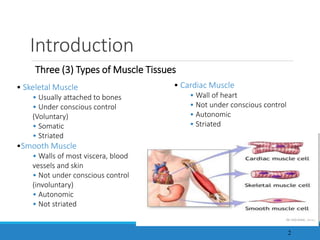
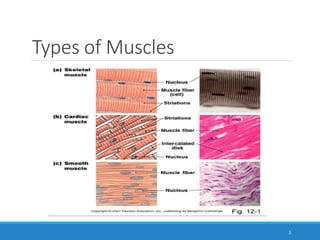
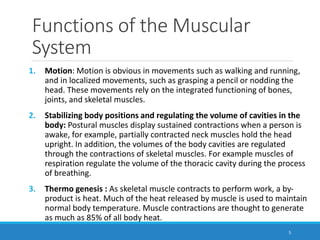
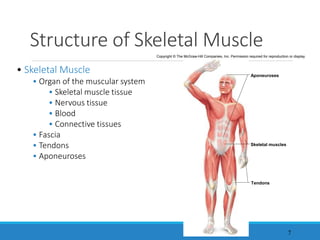
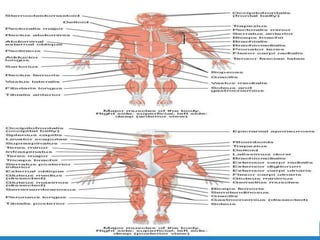
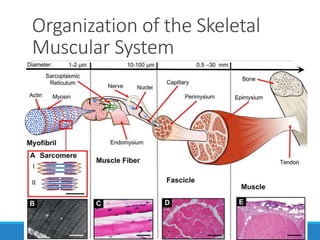
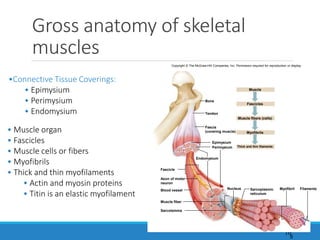
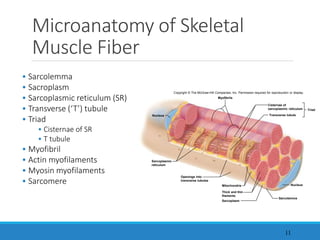
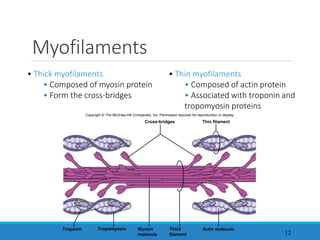
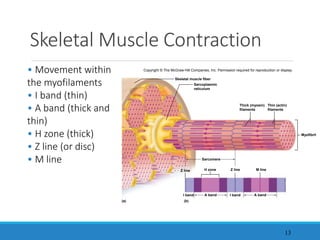
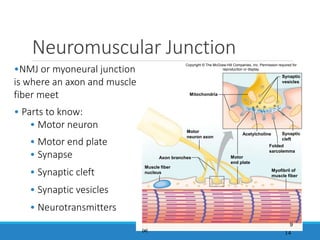
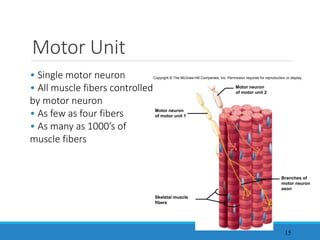
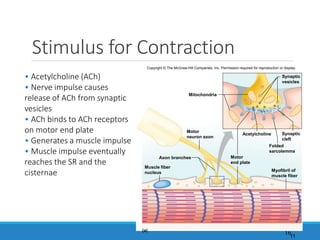
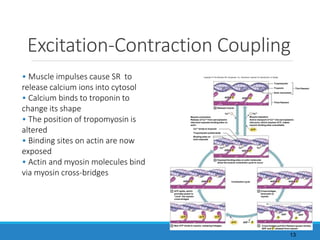
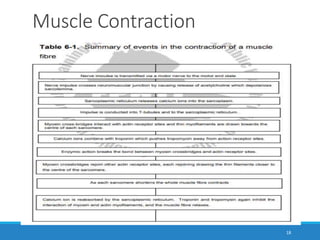
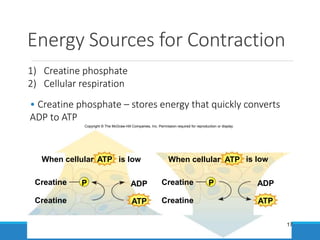
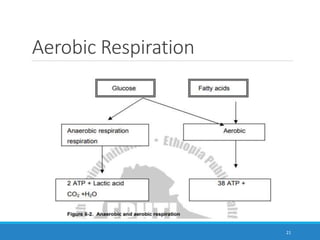
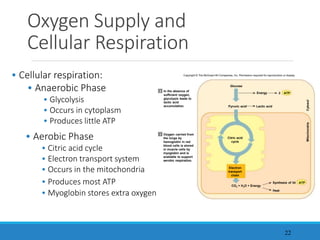
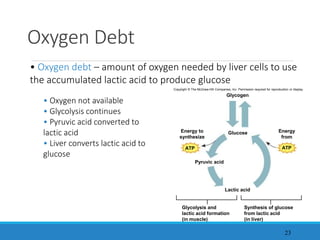
The document discusses the muscular system, describing the three main types of muscle tissue - skeletal, smooth, and cardiac muscle - and their functions. It examines the structure of skeletal muscle from the organ level down to the molecular level. Key concepts covered include muscle contraction, the roles of actin and myosin fibers, energy sources for muscle work, and effects of aging on muscle mass, fiber number and size, motor units, and performance.