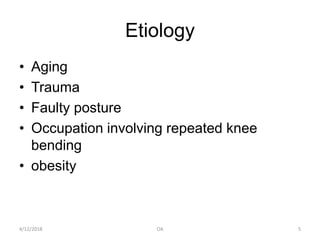
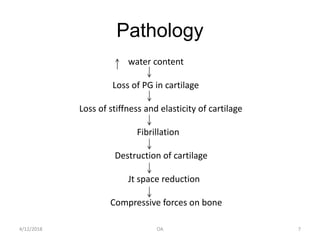
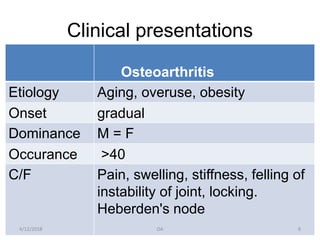
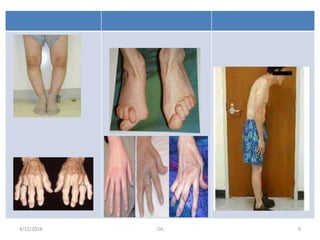
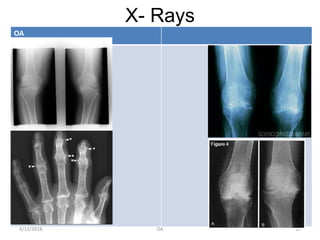
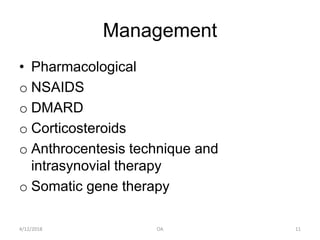
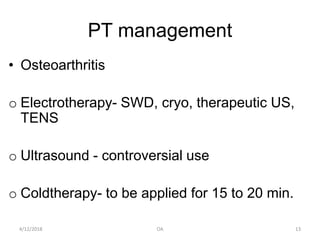
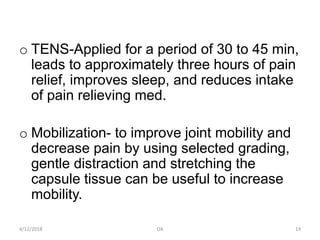
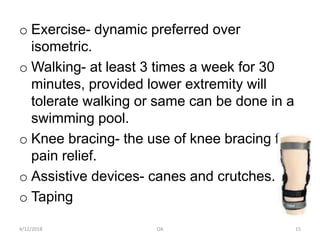
This document discusses osteoarthritis (OA), which is characterized by the progressive destruction of cartilage in joints followed by bone changes. It is the most common form of arthritis. Risk factors include aging, joint injury, poor posture, overuse, and obesity. Symptoms include pain, swelling, and stiffness in the joints that is worsened with use. Diagnosis is made based on symptoms and confirmed with x-rays showing bone changes and loss of cartilage. Treatment includes medications like NSAIDs, physical therapy focusing on exercises, bracing, and lifestyle modifications like weight loss.