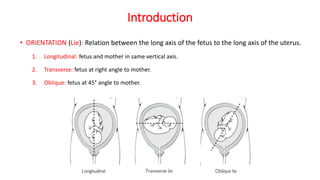
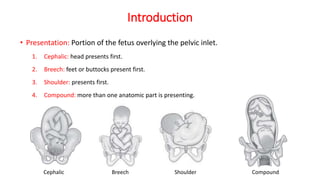
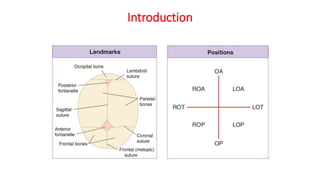
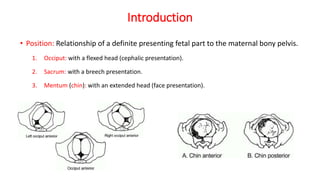
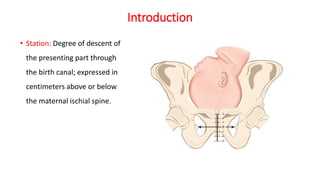
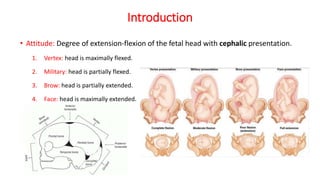
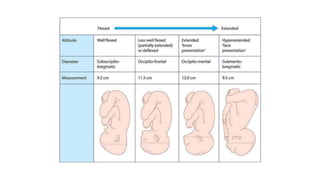
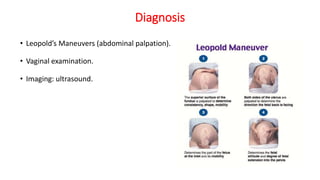
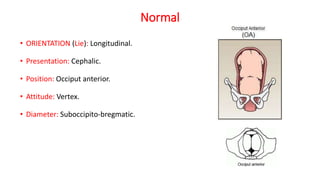
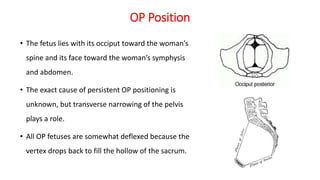
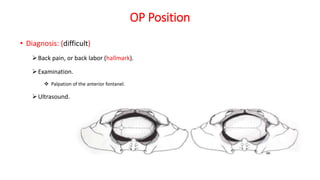
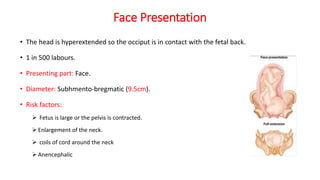
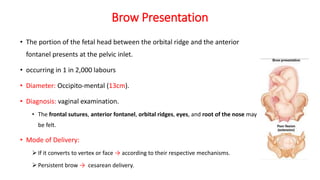
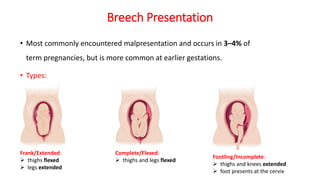
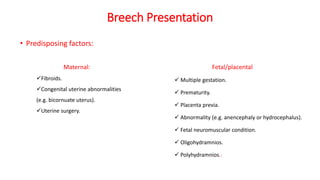
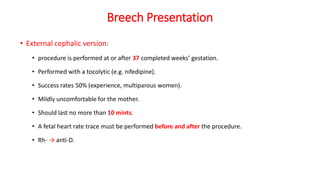
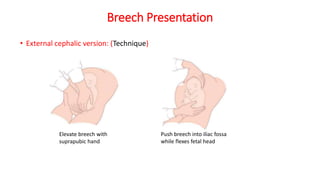
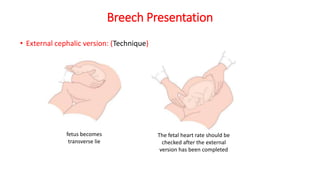
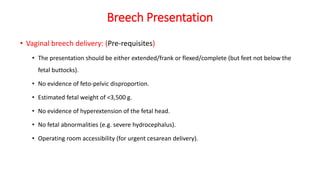
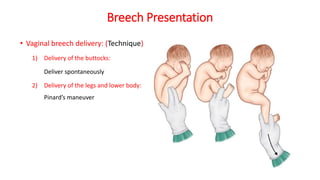
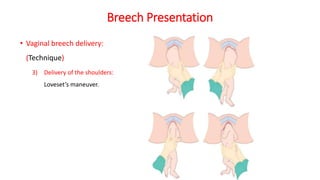
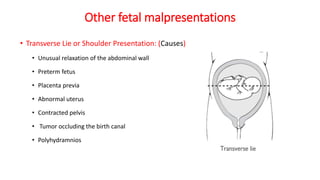
This document outlines various fetal malpresentations and malpositions that can occur during labor and delivery. It discusses normal presentation and position, as well as abnormal presentations including occiput posterior, face, brow, breech, transverse lie, shoulder, and compound. For each presentation, the document describes causes, diagnosis techniques including Leopold's maneuvers and ultrasound, and approaches to delivery management. Breech presentation is discussed in particularly depth, outlining types of breech, risk factors, techniques for external cephalic version and vaginal breech delivery.