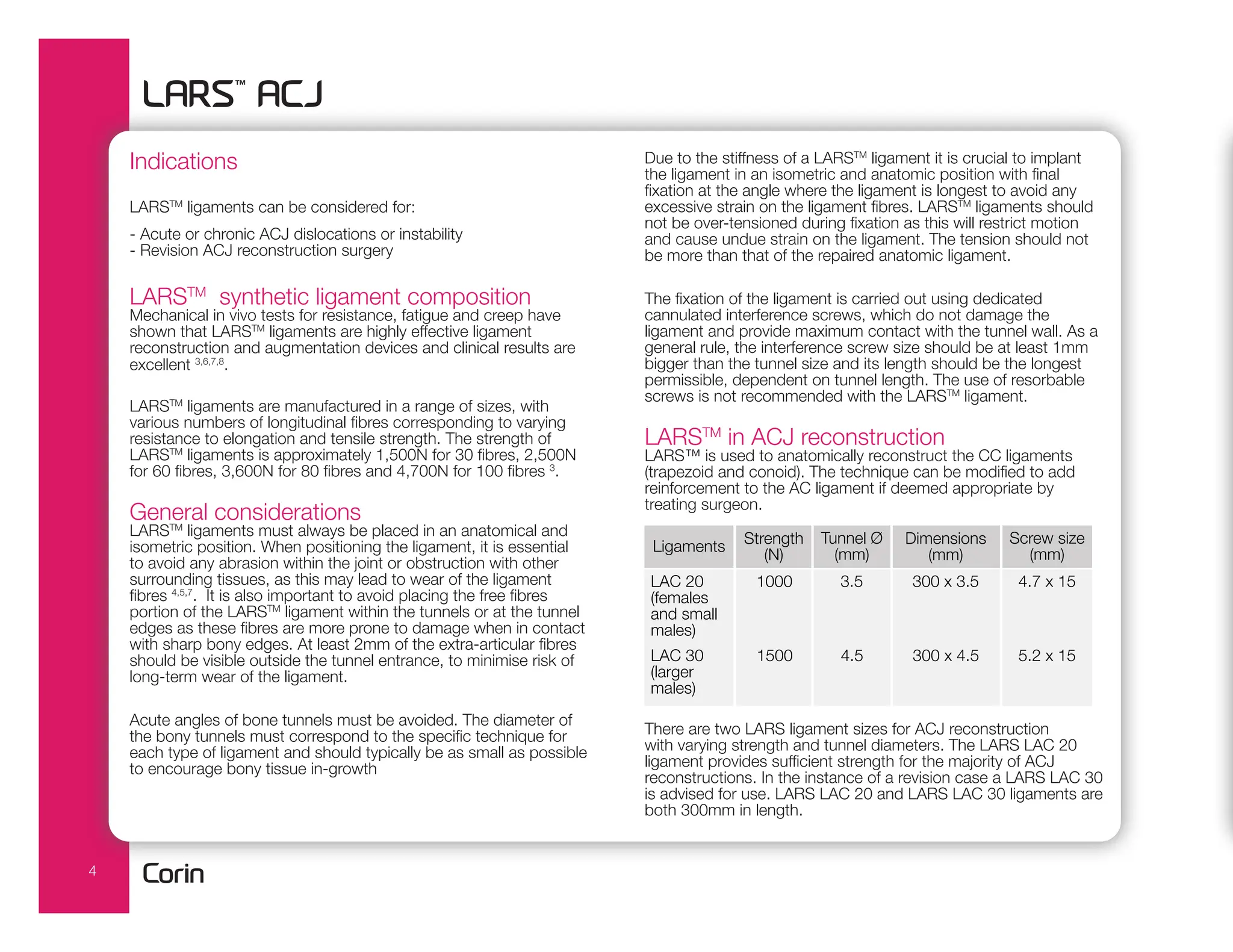
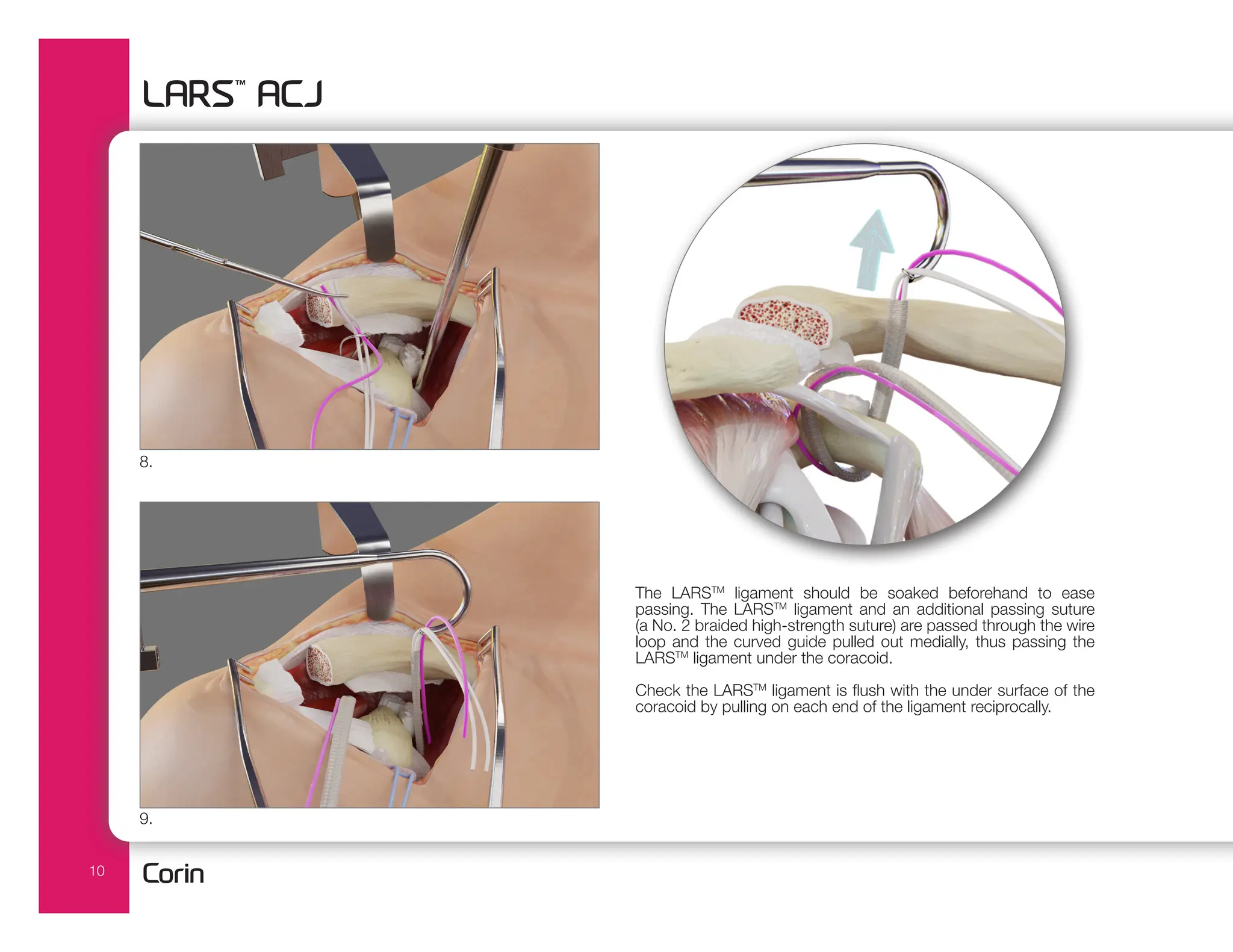
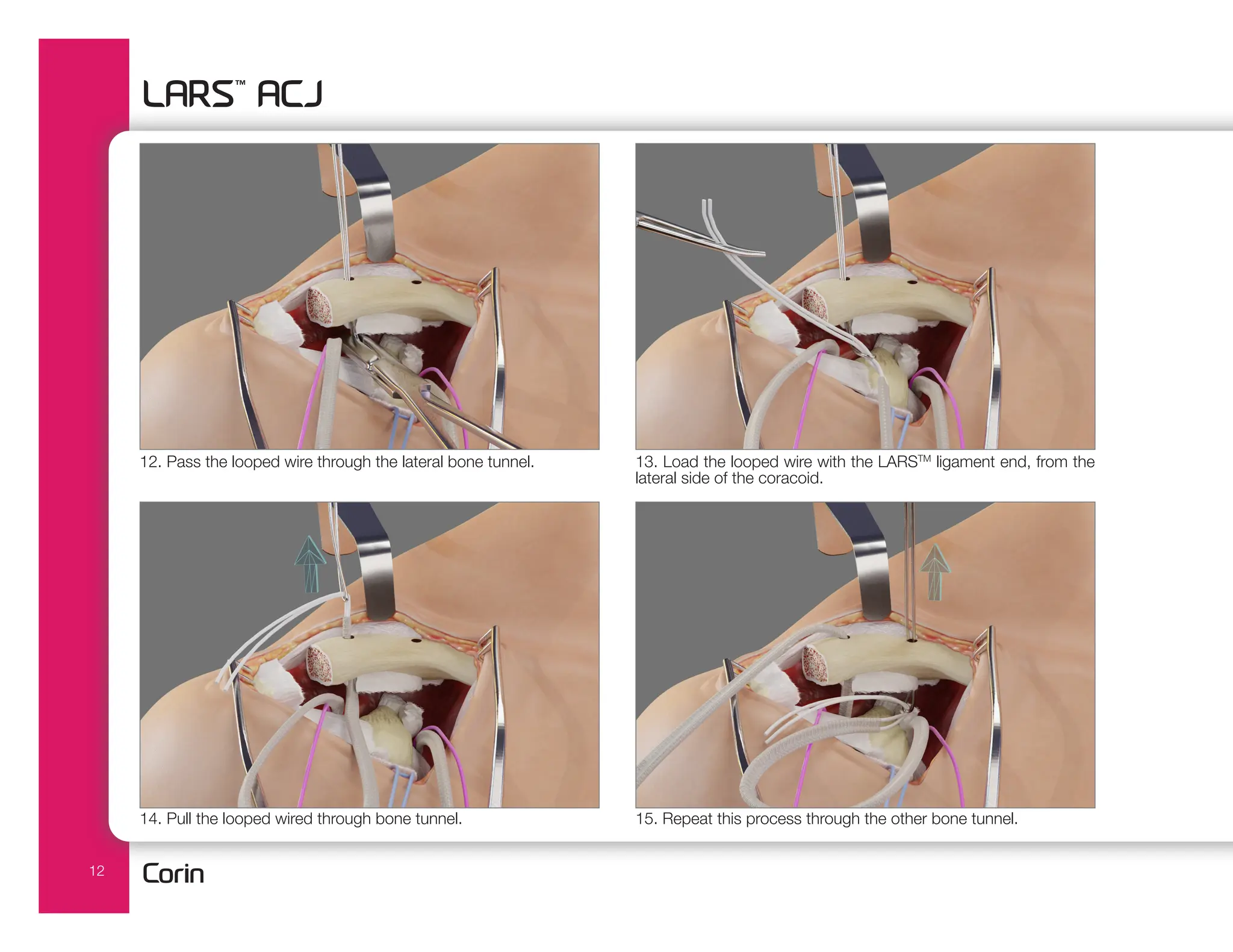
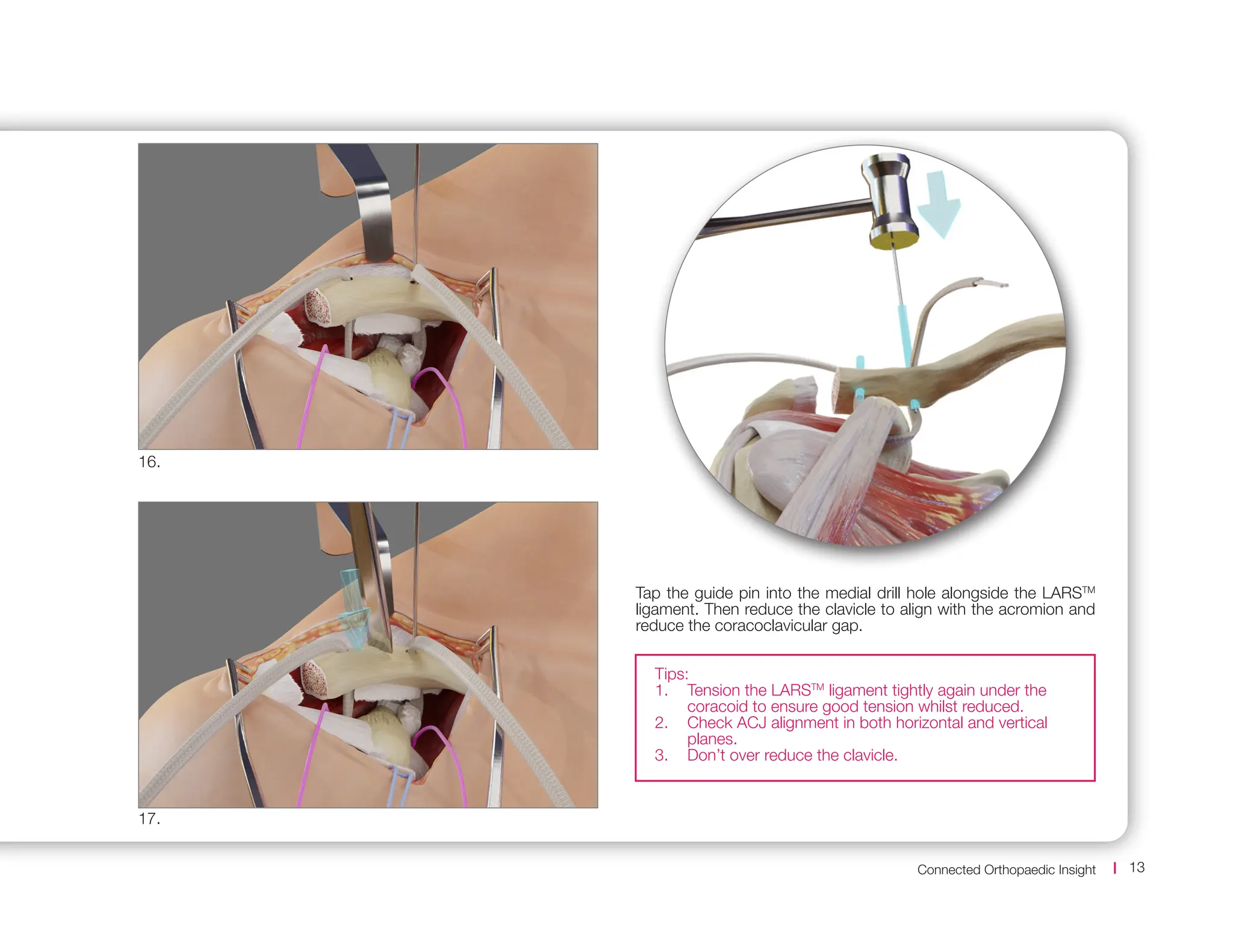
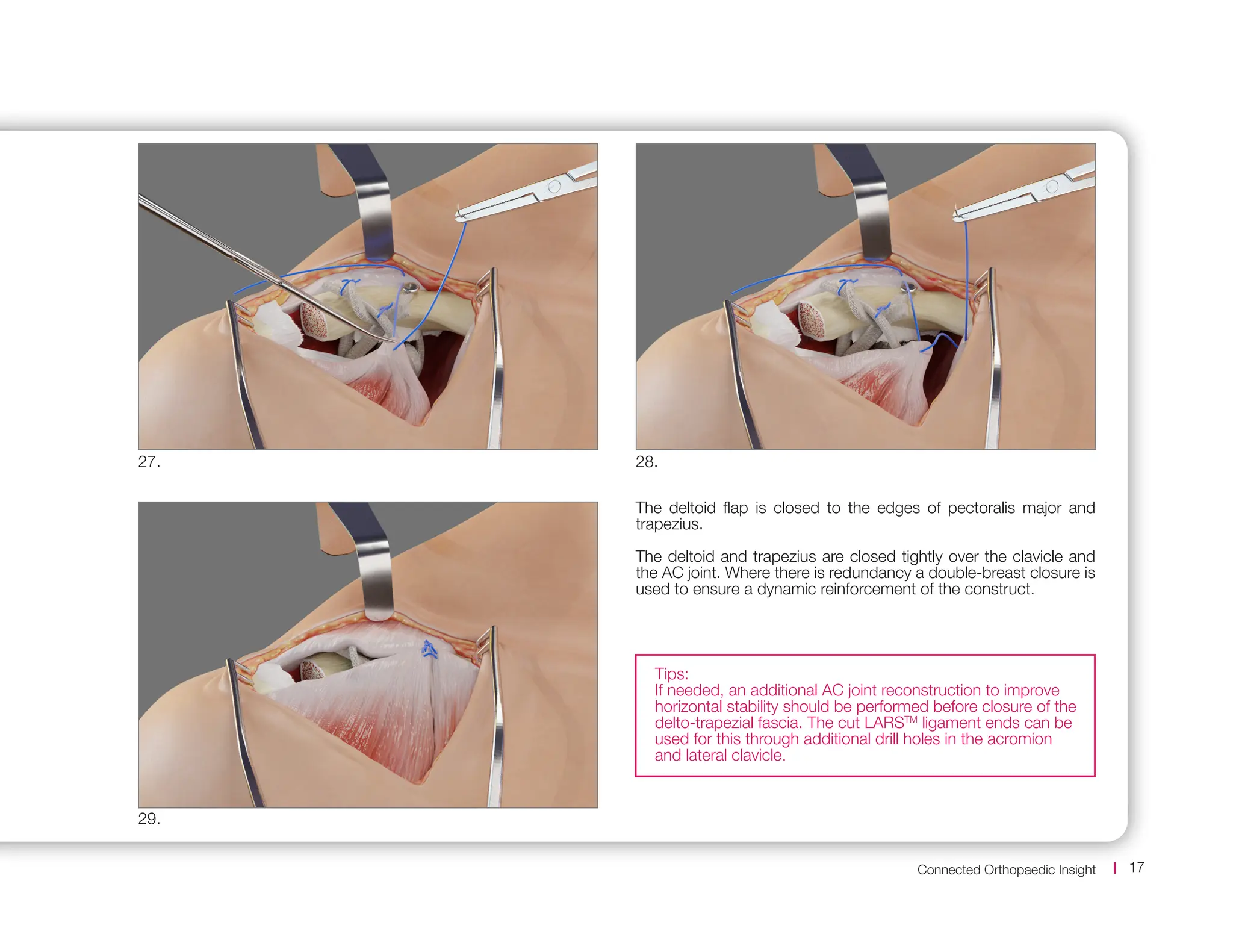
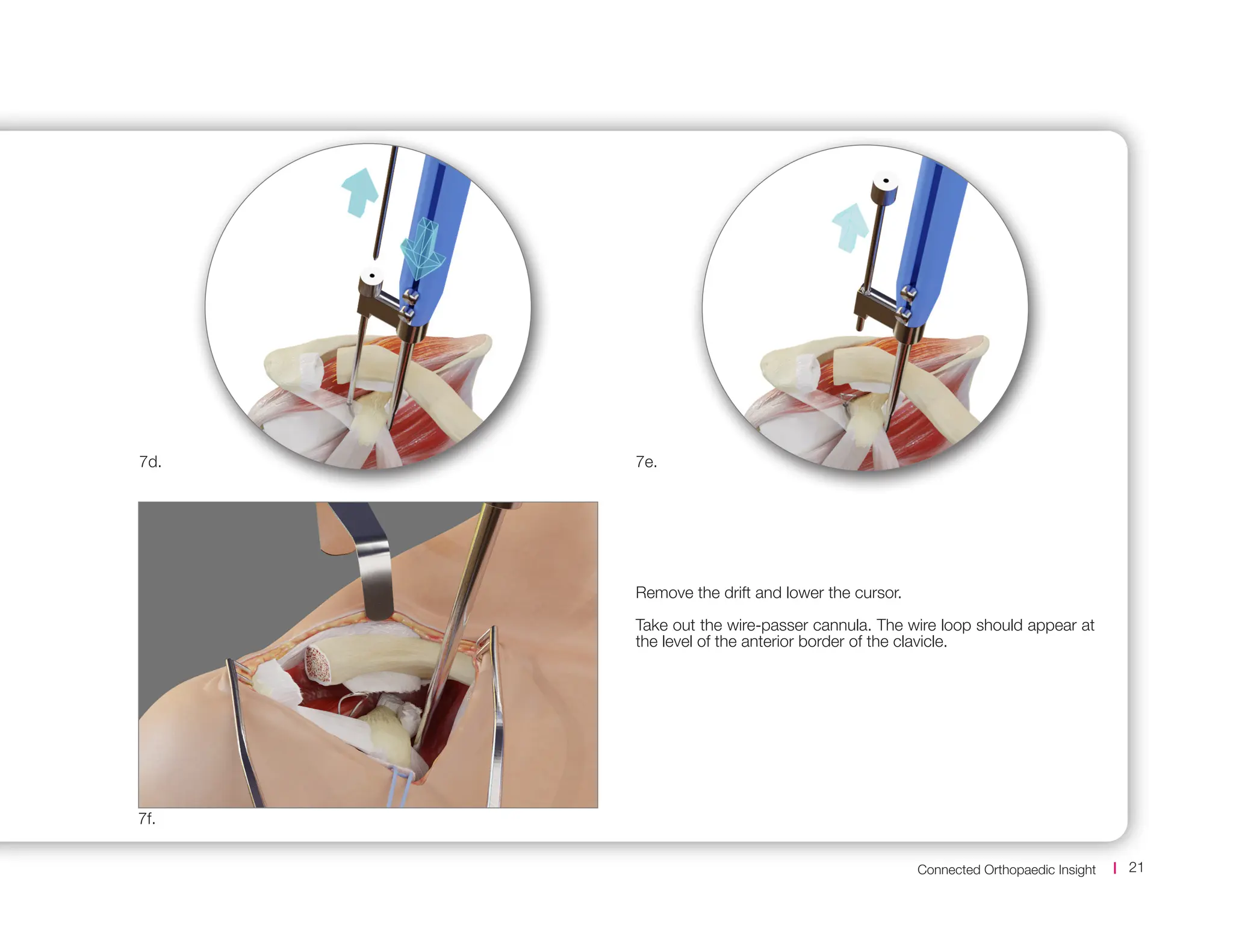
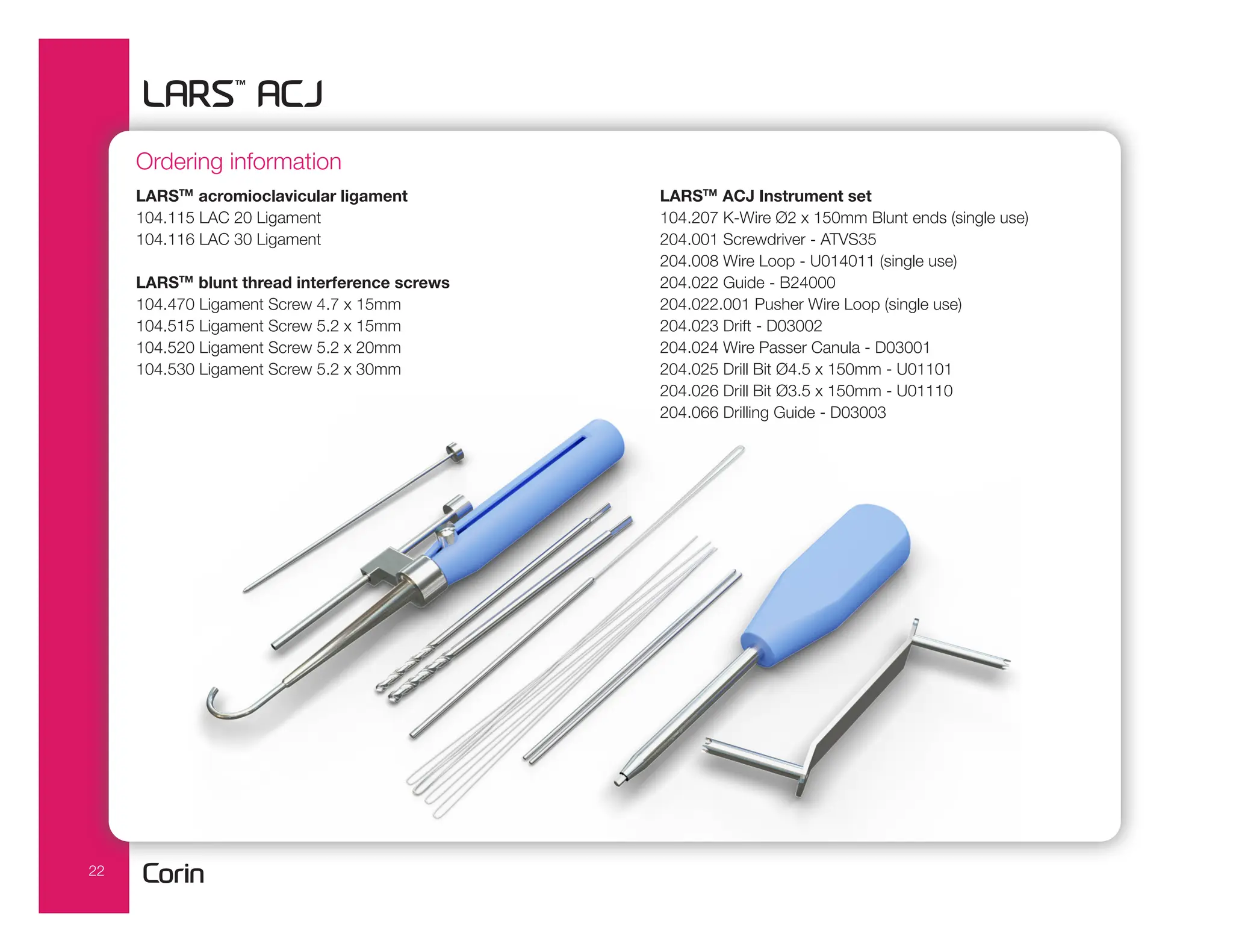
The document outlines the larstm ligament, a synthetic device designed for acromioclavicular (ACJ) reconstruction and augmentation. It details surgical techniques, indications for use, and the mechanical properties of the ligaments, emphasizing their effectiveness in restoring shoulder function. The document also provides specific procedural guidelines and considerations for surgeons to ensure proper placement and fixation during surgery.