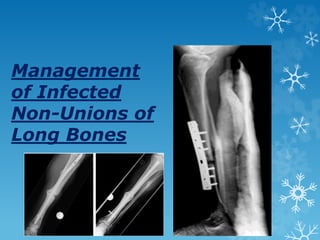
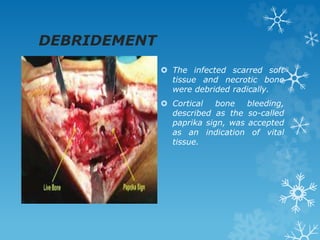
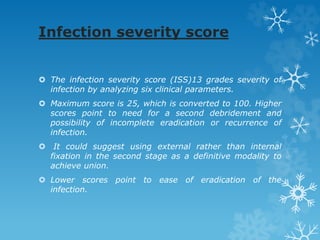
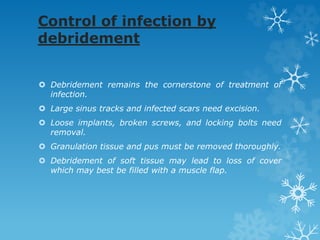
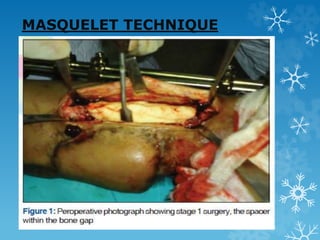
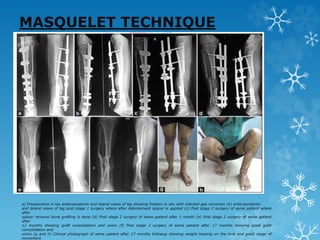
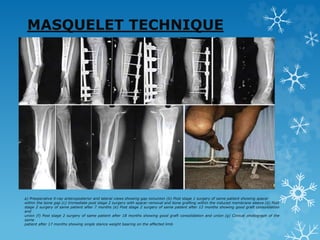
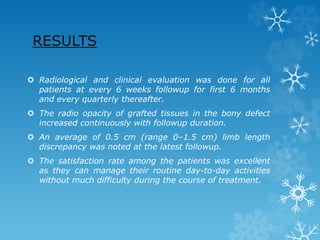
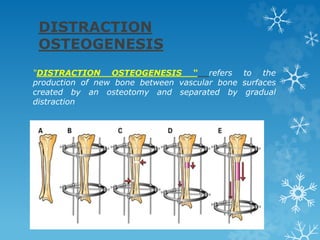
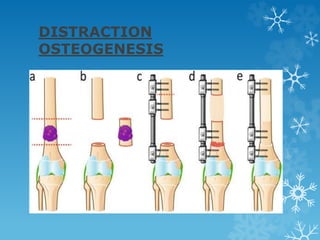
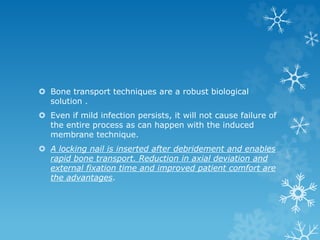
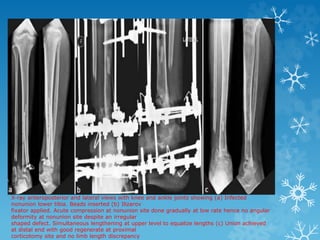
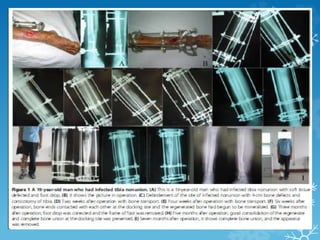
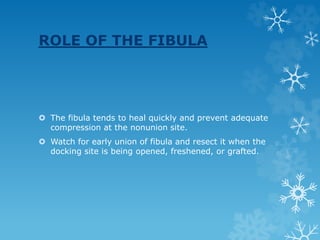
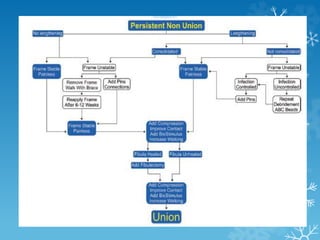
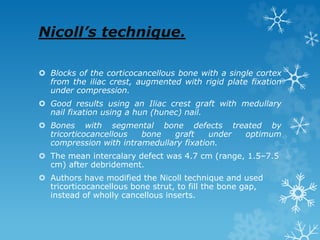
This document discusses the management of infected non-unions of long bones. It states that bone union requires stable fixation, biological stimulation, and restored function. For infected non-unions, the treatment is to first eliminate the infection through thorough debridement. Several surgical treatment options are then discussed to achieve union, including bone grafting, the induced membrane technique, antibiotic cement, and the Ilizarov method. The induced membrane technique involves creating a membrane through the use of a cement spacer that can later house bone grafts to achieve union.