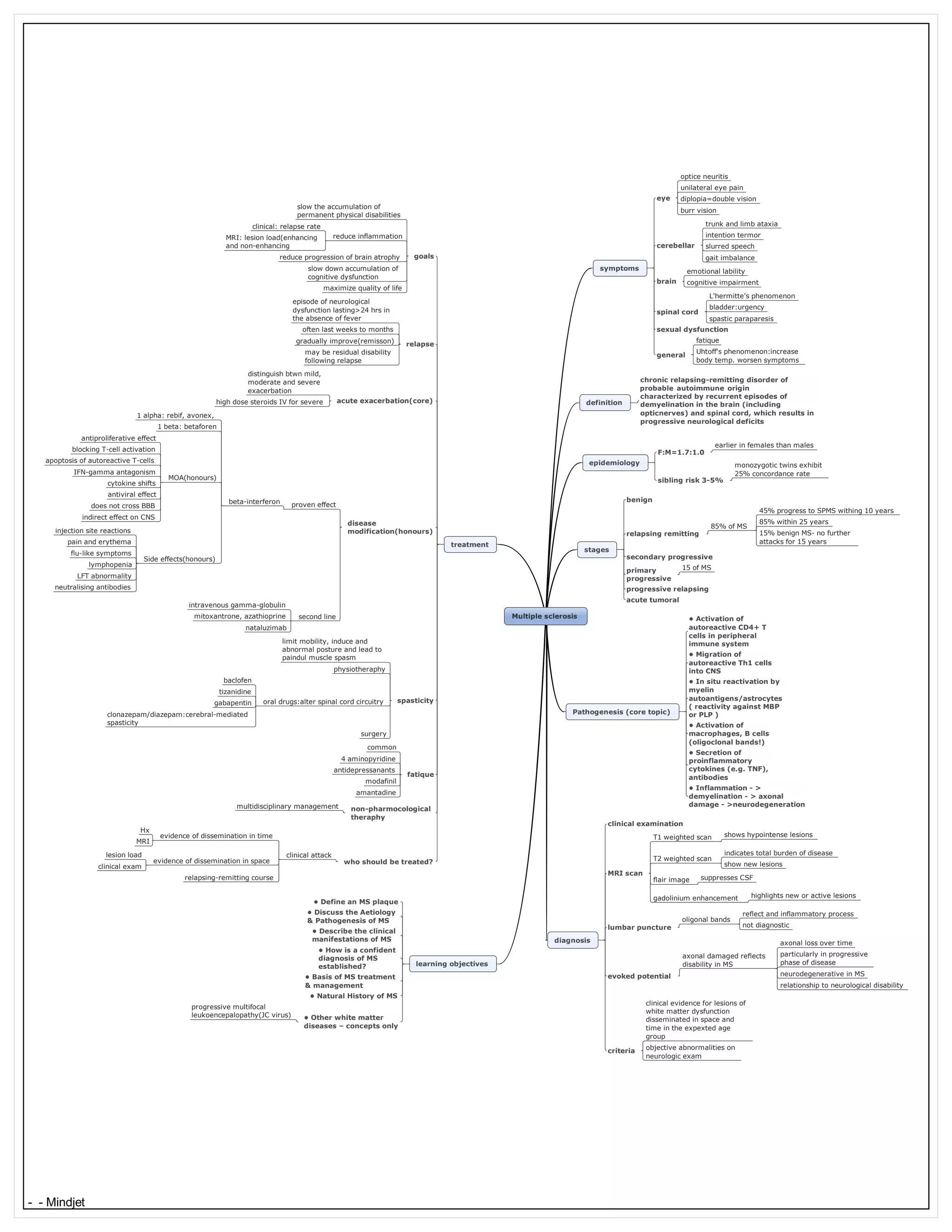
Multiple sclerosis (MS) is a chronic, inflammatory disease of the central nervous system characterized by demyelination of nerve fibers in the brain and spinal cord. Common symptoms include vision problems, muscle weakness, numbness, and impaired coordination. The cause is believed to be an autoimmune reaction where the immune system attacks myelin. A diagnosis requires evidence of lesions in both time and space on clinical examination and MRI imaging. While there is no cure, treatments aim to reduce inflammation and relapse rate to slow progression of disability.