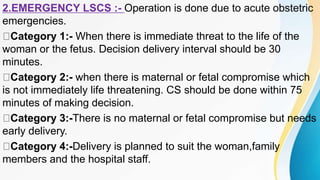
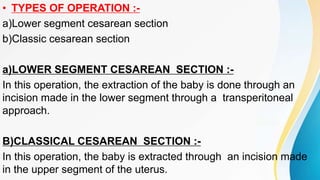
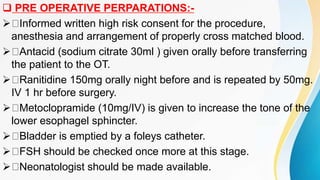
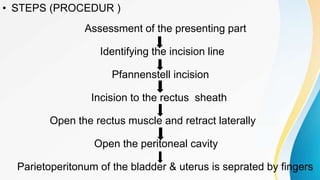
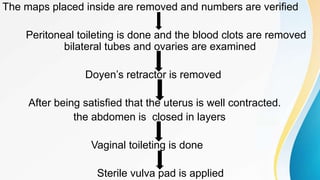
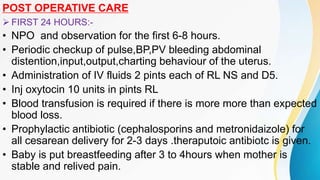
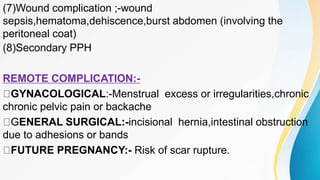
This document provides information about lower segment cesarean section (LSCS). It begins with an introduction defining LSCS as a surgical procedure to deliver a fetus after 28 weeks through an incision in the abdominal and uterine walls. It then discusses the rising incidence of LSCS, common indications including previous c-section and fetal distress, and the preoperative preparations and steps of the procedure. Complications are outlined as well, including potential issues for both the mother such as hemorrhage, and fetus like prematurity. Postoperative care including monitoring, antibiotics, feeding, and expected recovery timeline are also reviewed.