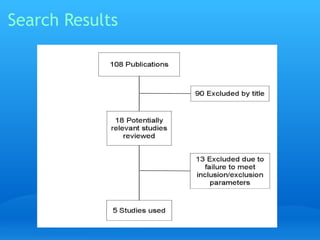
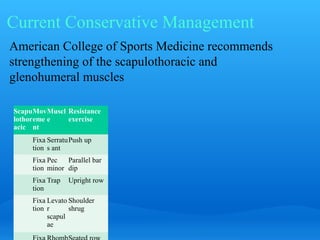
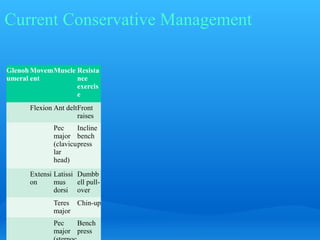
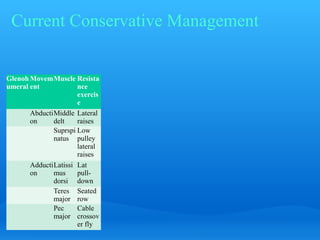
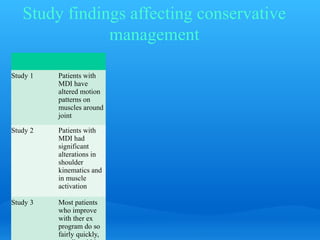
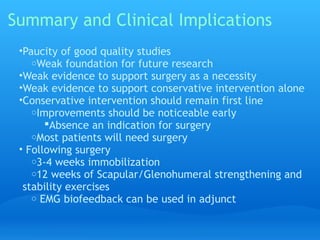
The document summarizes key studies on the effectiveness of conservative treatment for multidirectional instability (MDI). Three studies found that conservative treatment including strengthening exercises improved some outcomes like muscle activation patterns and kinematics, but did not fully restore shoulders to normal. One study found that after 8 years, only 30% of patients had good results with conservative treatment alone. Overall, the studies suggest that while conservative treatment can provide some benefits for MDI, surgery may be needed for full resolution of symptoms for many patients.