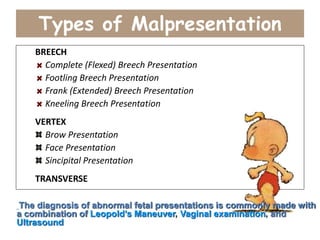
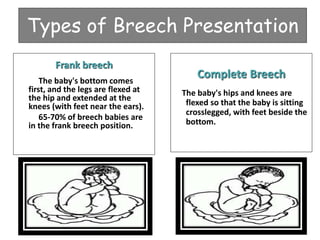
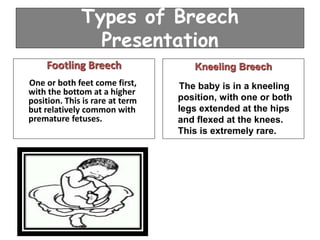
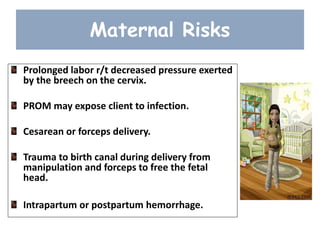
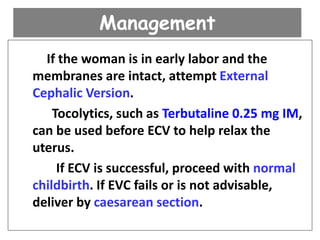
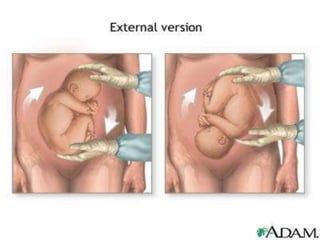
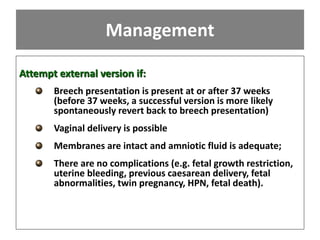
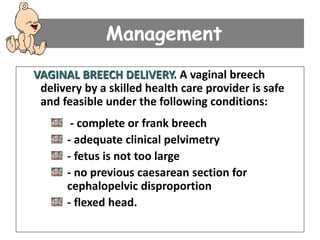
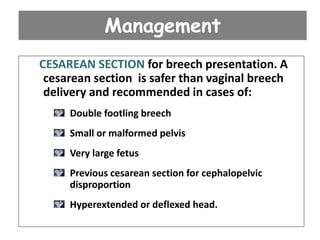
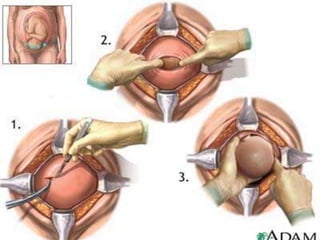
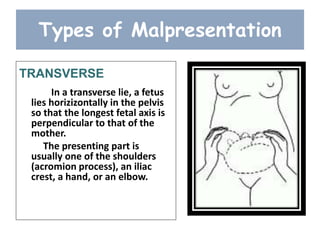
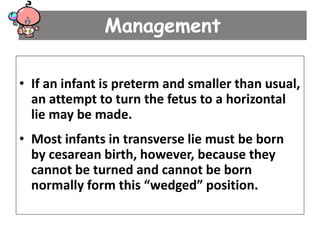
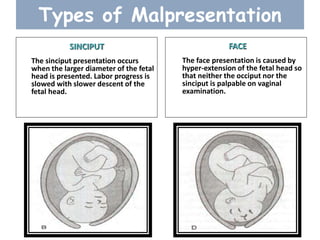
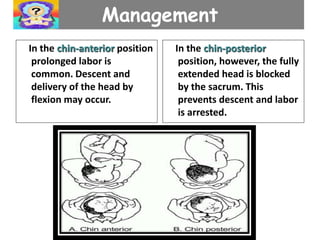
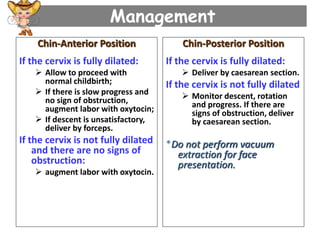
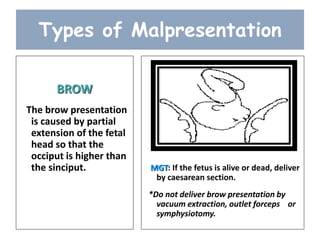
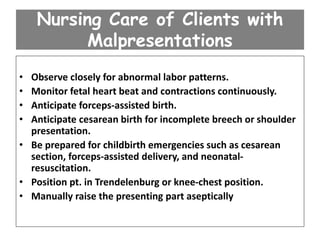
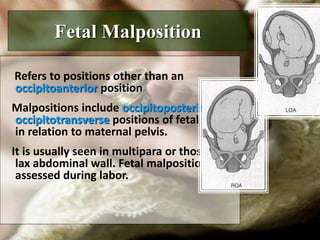
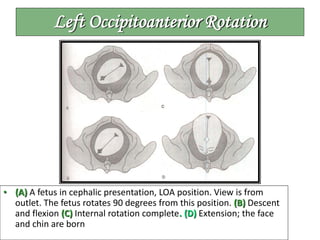
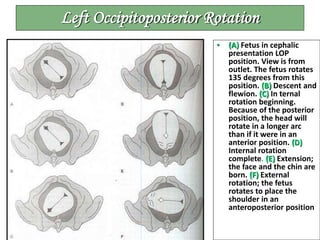
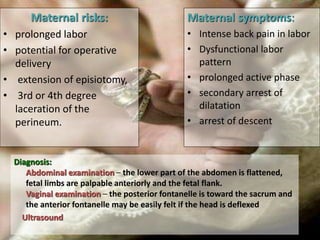
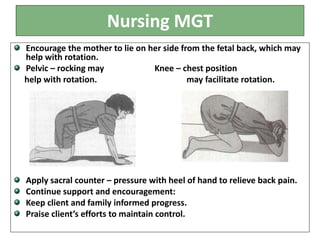
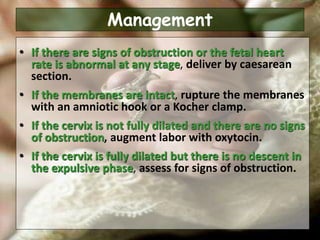
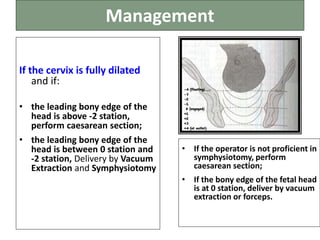
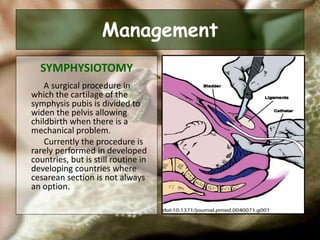
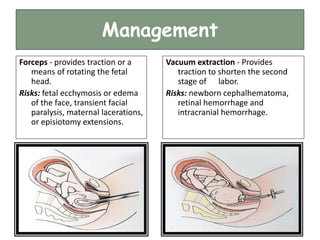
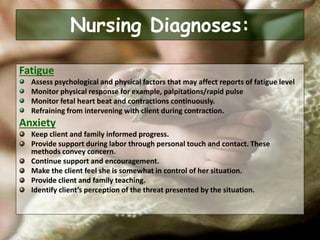
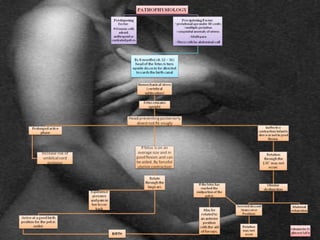
This document discusses fetal malpresentation and malposition, which refer to abnormal positions of the fetus within the uterus. Fetal malpresentation means any position other than vertex, such as breech or transverse lie. Malposition refers to positions other than occiput anterior, such as occiput posterior or occiput transverse. Types and management of different malpresentations and malpositions are described, along with risks to mother and fetus. Nursing care focuses on close monitoring for abnormal labor, supporting the mother physically and emotionally, and preparing for potential operative delivery.