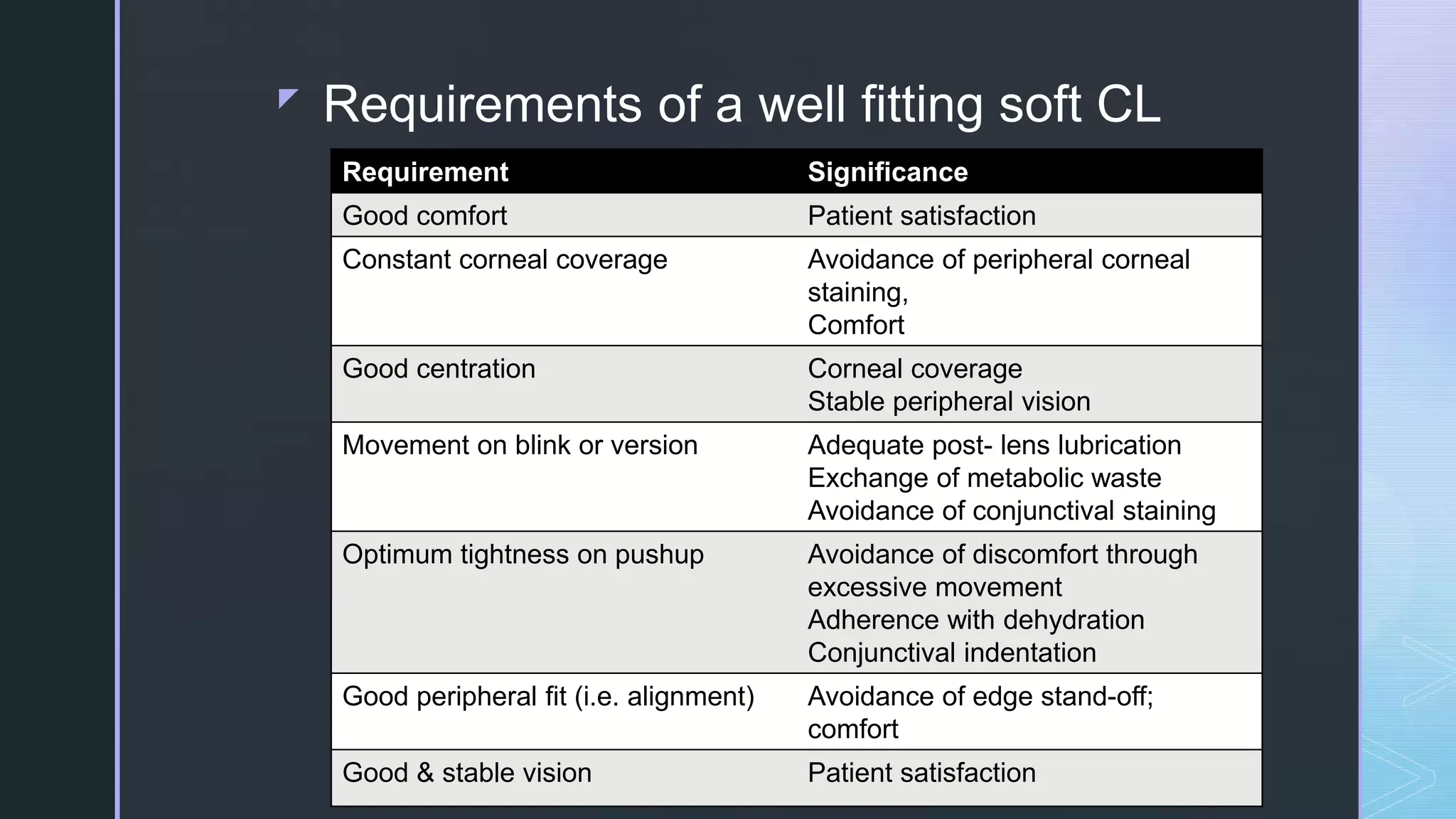
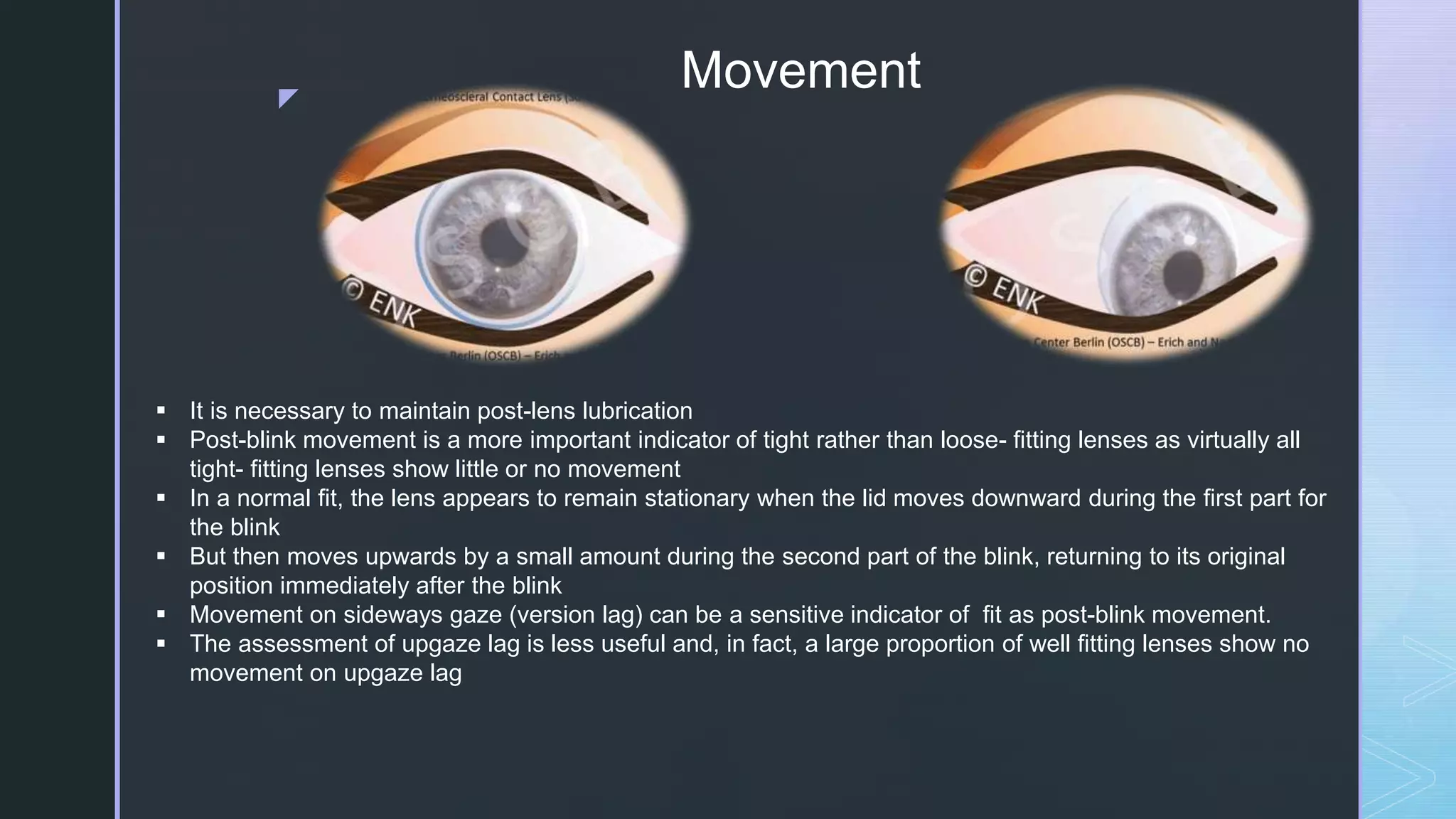
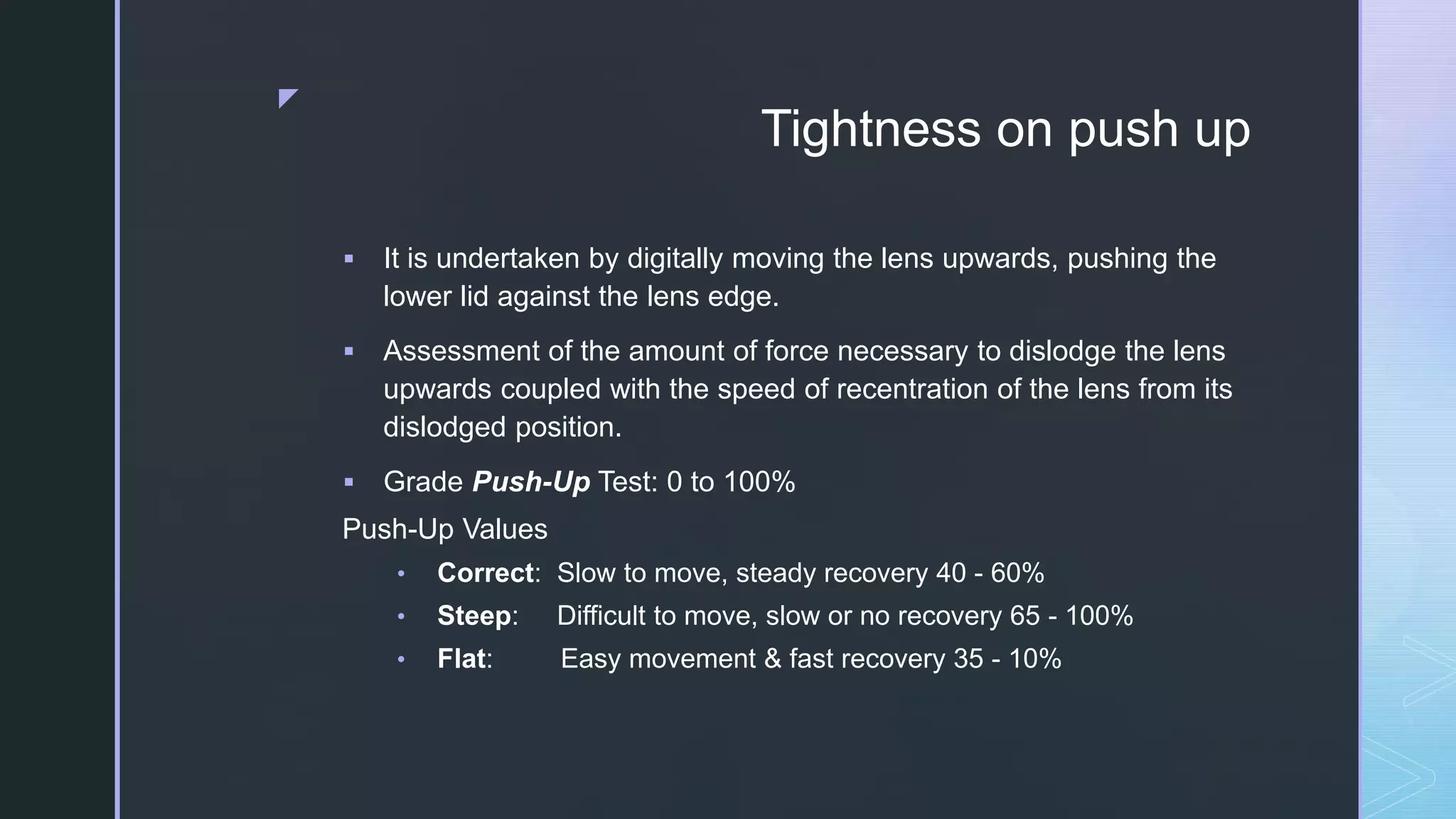
The document discusses the requirements and assessment of soft contact lens fitting. It outlines the characteristics of an optimum fit versus a tight or loose fit, including factors like comfort, centration, movement, tightness on push-up, and peripheral fit. The assessment of fit involves evaluating these factors through tests like observing movement, tightness on push-up, and assessing vision. Common fitting problems like discomfort, inappropriate diameter or fit tightness are also summarized.