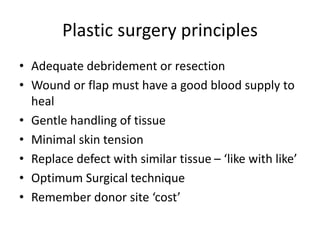
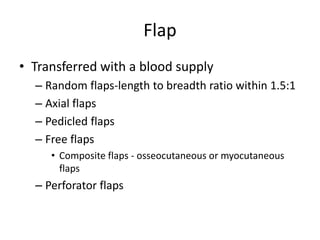
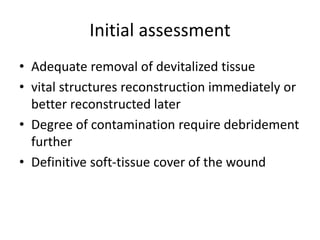
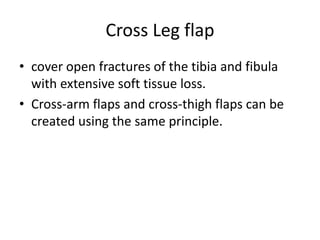
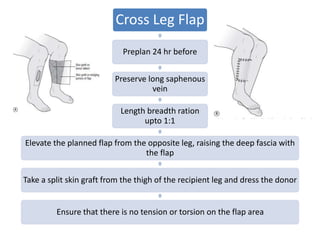
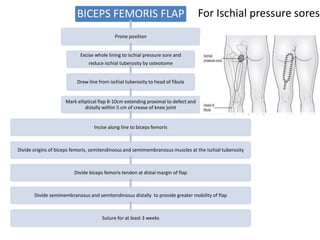
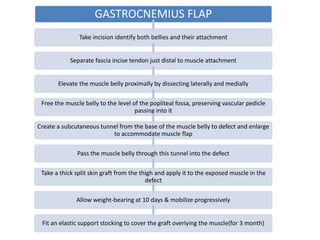
This document provides an overview of plastic and reconstructive surgery techniques. It discusses various types of grafts and flaps used to manage soft tissue defects, including split thickness skin grafts, full thickness skin grafts, nerve grafts, tendon grafts, random flaps, axial flaps, pedicled flaps, and free flaps. Specific techniques are described for cross leg flaps, biceps femoris flaps, gastrocnemius flaps, soleus flaps, and peroneous brevis flaps to cover defects in the lower limbs. Key principles of plastic surgery like adequate debridement and minimal skin tension are also summarized.