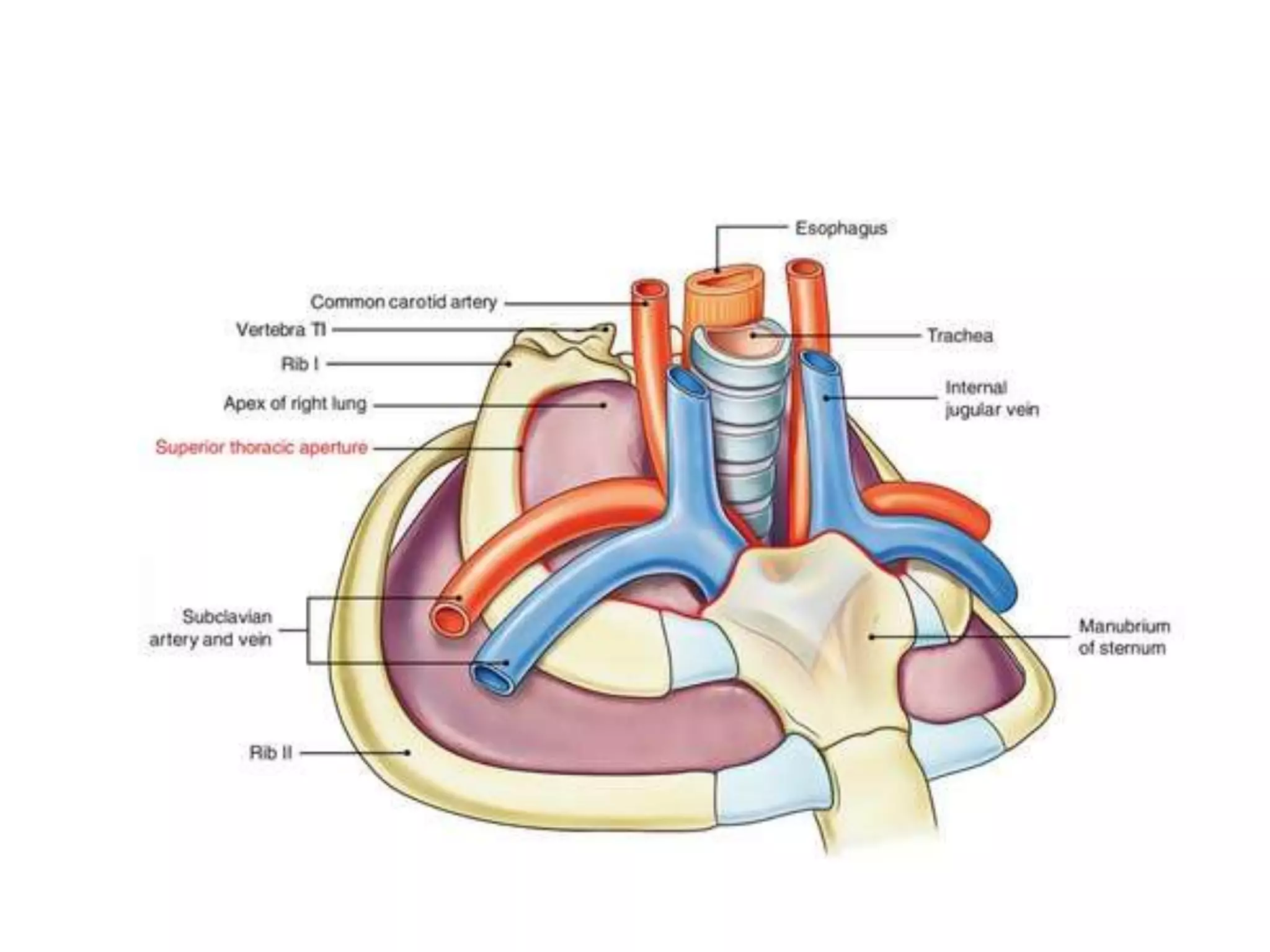
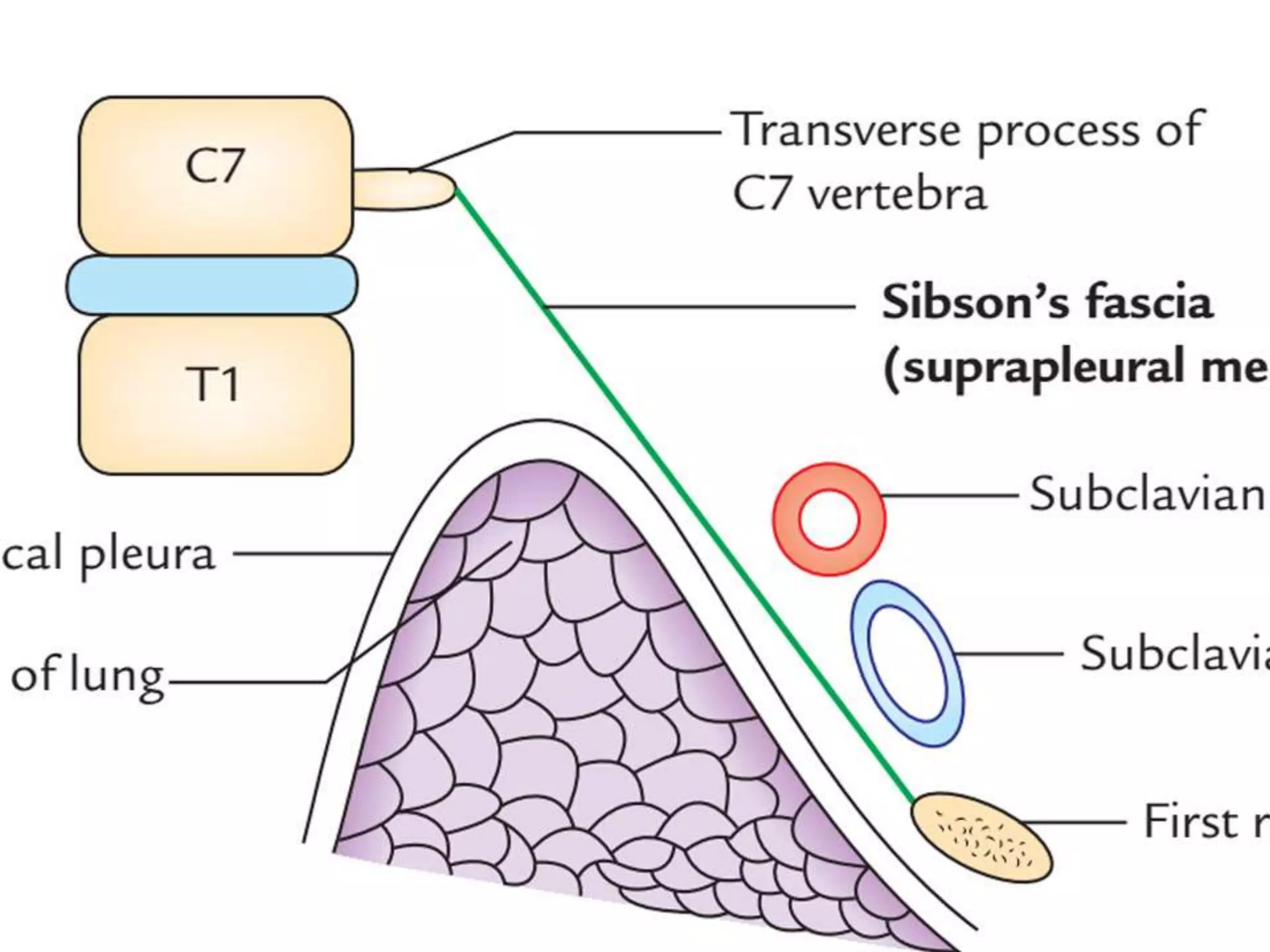
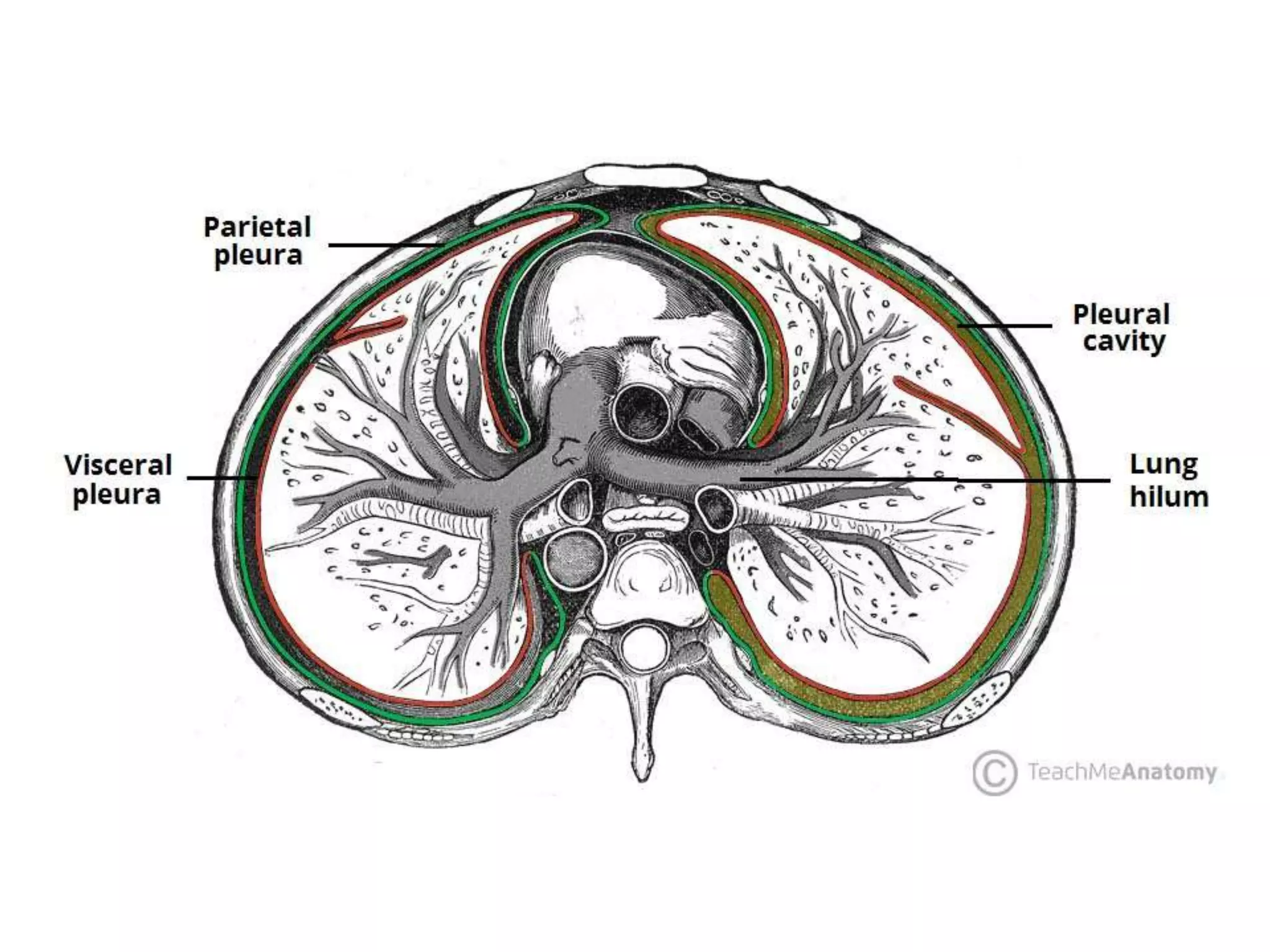
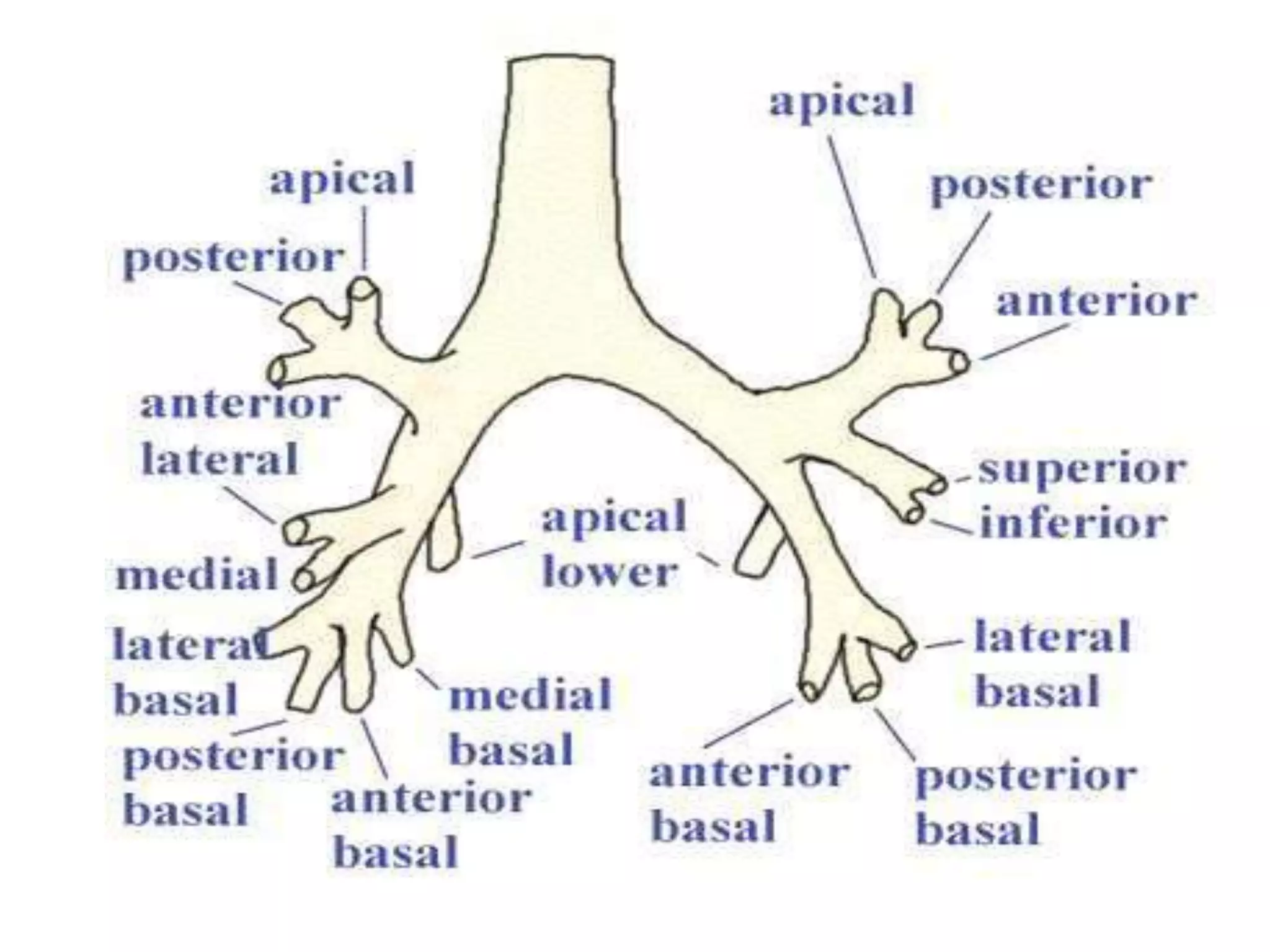
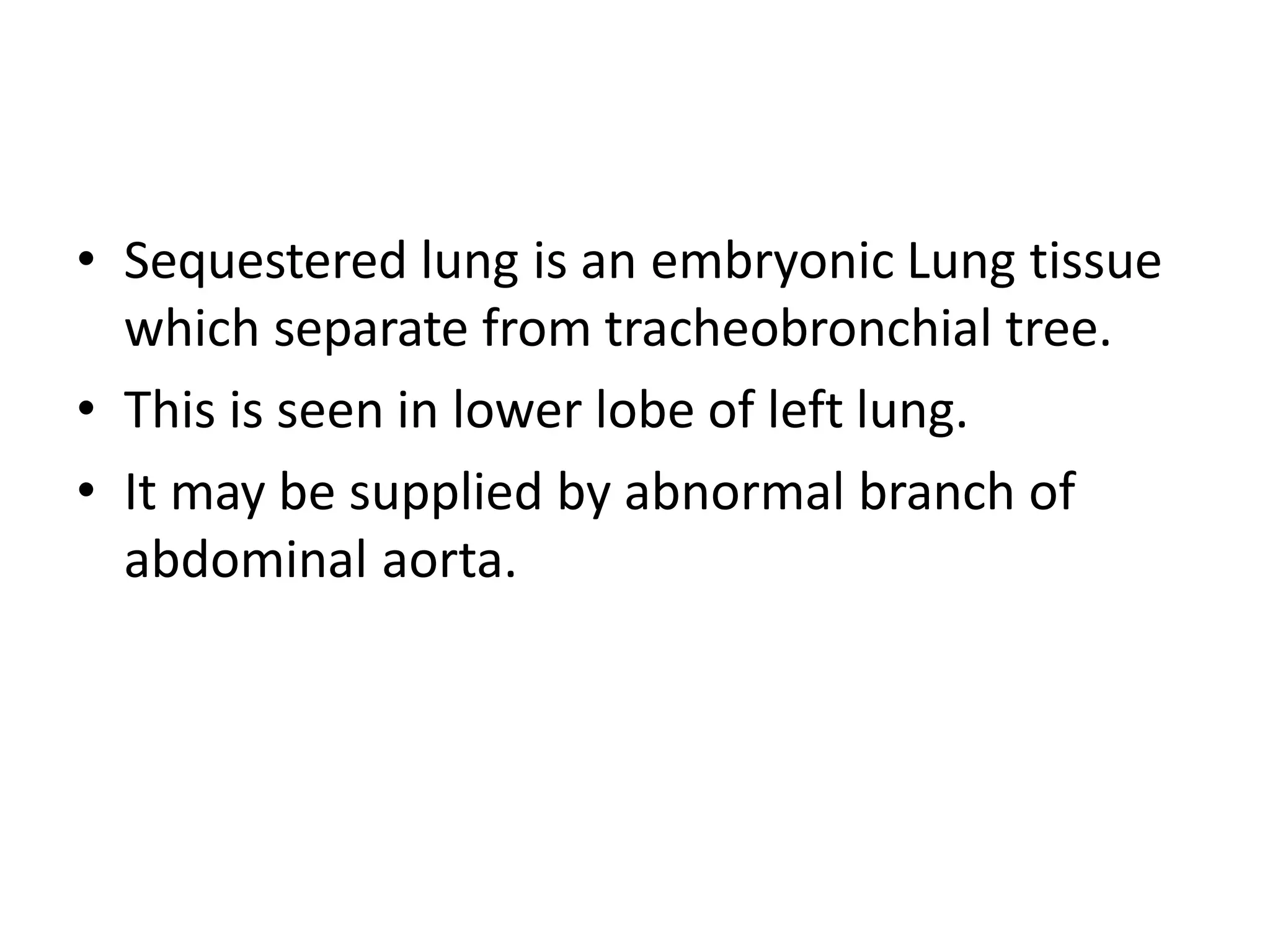
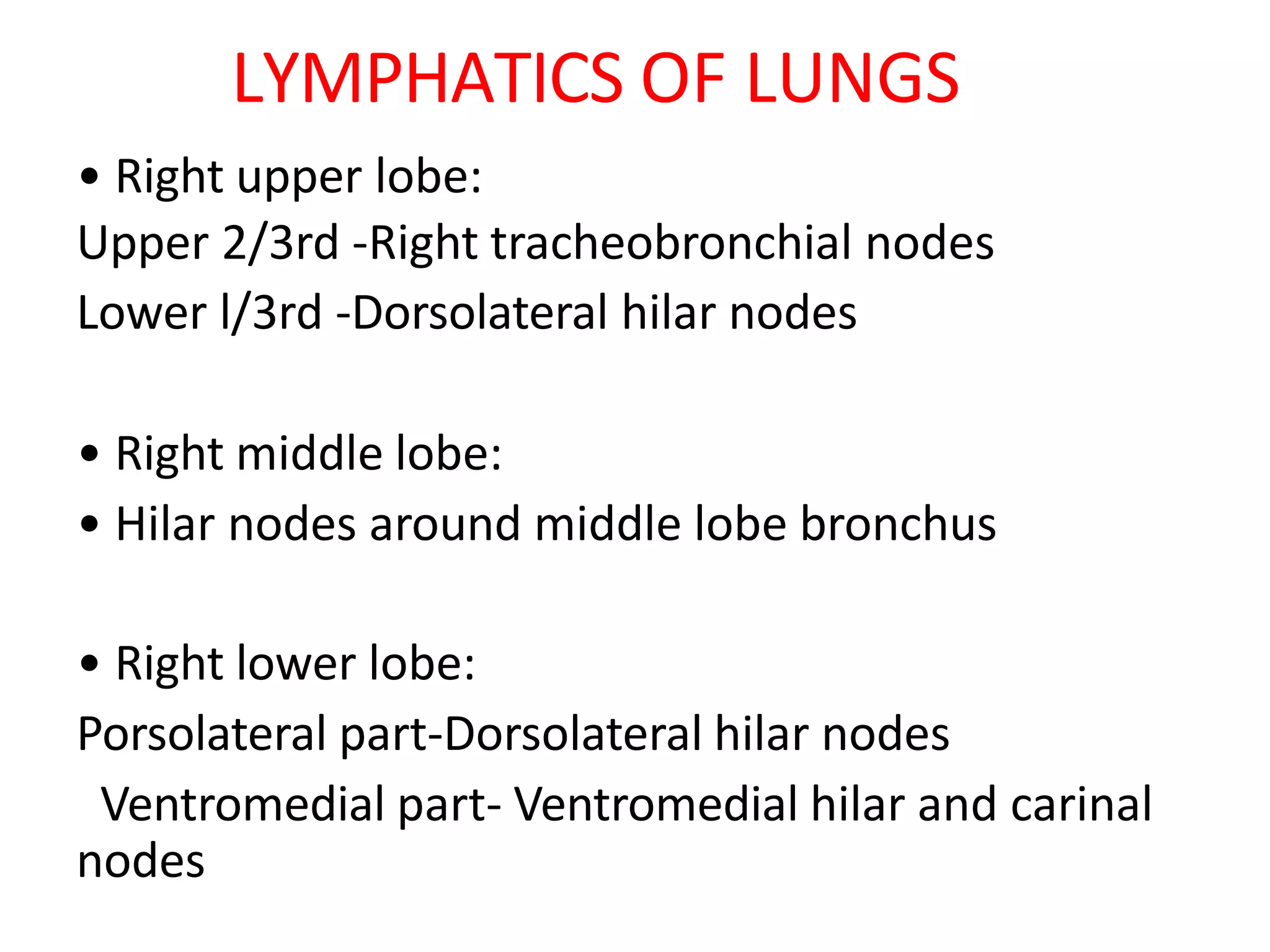
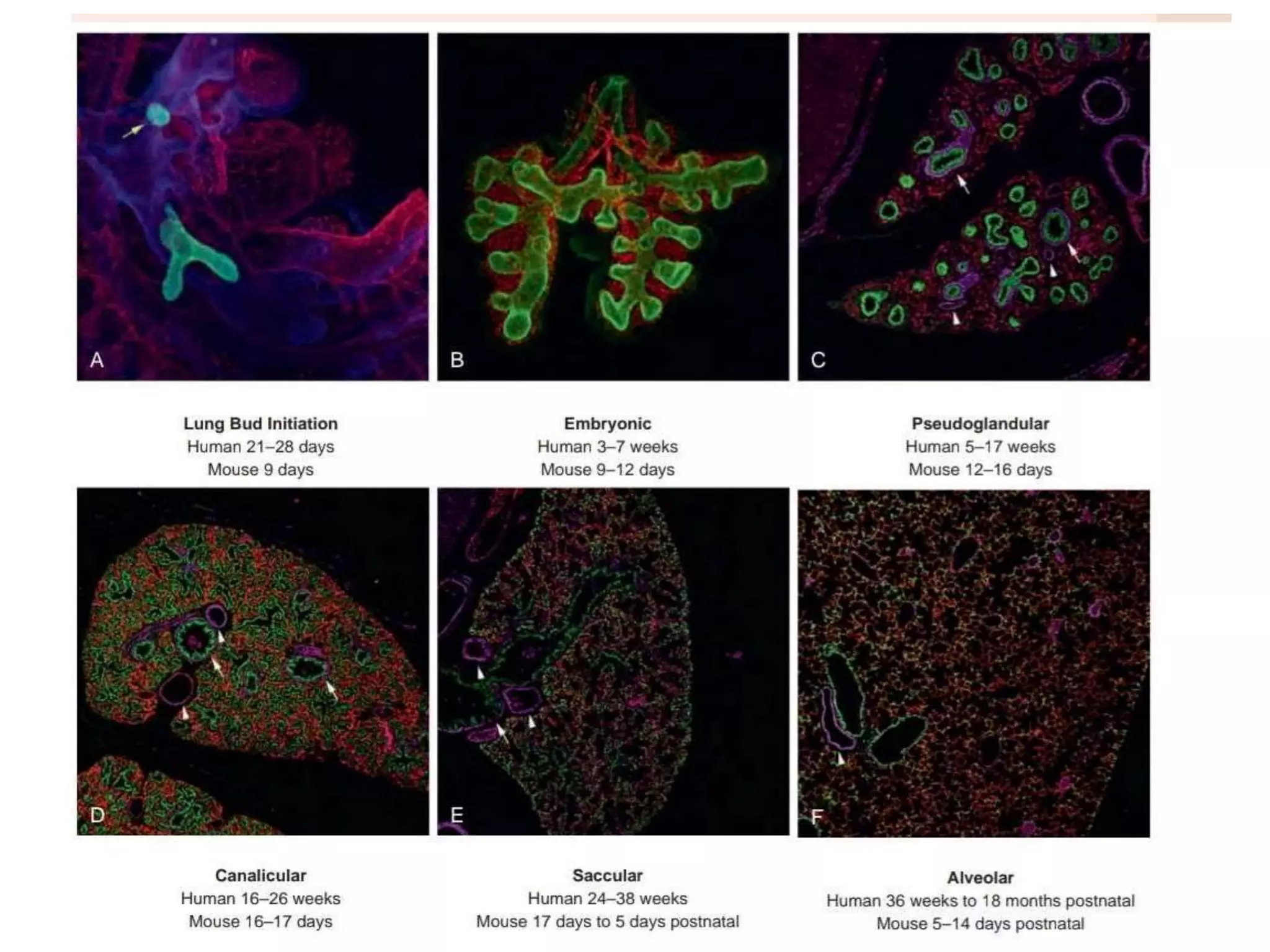
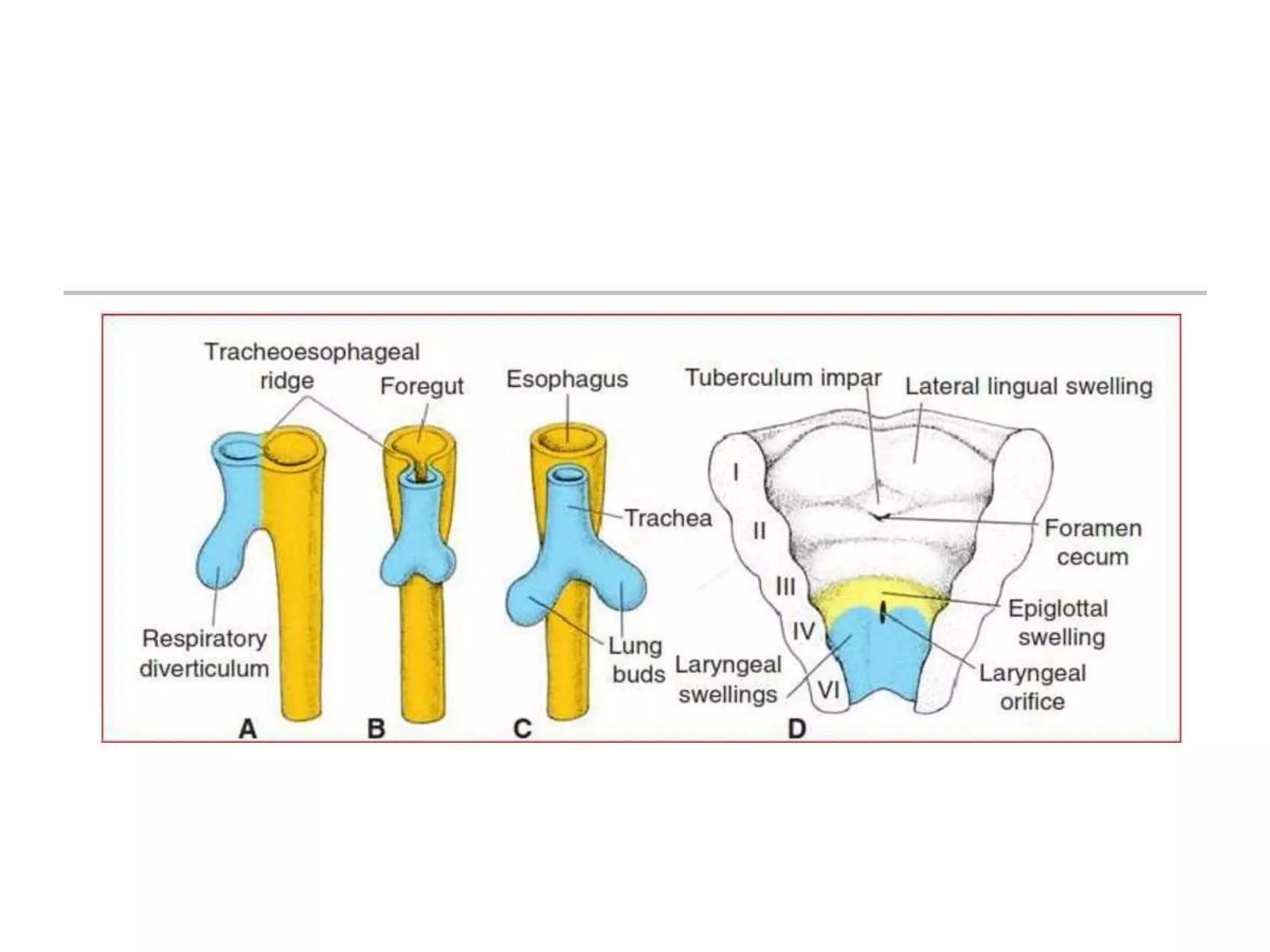
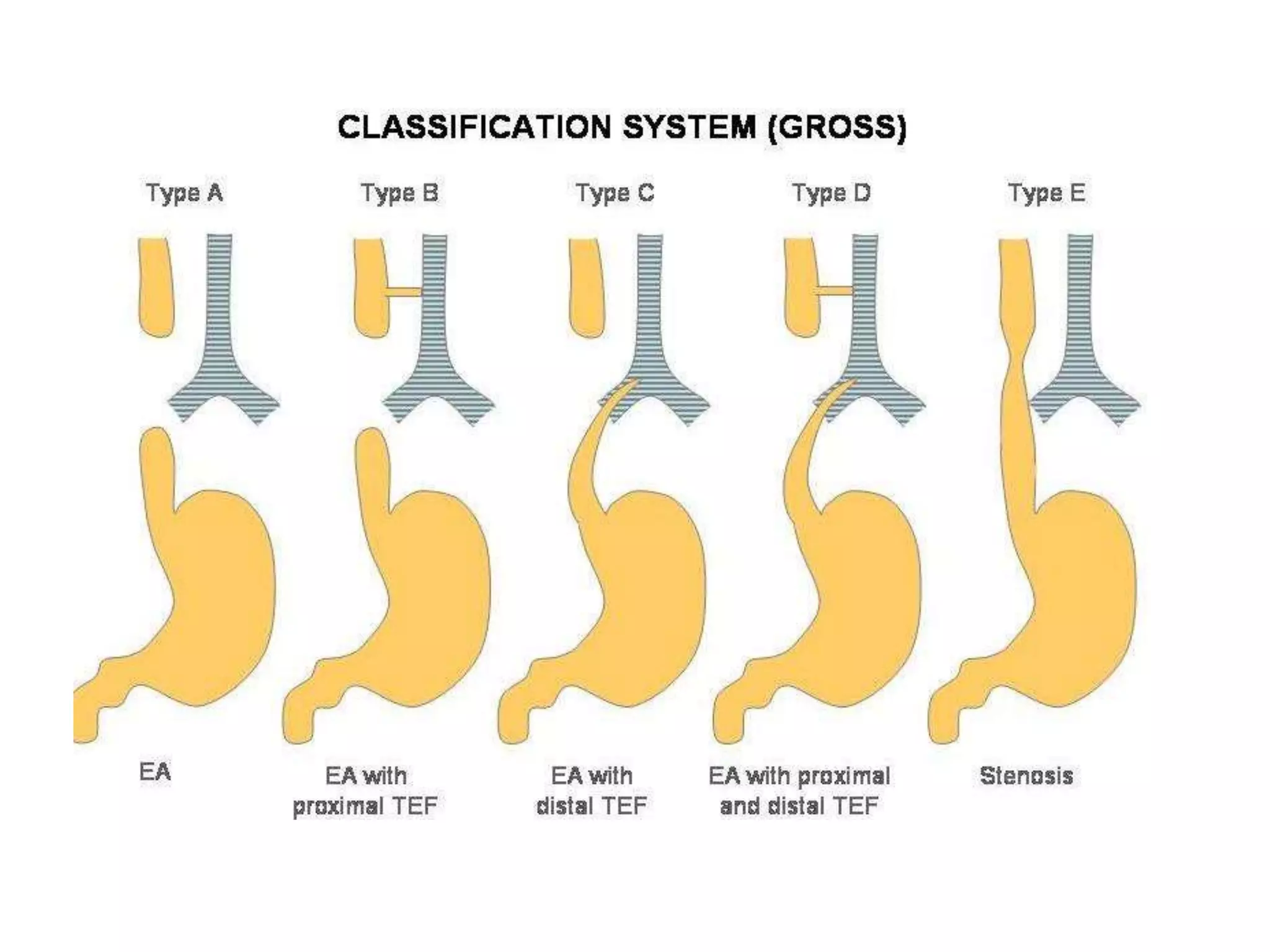
The document provides a detailed overview of the anatomy and development of the lungs, covering aspects such as their gross structure, surfaces, lobes, blood supply, nerve supply, lymphatics, and pleura. It also discusses the stages of lung development, from embryonic formation to postnatal changes, including the implications of conditions like tracheoesophageal fistula and respiratory distress syndrome. Additionally, it includes clinical significance and management approaches related to various lung pathologies.