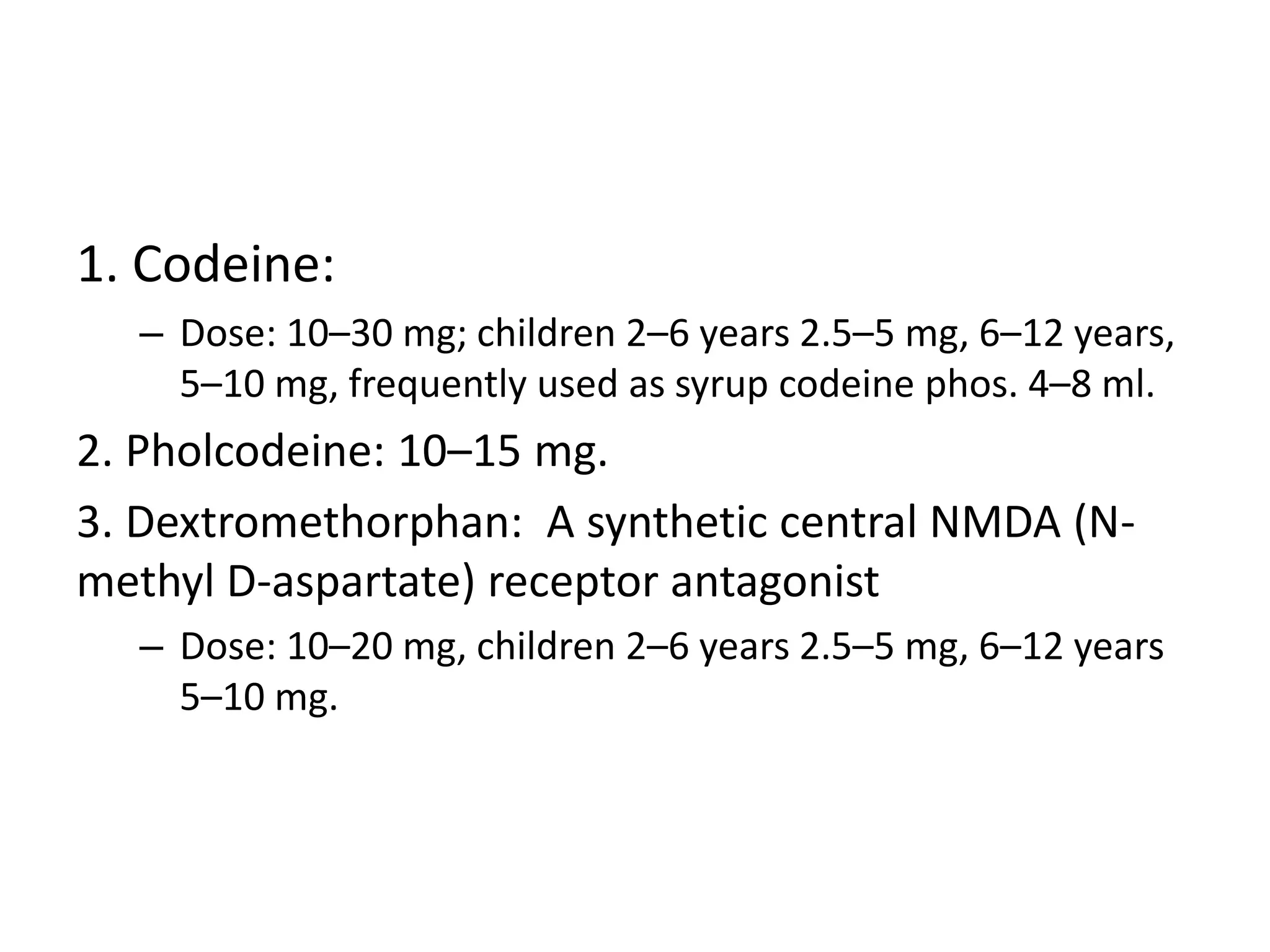
1. The document discusses various treatments for cough, asthma, and status asthmaticus. It outlines medications commonly used for their mucolytic, antitussive, bronchodilating, and anti-inflammatory effects such as bromhexine, carbocisteine, codeine, salbutamol, ipratropium bromide, and corticosteroids.
2. Asthma types and triggers are defined. Diagnosis involves pulmonary function tests and management involves both pharmacological and non-pharmacological approaches. Treatment selection is based on asthma severity and control.
3. Status asthmaticus is described as a life-threatening condition requiring immediate treatment including oxygen, nebulized bronch