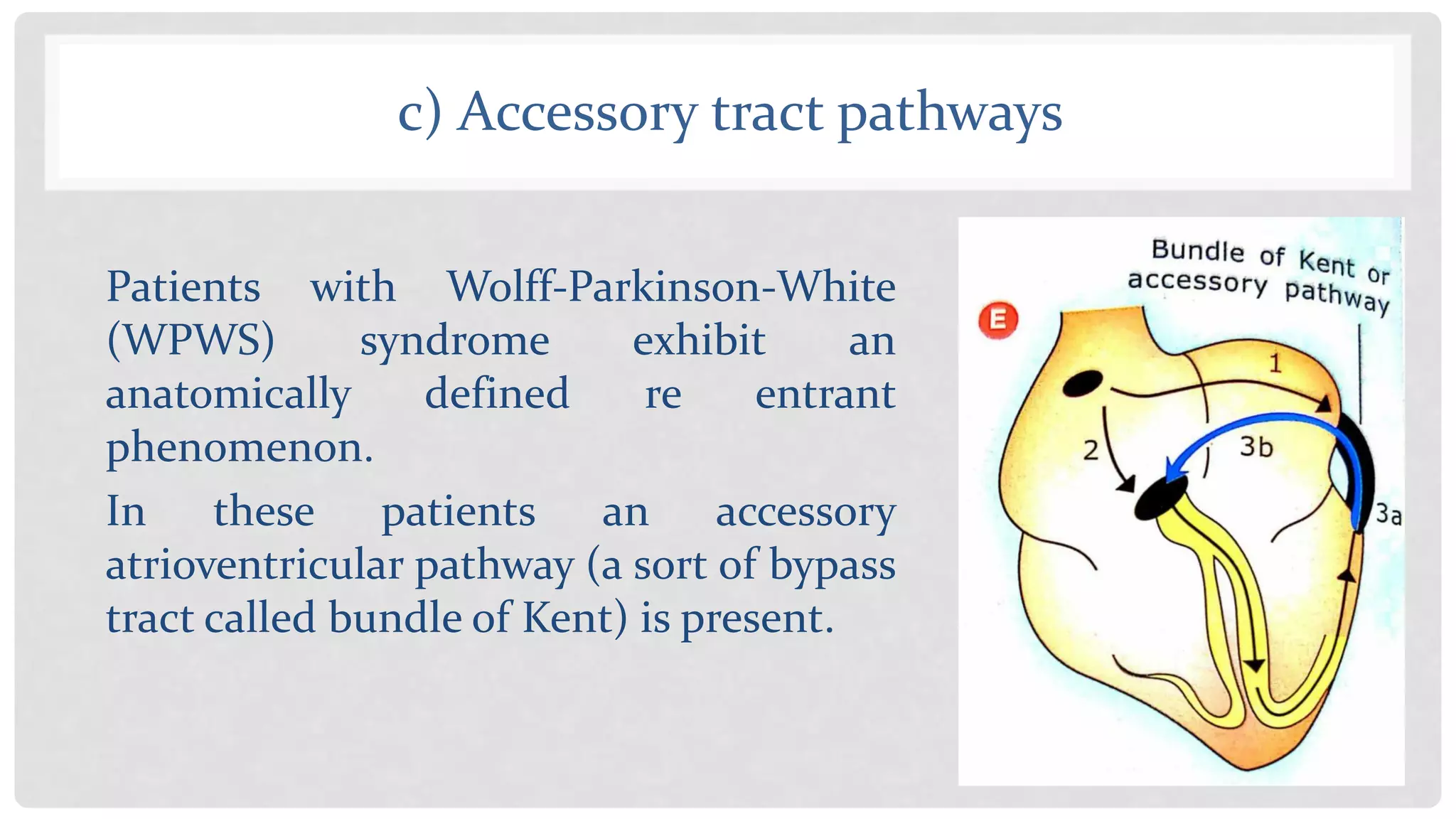
Cardiac arrhythmias refer to irregularities in heart rhythm and can be caused by abnormalities in impulse generation, conduction, or triggered activity. Bradyarrhythmias result from issues with the sinoatrial or atrioventricular nodes and can be treated with pacemakers, while tachyarrhythmias can often be managed with drugs. There are three main mechanisms for arrhythmias - abnormal impulse generation from altered automaticity, triggered activity due to afterdepolarizations, and abnormal impulse conduction from blocks, reentry phenomena, or accessory pathways. Antiarrhythmic drugs work to suppress enhanced automaticity or abolish reentry by slowing conduction.