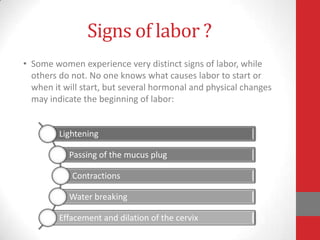
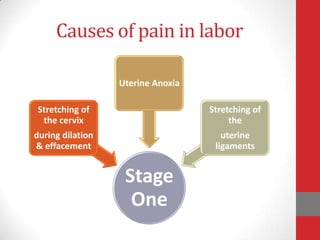
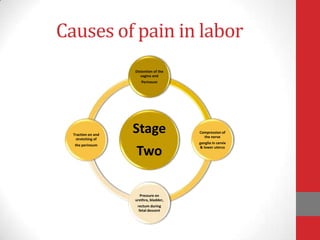
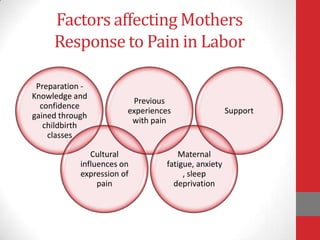
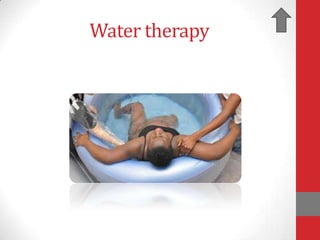
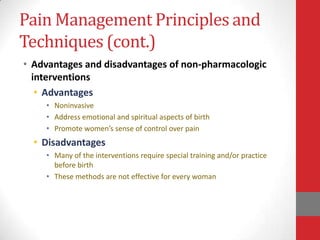
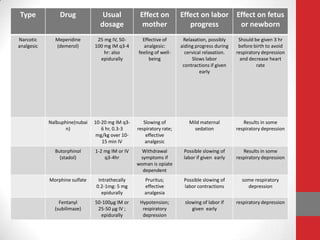
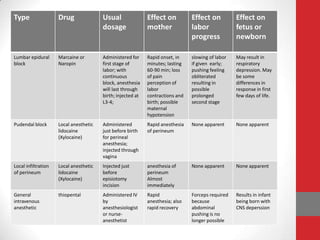
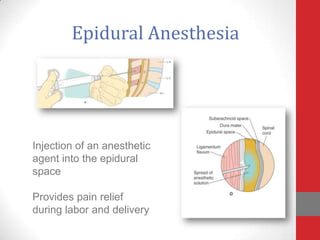
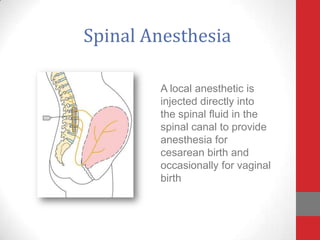
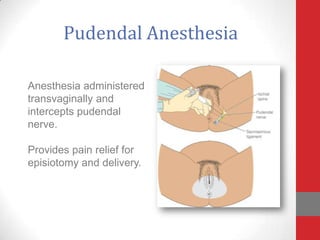
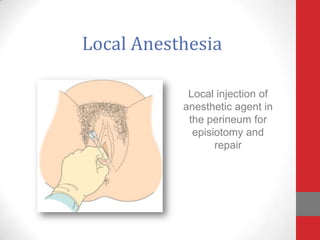
This document discusses pain management during labor and childbirth. It explains that labor pain is unique compared to other types of pain. Sources of labor pain include cervical dilation, uterine contractions, and fetal descent. Factors like preparation, culture, anxiety and fatigue can influence a woman's experience of pain. Non-pharmacological methods for managing pain include breathing, positioning, water therapy and relaxation techniques. Pharmacological options include opioids, epidural anesthesia and spinal anesthesia, each with advantages and disadvantages. Complications of regional anesthesia include hypotension and fetal distress. General anesthesia is riskier for mother and fetus due to issues like failed intubation or aspiration.