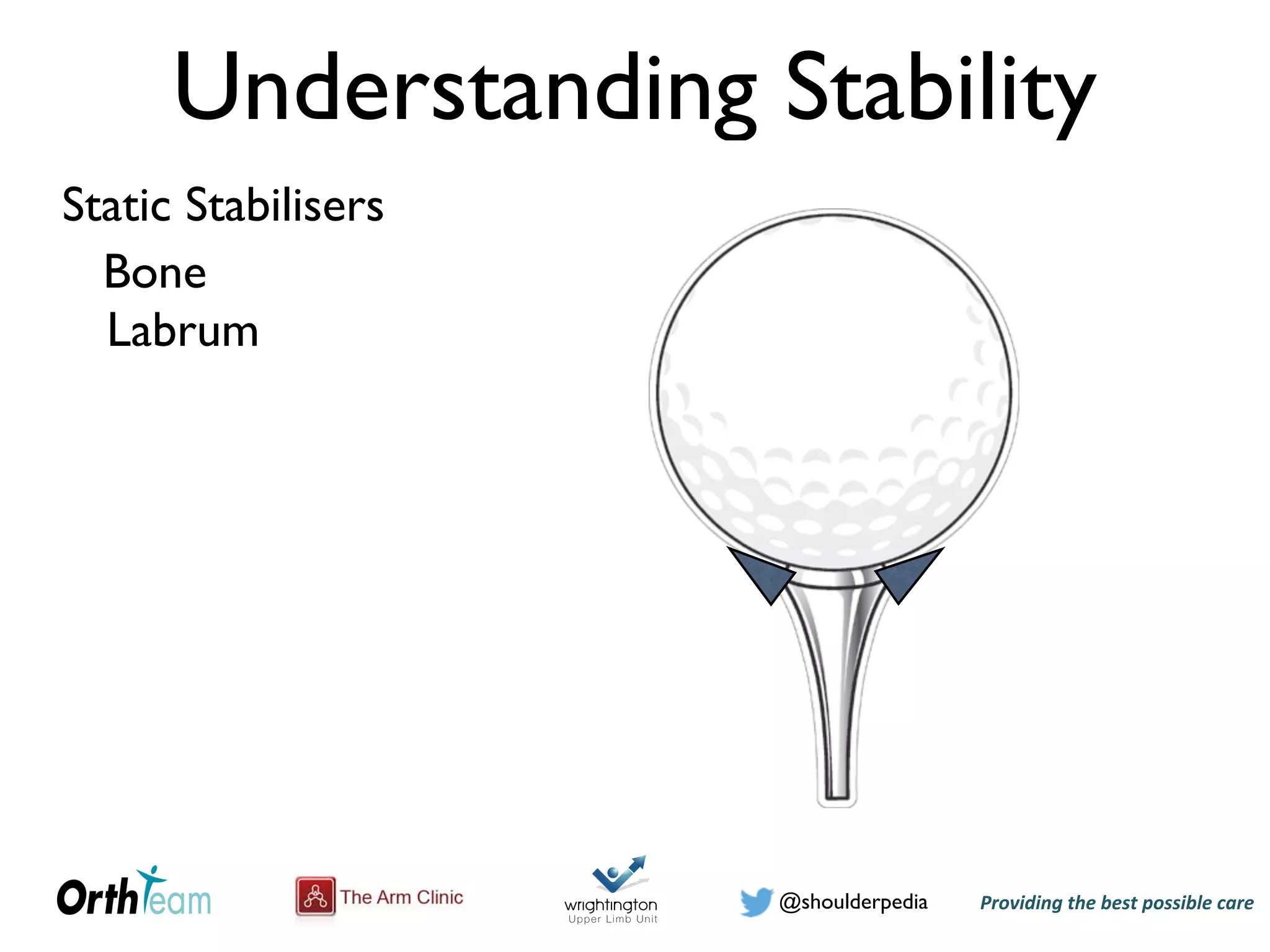
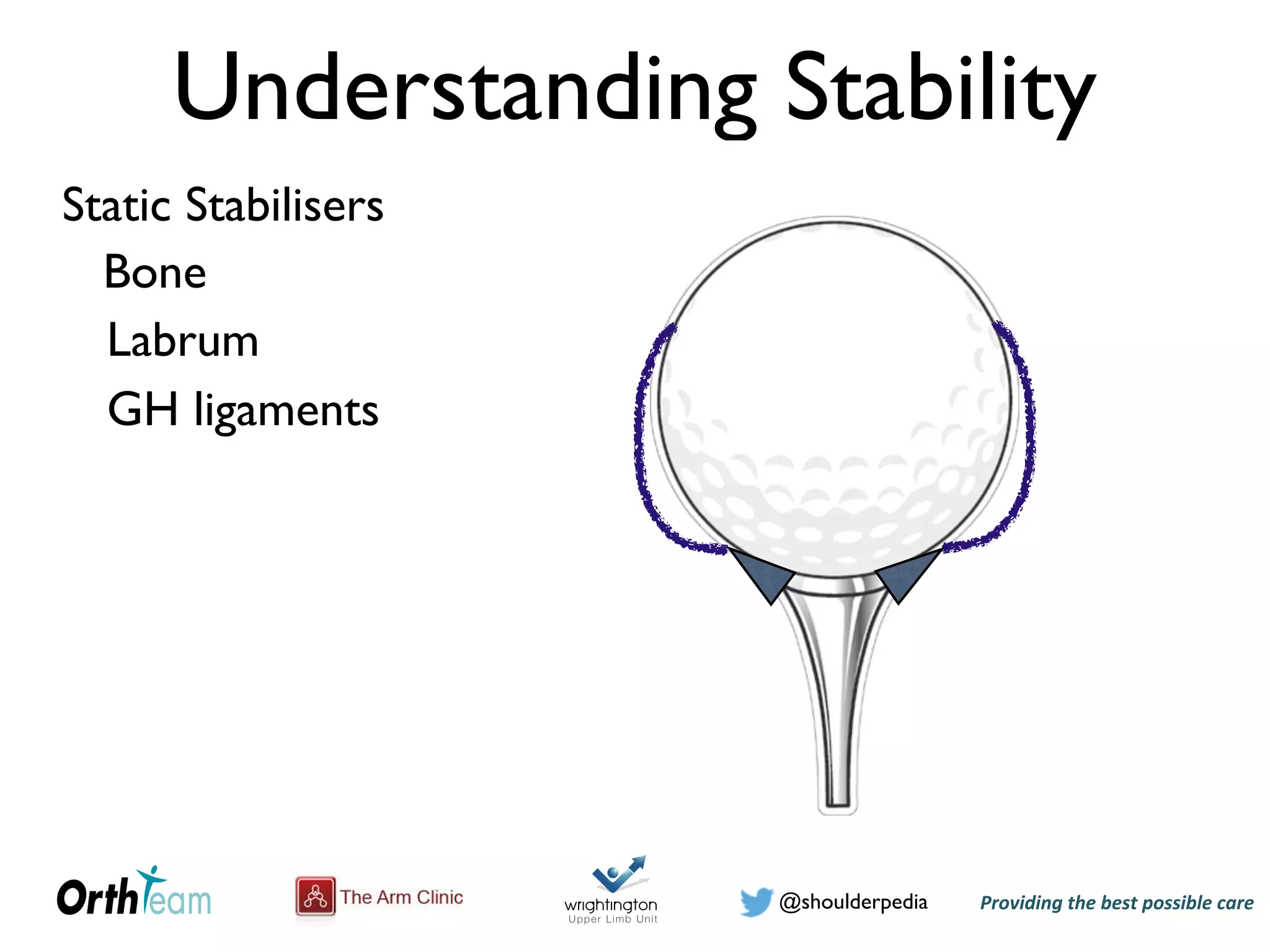
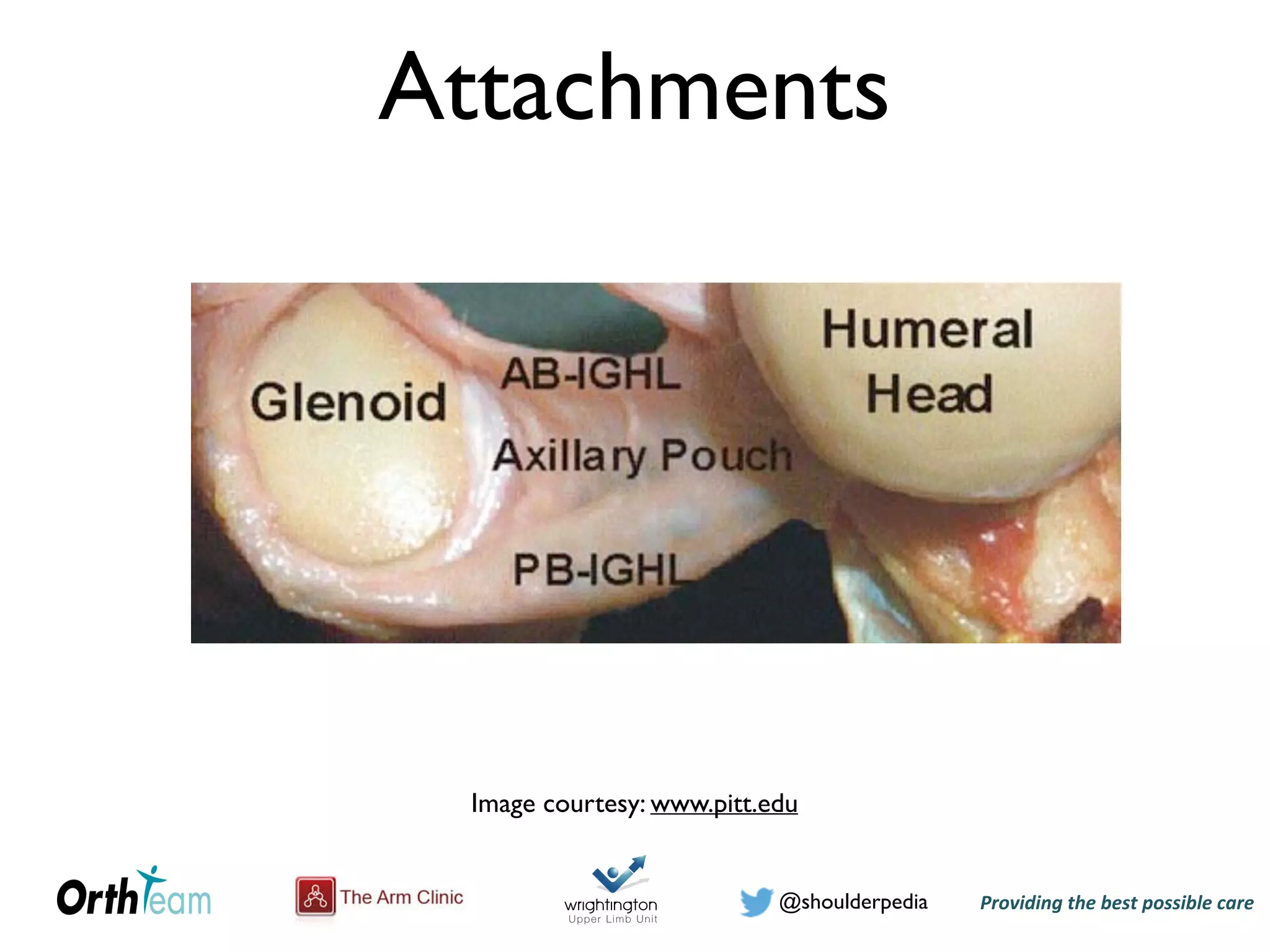
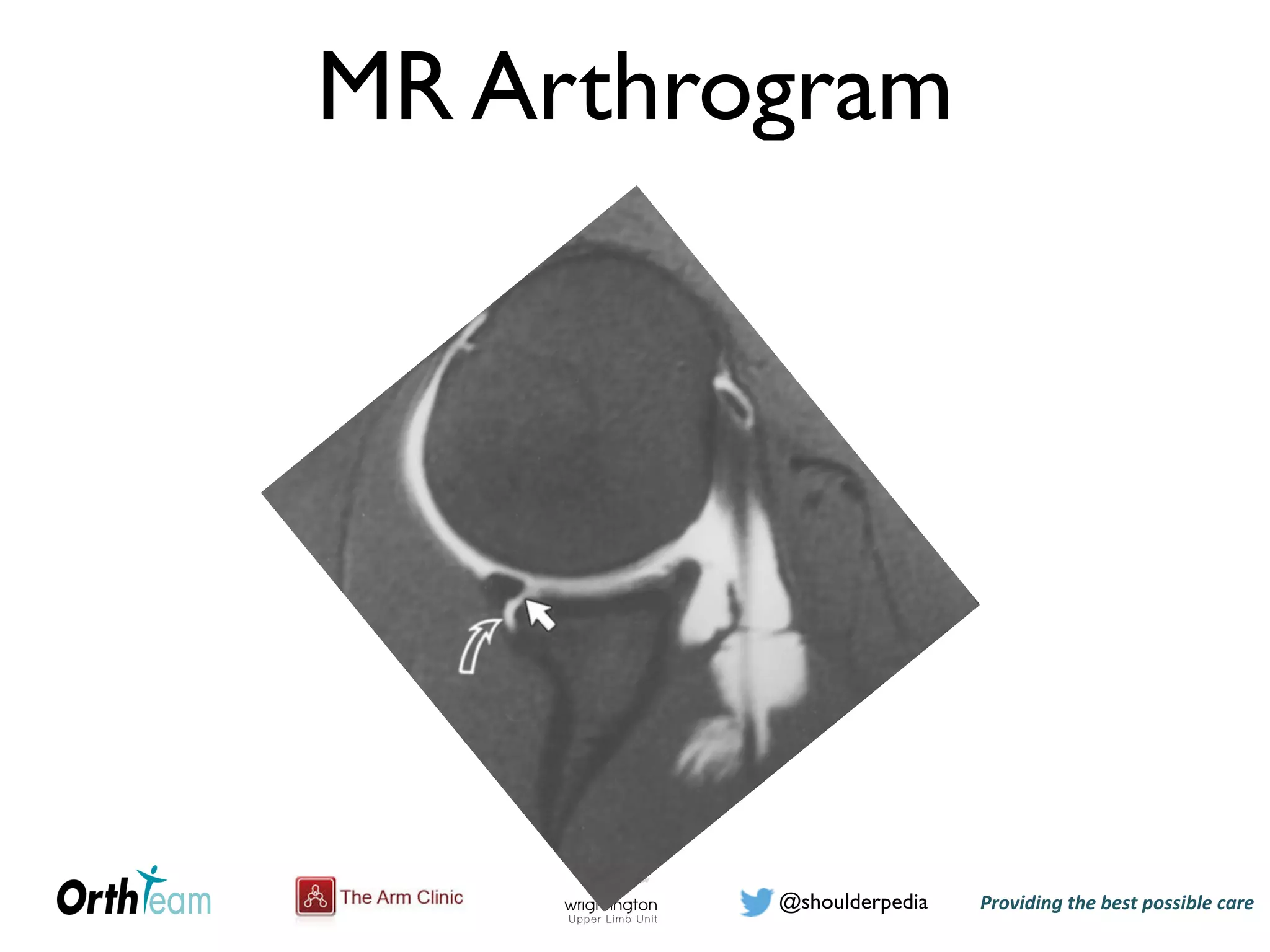
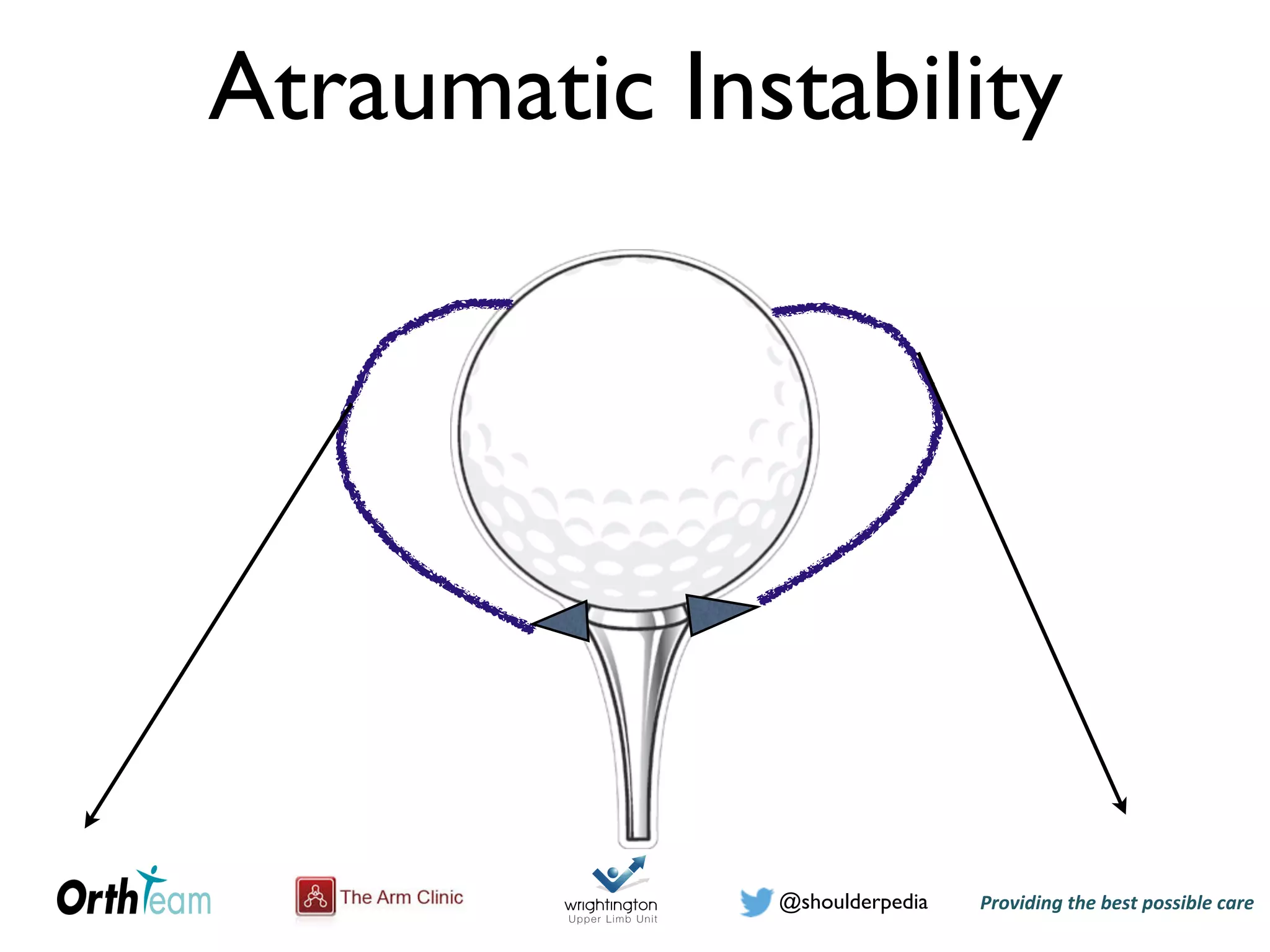
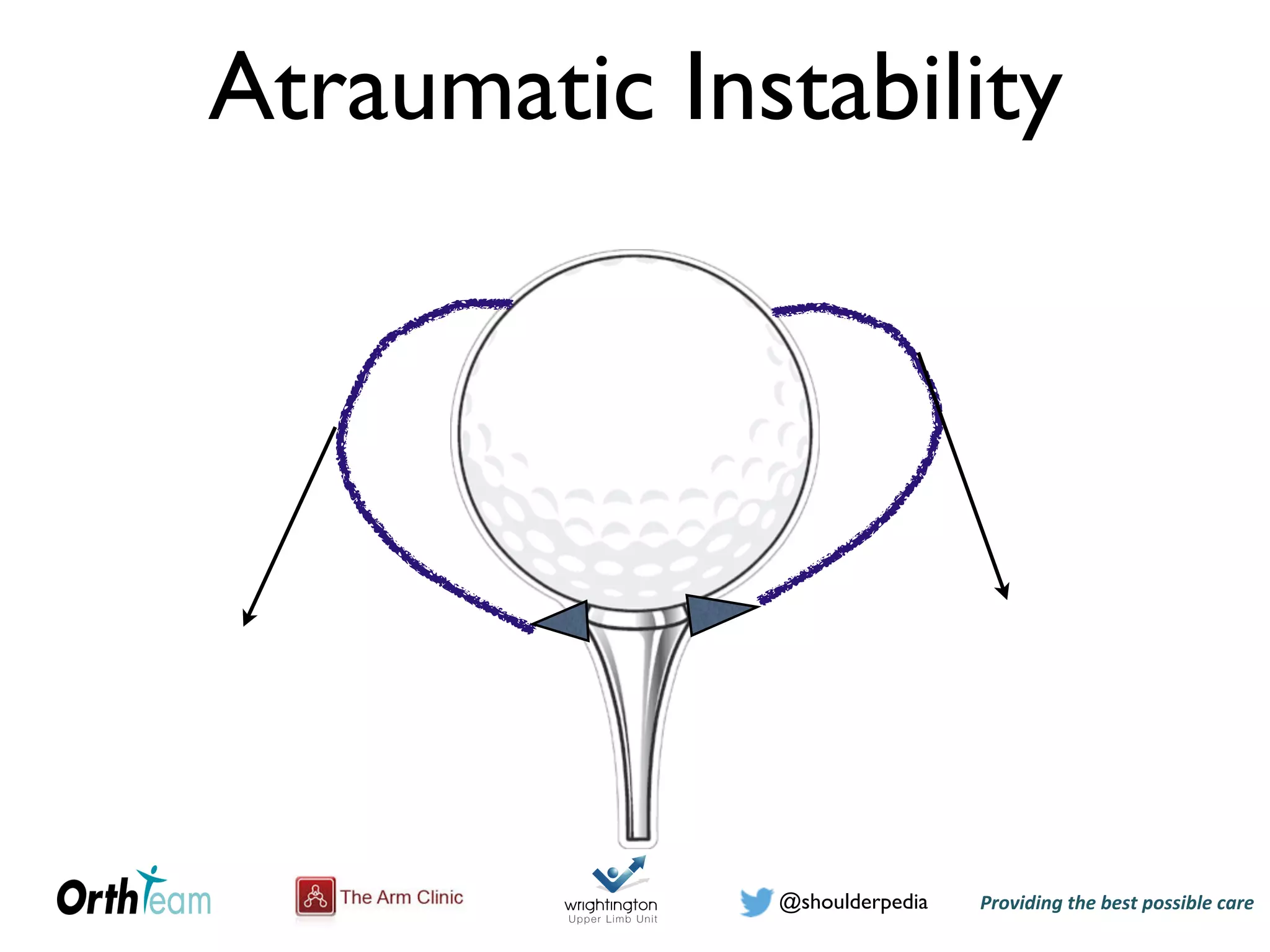
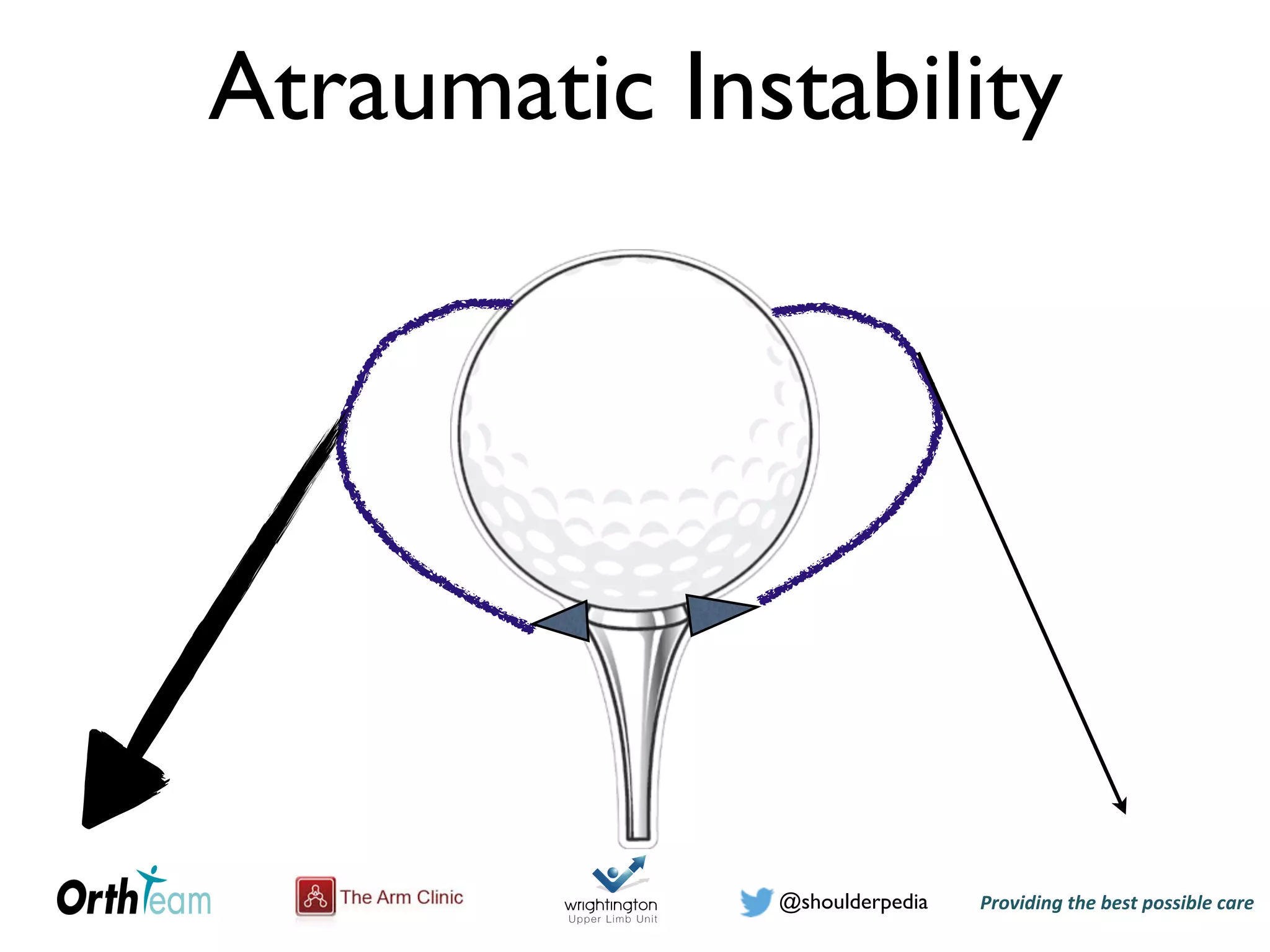
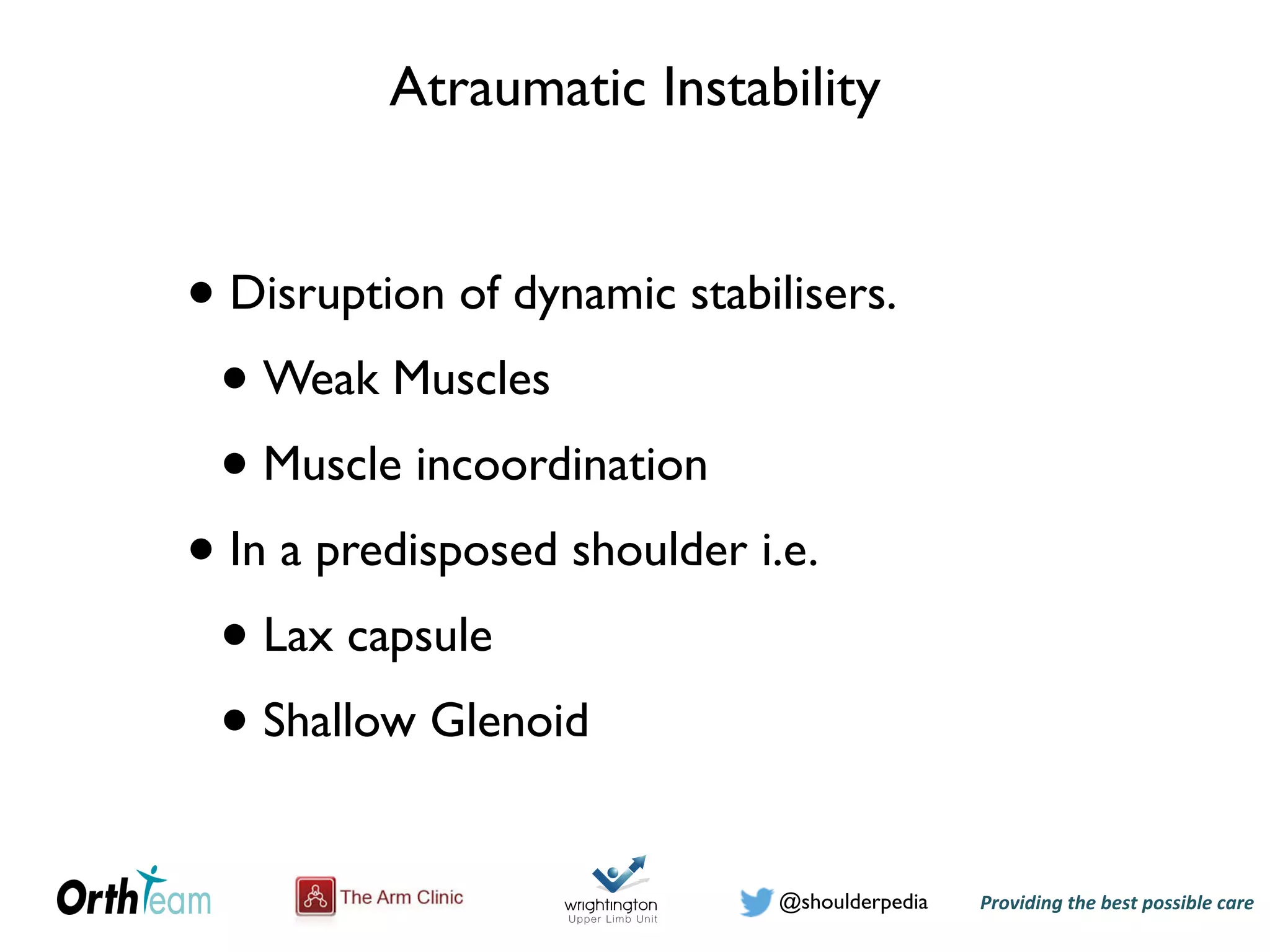
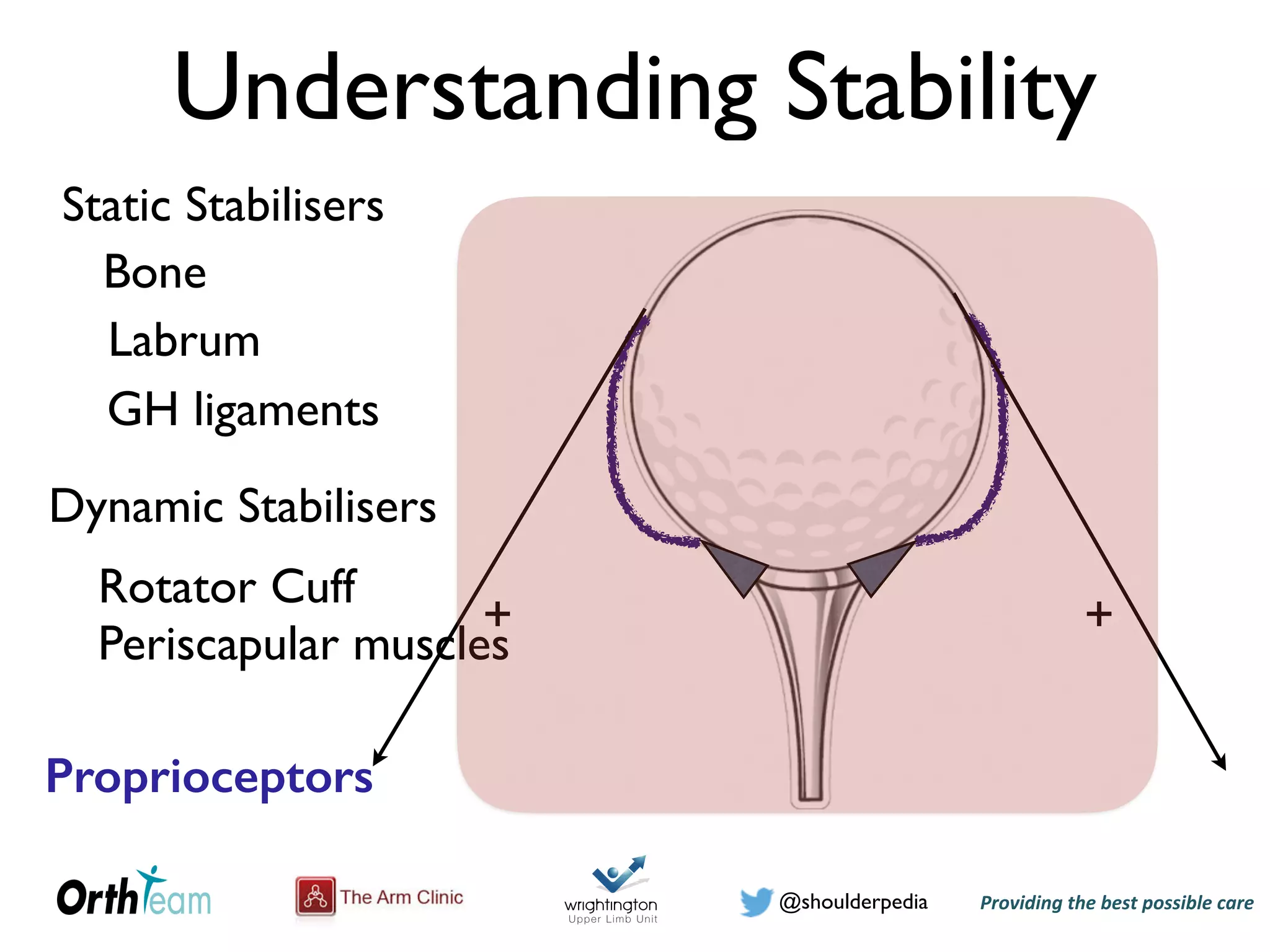
The document discusses atraumatic shoulder instability, providing 4 scenarios of 16-year-old girls with unstable shoulders. It describes how to differentiate instability from hyperlaxity and covers the static and dynamic stabilizers of the shoulder. The clinical assessment of atraumatic instability includes assessing contributions from the traumatic history, structural factors like the sulcus sign, and range of motion tests like the Gagey sign. Classification systems for instability including Rockwood and Stanmore are presented.