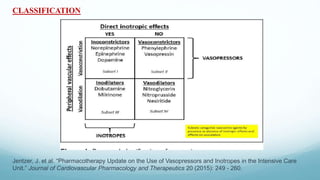
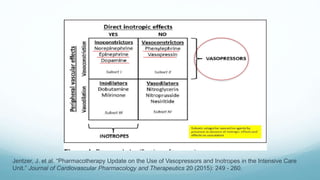
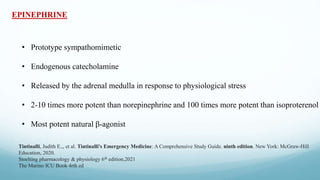
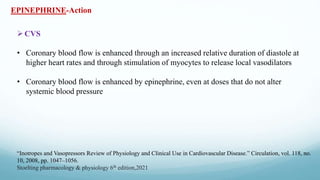
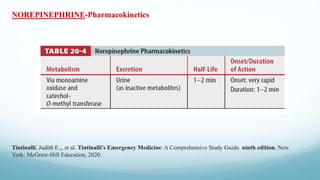
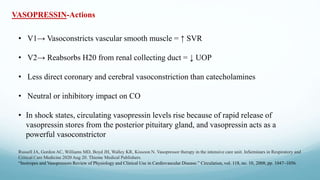
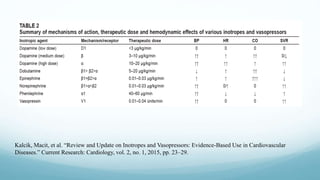
Vasopressors and inotropes are commonly used in the intensive care unit to treat low blood pressure and cardiac dysfunction. This document discusses the physiology and clinical use of various agents. It defines vasopressors as agents that increase vascular tone and blood pressure, while inotropes increase myocardial contractility. Common vasopressors described include norepinephrine, phenylephrine, vasopressin, and epinephrine. The document outlines key principles for the rational use of vasopressors, such as correcting hypovolemia first, titrating the dose based on blood pressure and organ perfusion targets, and considering an agent's effects on various receptor subtypes. Practical issues are also reviewed