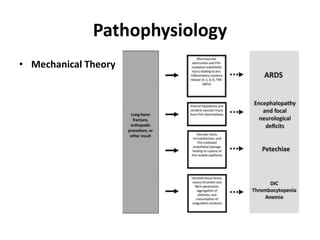
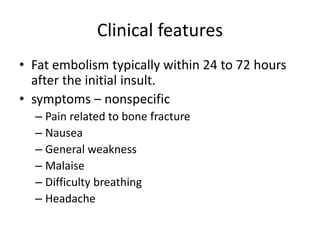
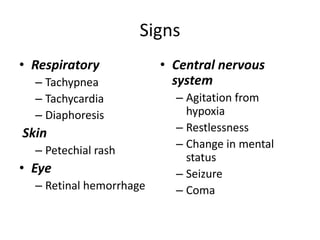
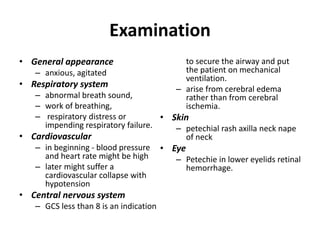
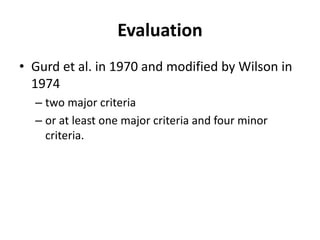
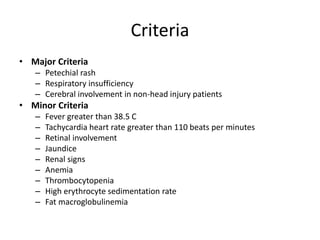
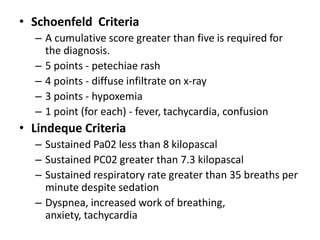
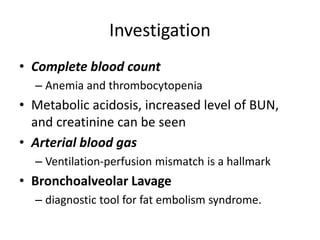
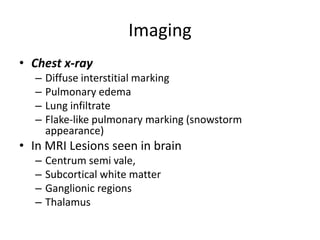
Fat embolism occurs when fat enters the bloodstream from broken bones or other injuries. It can disrupt circulation in the lungs, brain, and skin. Symptoms appear within 1-3 days and include respiratory distress, neurological changes, and a rash. Diagnosis is based on clinical criteria involving these organ systems. Treatment focuses on supportive care like oxygen supplementation, ventilation if needed, and managing complications. Outcomes have improved but risks of ARDS and cerebral edema remain.