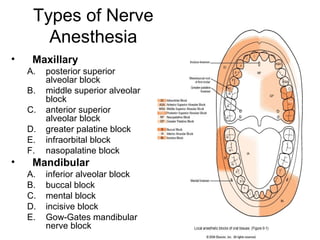
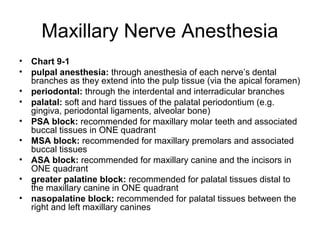
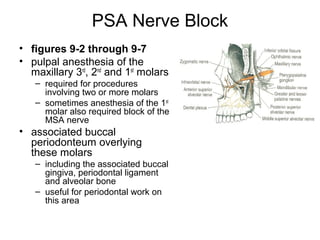
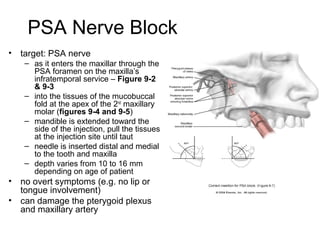
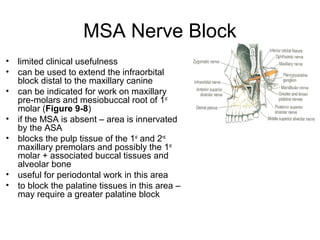
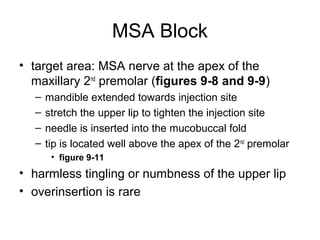
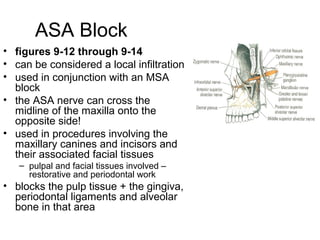
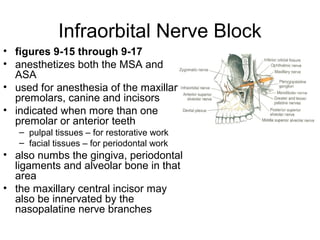
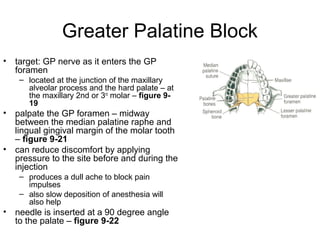
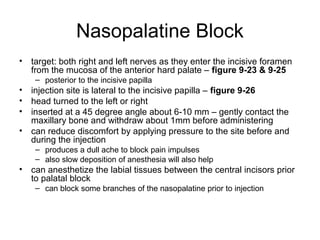
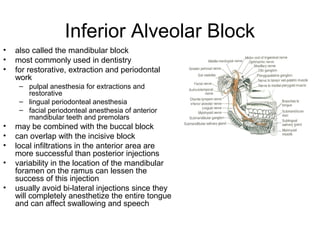
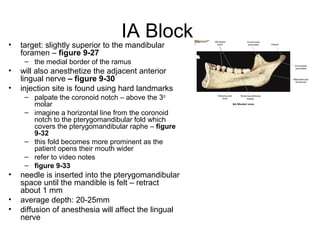
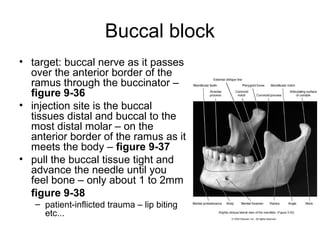
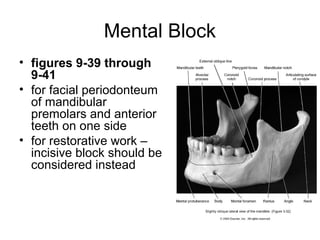
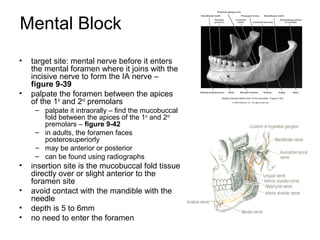
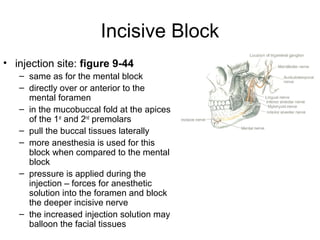
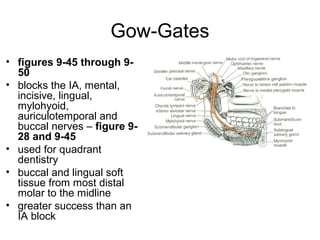
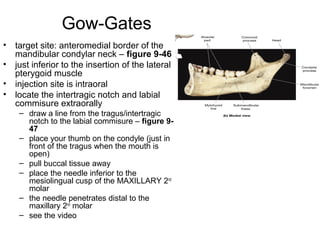
The document discusses different types of local anesthesia used in dentistry, including local infiltration which anesthetizes a small area and nerve blocks which anesthetize larger areas. It provides detailed descriptions and illustrations of various nerve blocks used for maxillary and mandibular anesthesia, including the posterior superior alveolar, infraorbital, greater palatine, and inferior alveolar nerve blocks. The inferior alveolar nerve block is the most commonly used technique in dentistry for restorative procedures, extractions, and periodontal work on mandibular teeth.