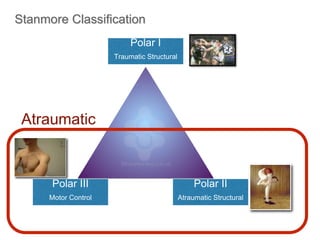
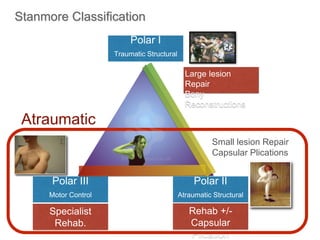
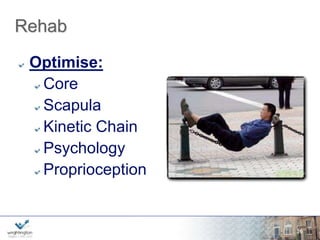
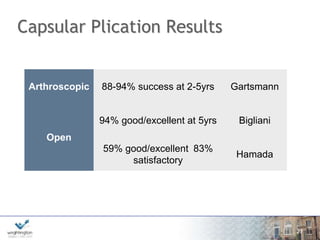
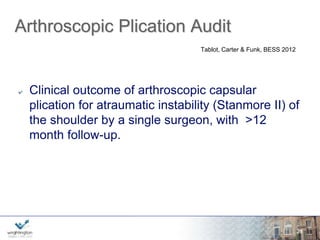
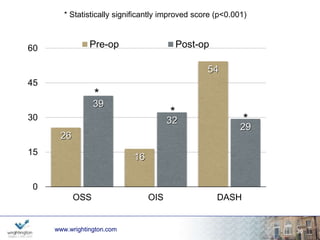
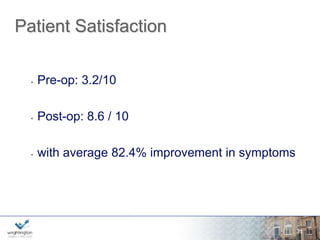
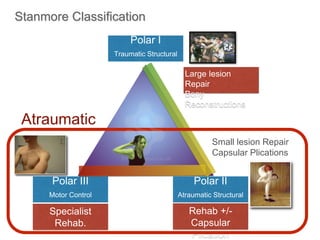
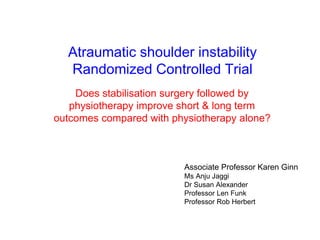
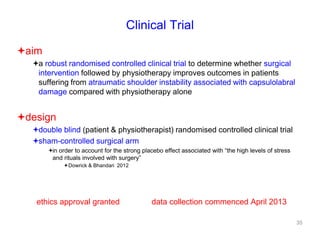
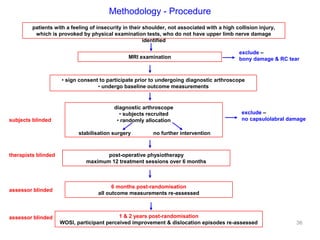
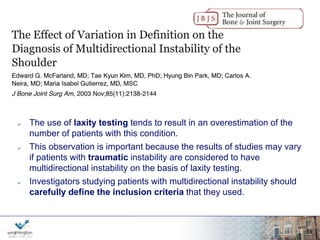
The document discusses shoulder instability, detailing various cases of patients with multidirectional instability and the definitions related to the condition. It highlights outcomes of surgical interventions for atraumatic shoulder instability, mentioning a randomized controlled trial to compare the effectiveness of surgical stabilization combined with physiotherapy against physiotherapy alone. The findings suggest that surgical intervention may enhance recovery in patients suffering from capsulolabral damage.


![MDI - Definitions?
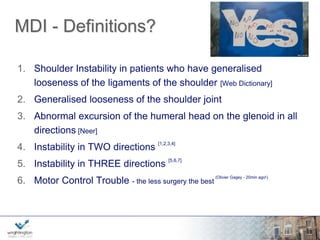
1. Shoulder Instability in patients who have generalised
looseness of the ligaments of the shoulder [Web Dictionary]
2. Generalised looseness of the shoulder joint
3. Abnormal excursion of the humeral head on the glenoid in all
directions [Neer]
4. Instability in TWO directions [1,2,3,4]
5. Instability in THREE directions [5,6,7]
6. Motor Control Trouble - the less surgery the best
wwwwww.w.wrigrhigtinhgttionng.ctoomn.com
(Olivier Gagey - 20min ago!)
6](https://image.slidesharecdn.com/multidirectionalinstabilityoftheshoulder2014-141020004508-conversion-gate02/85/Multidirectional-instability-of-the-shoulder-2014-6-320.jpg)

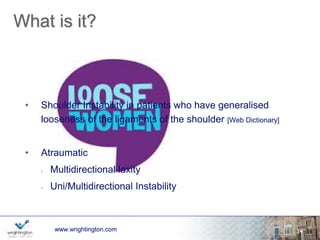
![What is it?
www.wrightington.com
12
• Shoulder Instability in patients who have generalised
looseness of the ligaments of the shoulder [Web Dictionary]
• Atraumatic
• Multidirectional laxity
• Uni/Multidirectional Instability](https://image.slidesharecdn.com/multidirectionalinstabilityoftheshoulder2014-141020004508-conversion-gate02/85/Multidirectional-instability-of-the-shoulder-2014-11-320.jpg)