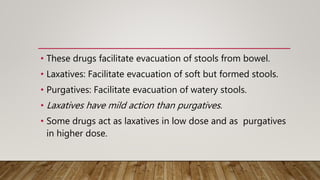
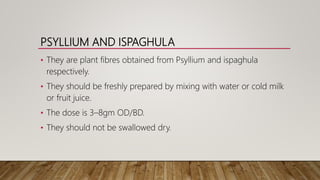
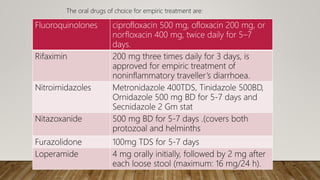
This document discusses various laxatives and purgatives used to treat constipation. It classifies them based on their mechanism of action into bulk forming agents, stool softeners, stimulant purgatives, and osmotic purgatives. It provides examples of commonly used drugs from each class and describes their doses, mechanisms of action, and side effects. The document also discusses antidiarrheal drugs and classifications of diarrhea. It outlines specific antimicrobial treatments for infectious causes of diarrhea and describes non-specific antidiarrheal drugs that decrease intestinal secretion and motility.















































































![Rotavirus Vaccines
RotaTeq Rotarix
Genetic framework Bovine Rotavirus – WC3 Human Rotavirus-89-12
Composition 5 Human, Bovine re-assortant Single Human rotavirus
Genotypes G1, 2, 3, 4 and [P8] G1 [P8]
Dosage Schedule 3 doses at 2, 4 and 6 months 2 doses at 2 and 4 months
Route oral oral
Presentation liquid Lysophilized-reconstituted
Efficacy against severe disease 85% 95%
Virus shedding Up to 13 % 17 % - 27%](https://image.slidesharecdn.com/drugsforconstipationandiarrhoeambbs-190704061210/85/Drugs-for-constipationa-n-diarrhoea-85-320.jpg)