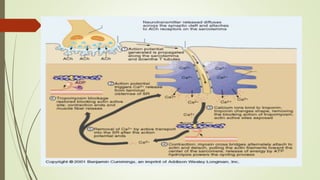
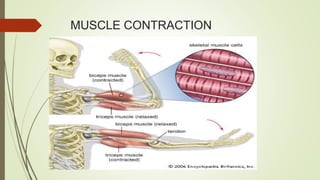
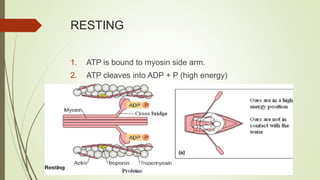
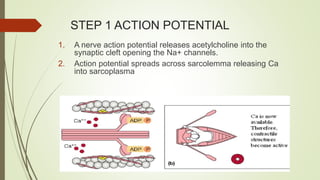
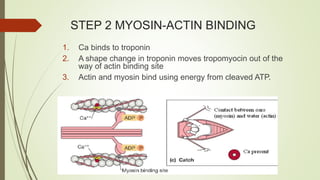
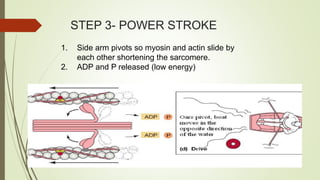
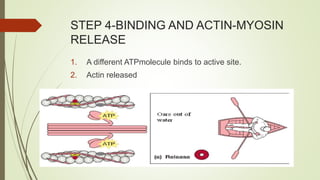
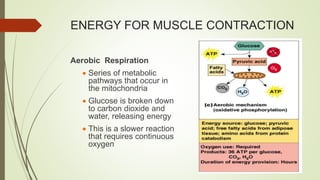
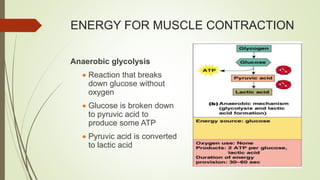
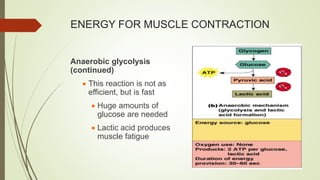
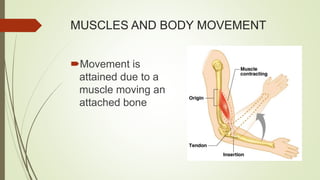
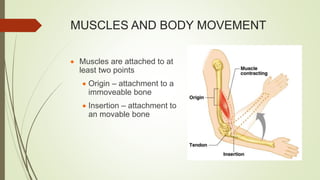
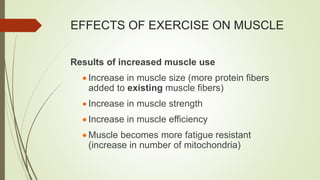
The muscular system is composed of three main types of muscle - skeletal, cardiac, and smooth muscle. Skeletal muscle is voluntary and attached to bones, producing movement. It contracts through the sliding filament theory where actin and myosin interact powered by ATP. Muscle contraction provides movement, posture, heat generation, and joint stabilization. Fatigue occurs due to the buildup of lactic acid from anaerobic respiration when oxygen demands are not met.