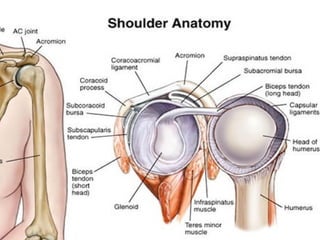
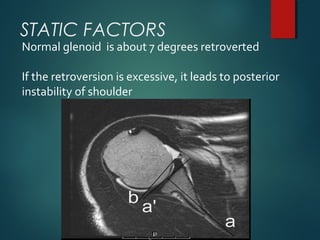
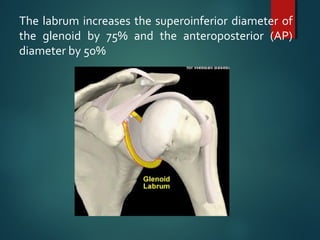
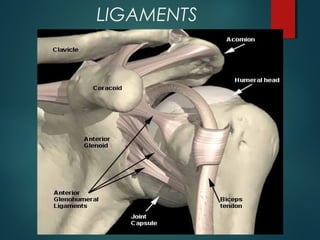
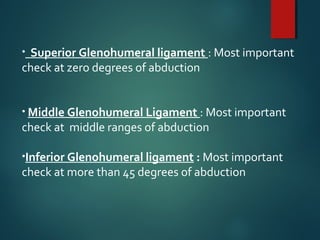
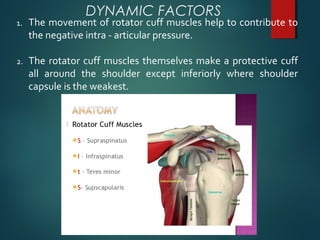
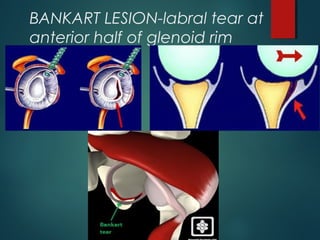
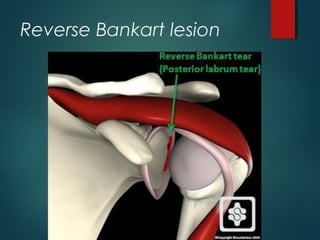
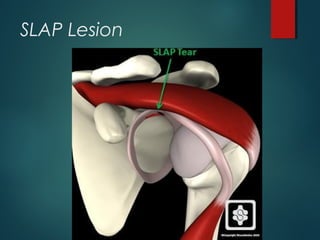
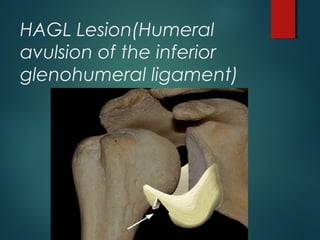
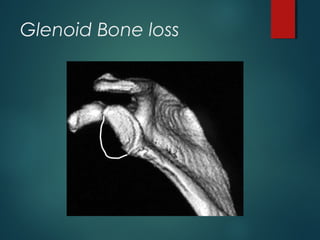
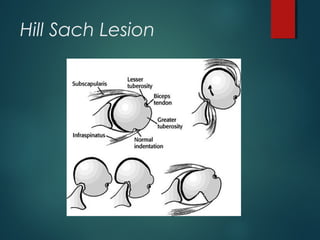
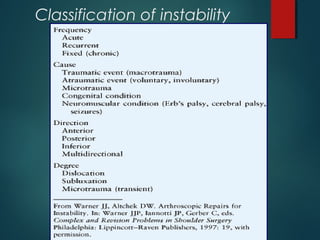
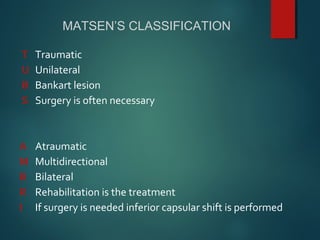
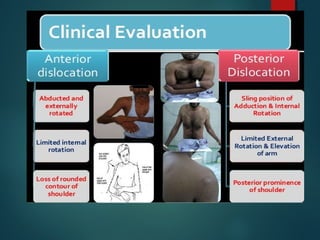
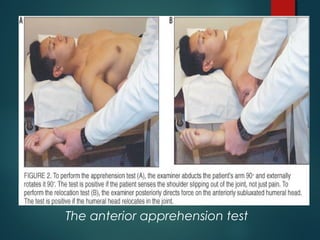
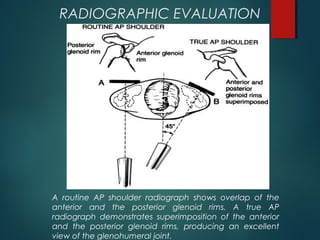
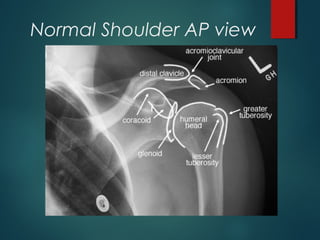
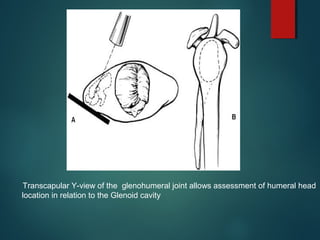
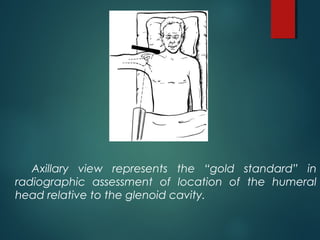
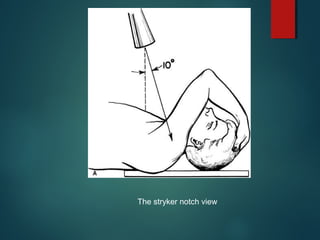
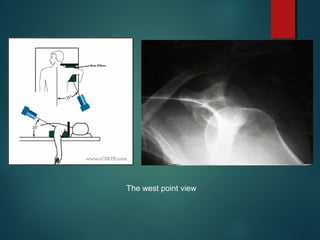
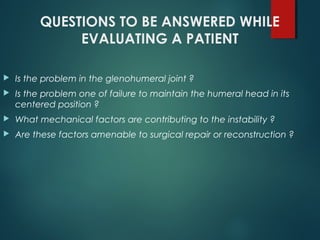
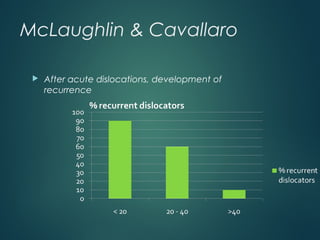
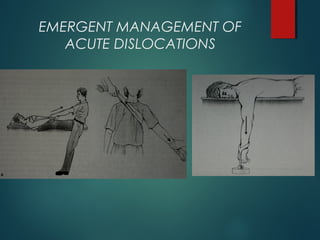
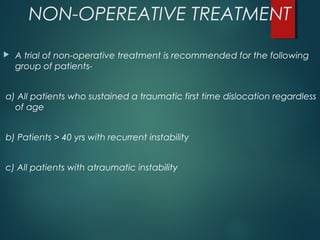
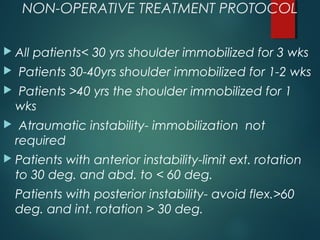
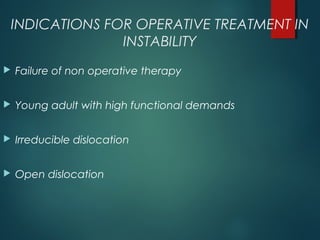
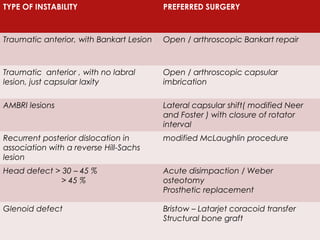
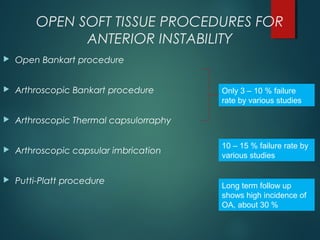
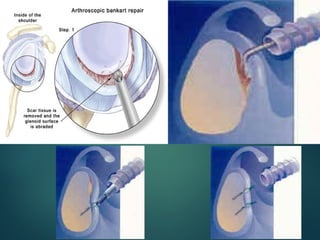
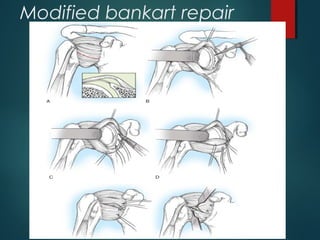
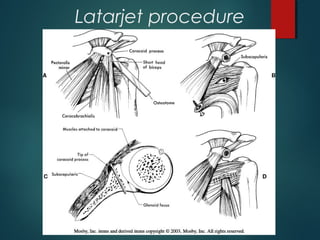
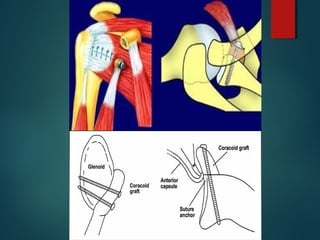
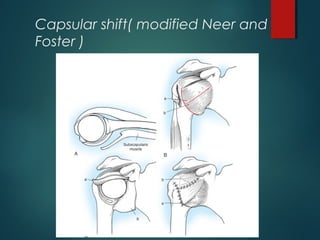
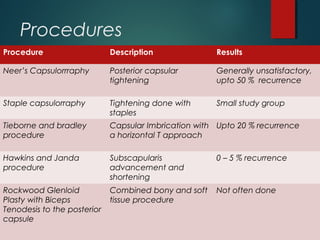
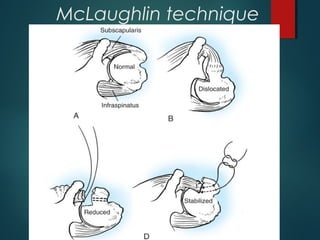
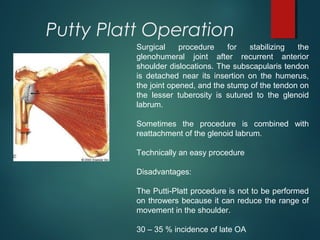
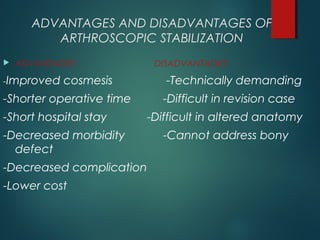
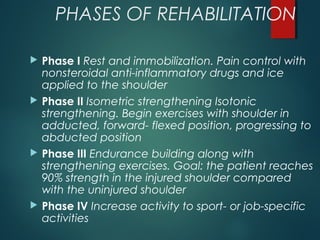
The document discusses shoulder instability, including its definition, causes, clinical presentation, evaluation, and treatment options. Static factors like bony anatomy and ligaments contribute to stability, while dynamic factors include muscle forces. Pathologies include labral tears and capsular injuries. Treatment depends on factors like age, activity level, and pathology. Non-operative options include immobilization, while surgery repairs tissues like the labrum or tightens the capsule. Rehabilitation progresses from rest to strengthening and sport-specific training.