1) Dr Sandhya Manorenj presented information on multiple sclerosis (MS) including its epidemiology, clinical patterns, diagnosis, management, and monitoring of treatment response.
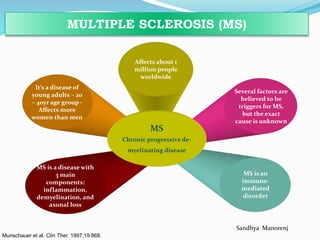
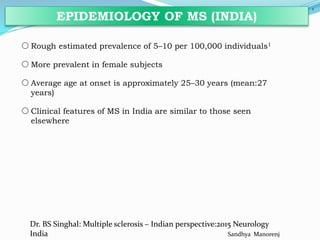
2) MS is a chronic inflammatory disease that affects the central nervous system. It is most common in young adults aged 20-40 years and affects more women than men.
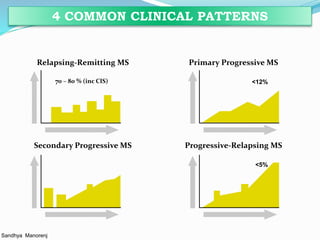
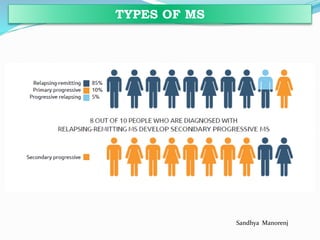
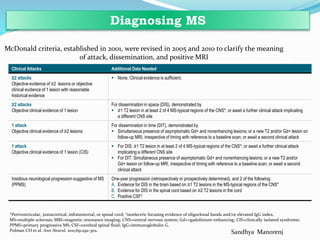
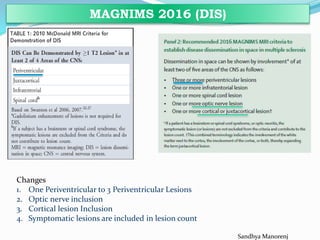
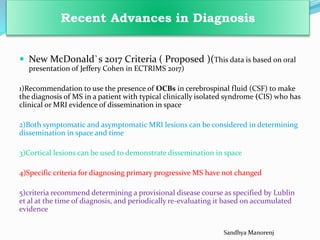
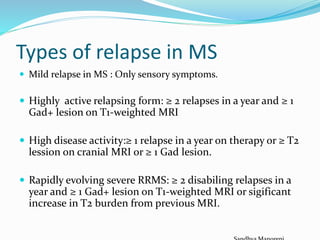
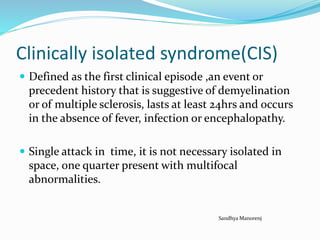
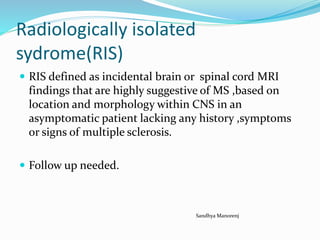
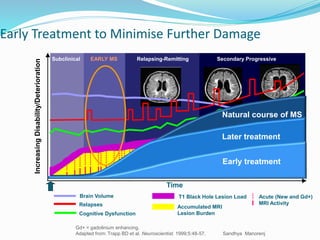
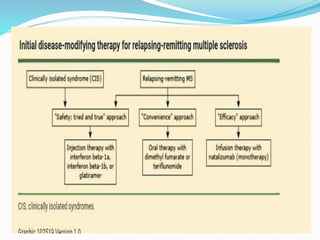
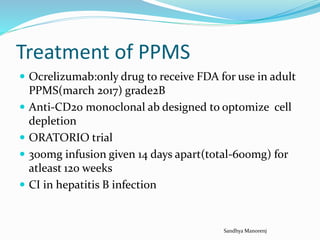
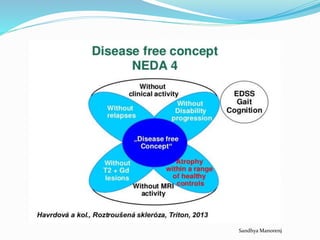
3) There are four main clinical patterns of MS including relapsing-remitting MS, primary progressive MS, secondary progressive MS, and progressive-relapsing MS. Diagnosis involves evaluating clinical symptoms and MRI findings based on McDonald criteria.
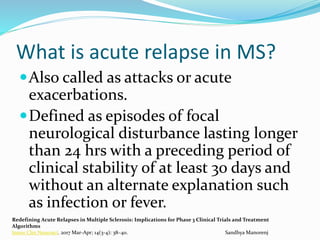
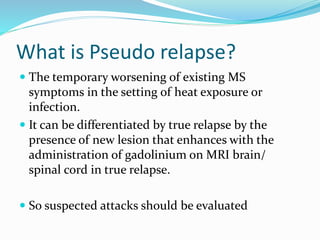
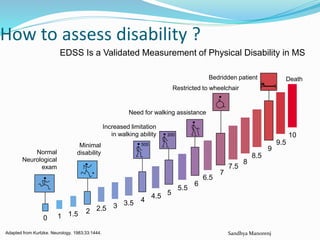
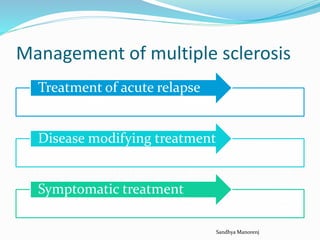
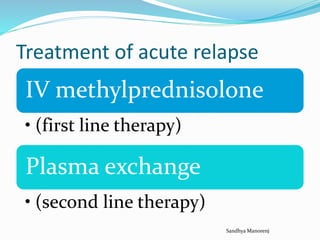
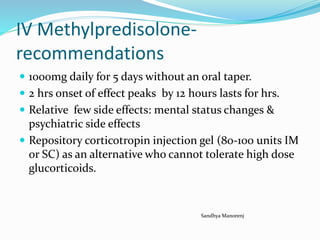
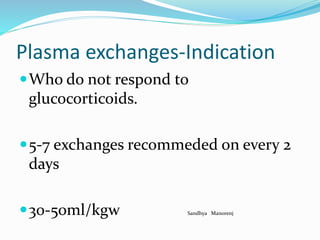
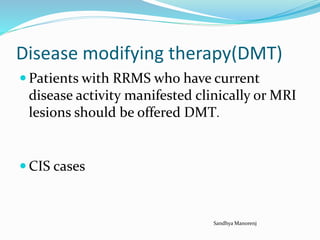
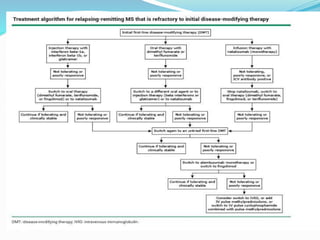
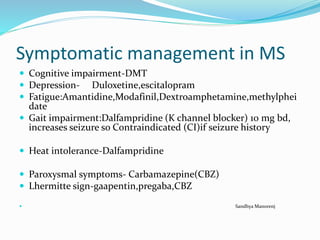
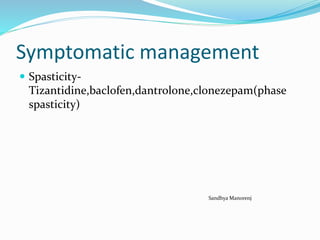
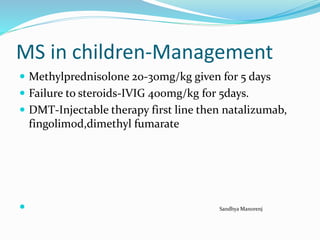
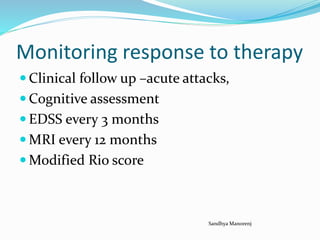
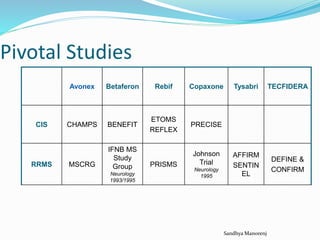
4) Management of MS includes treatment of acute relapses with corticosteroids, disease-modifying therapies,