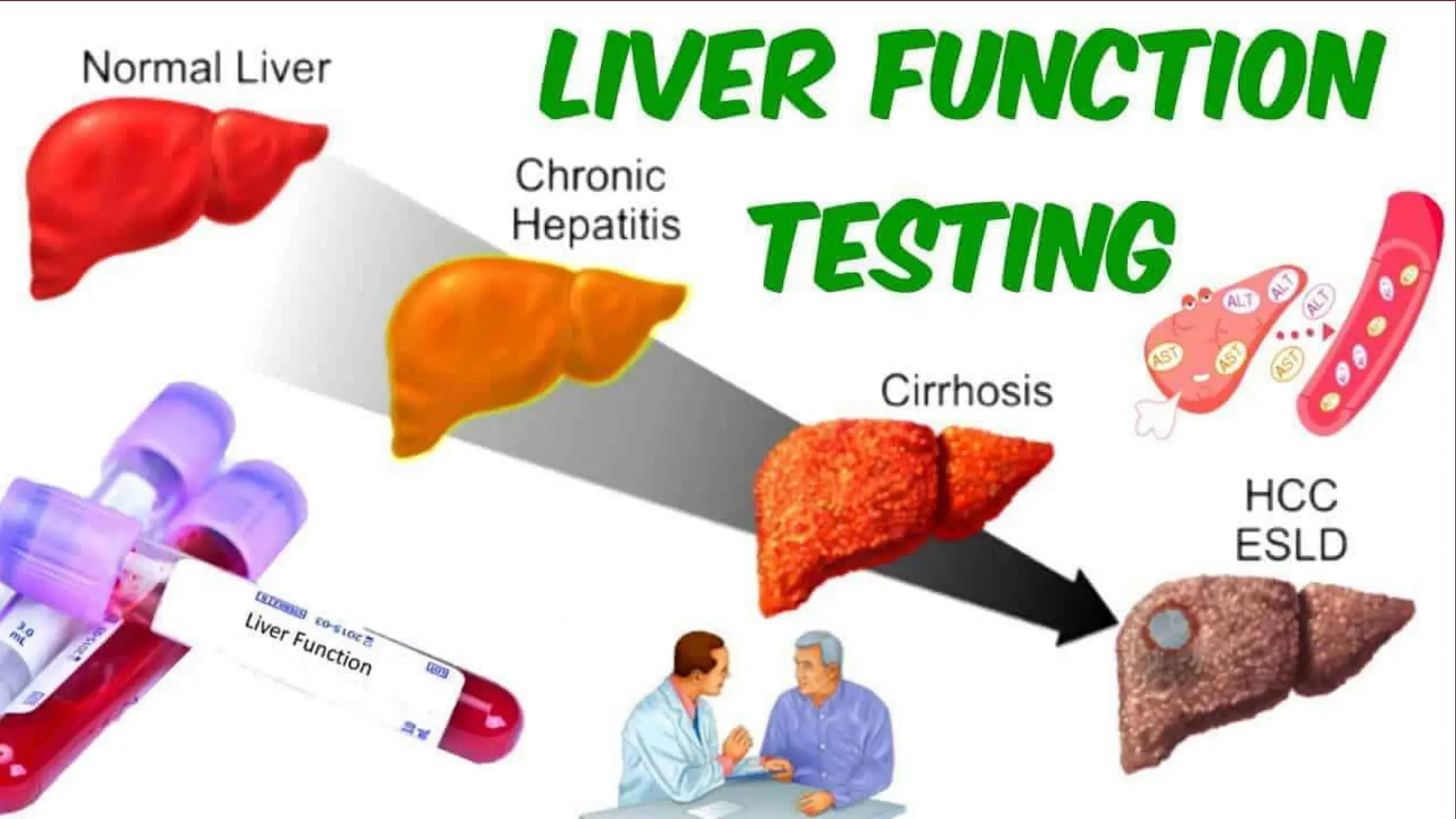
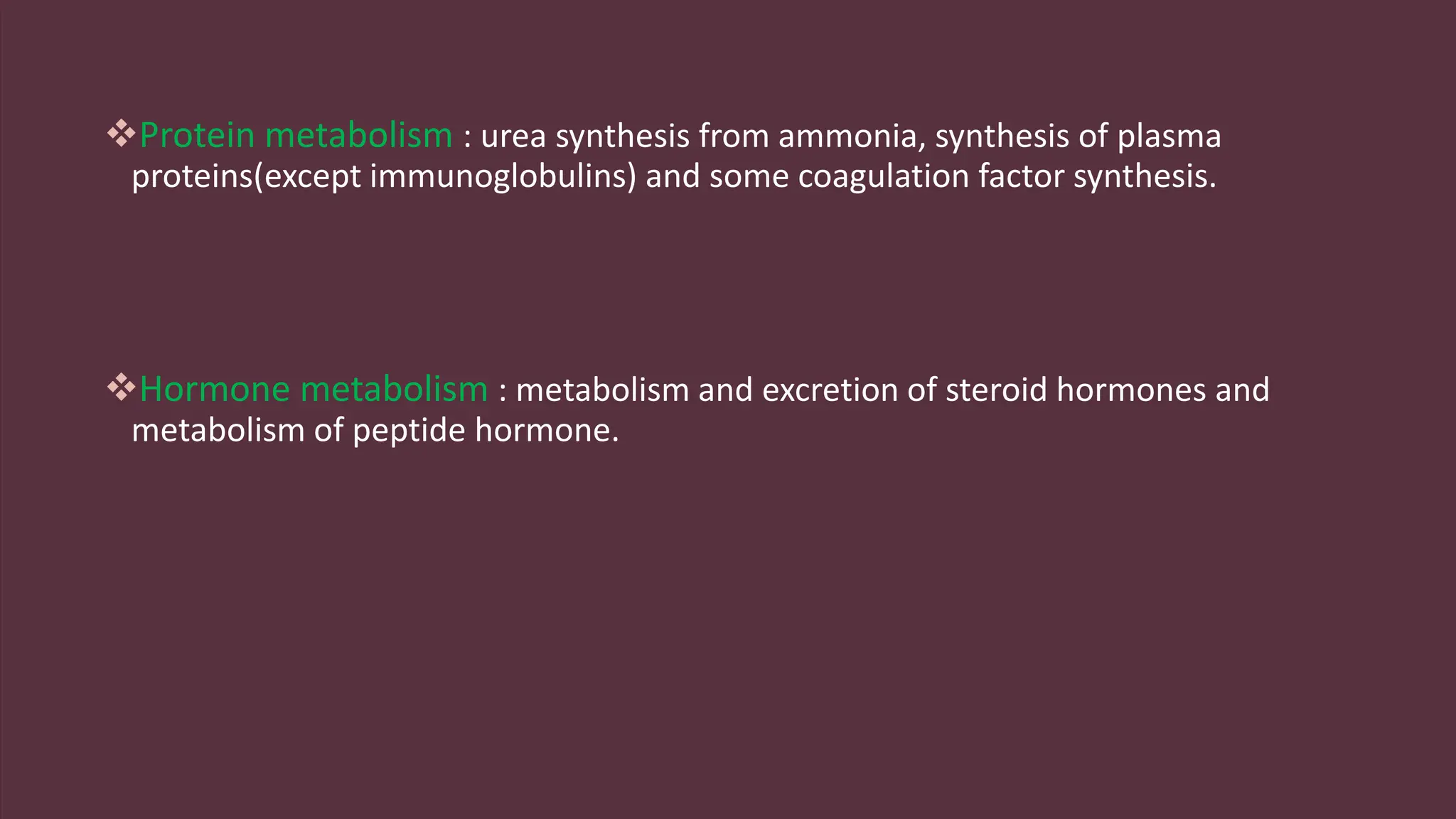
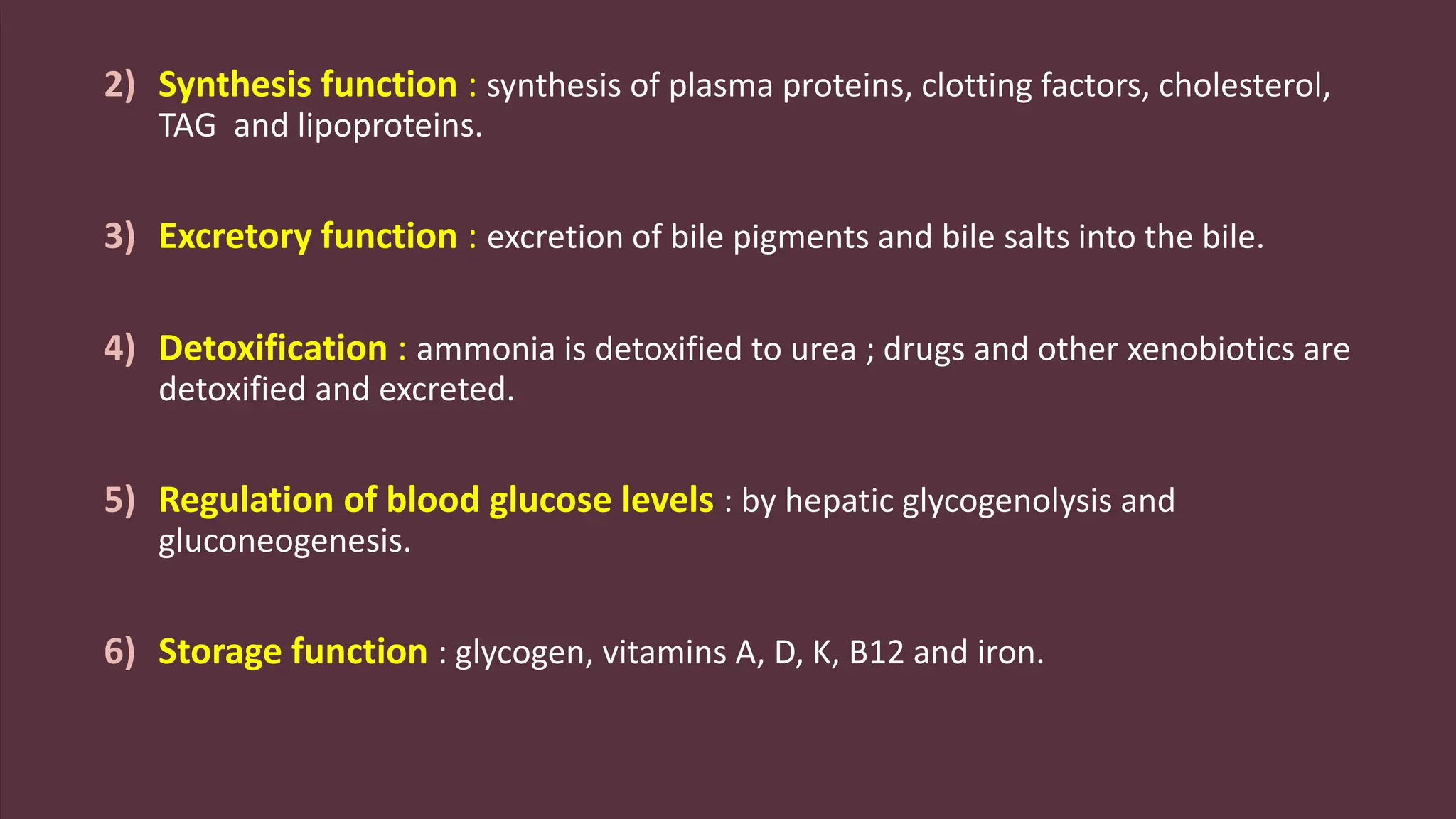
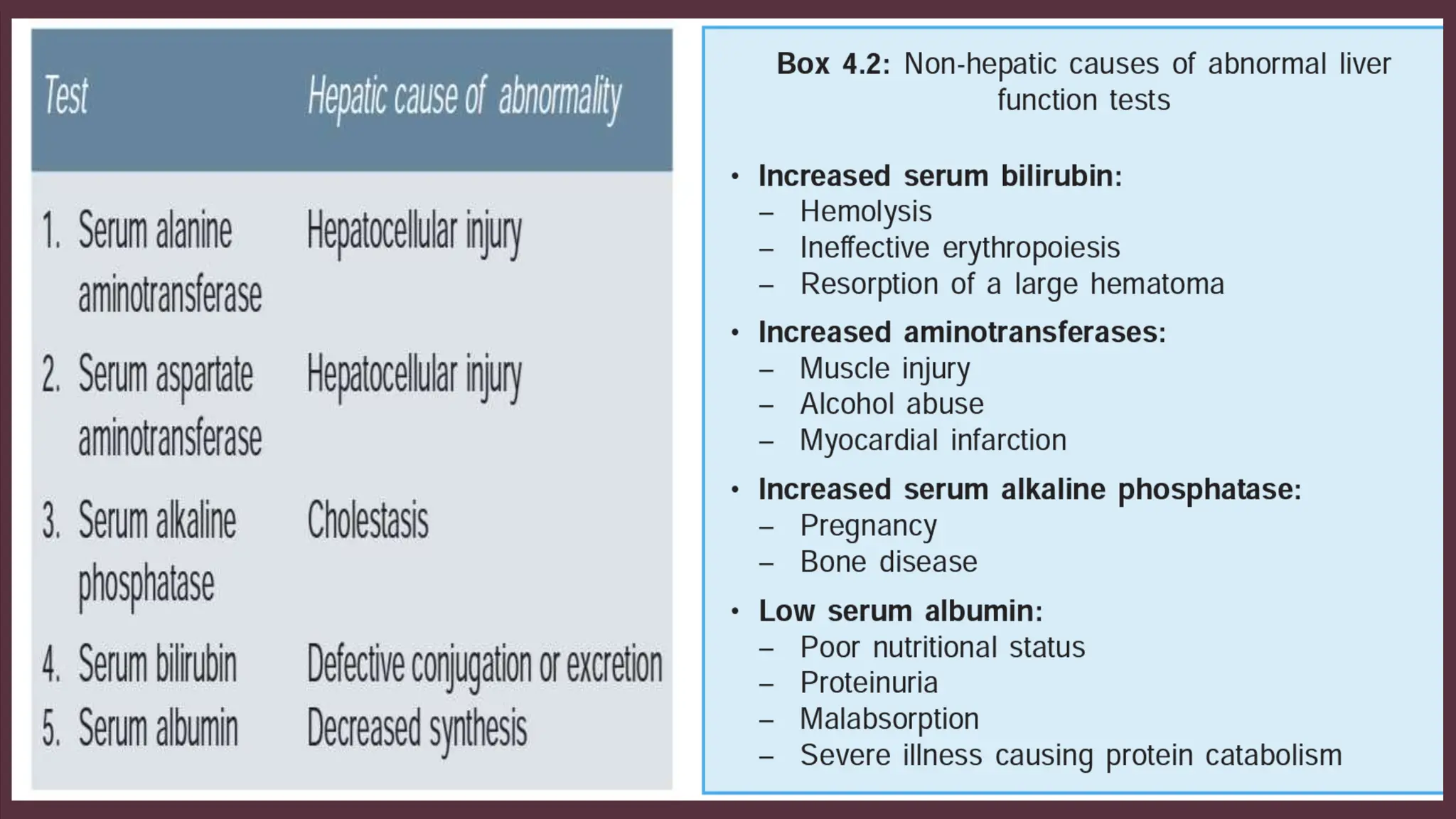
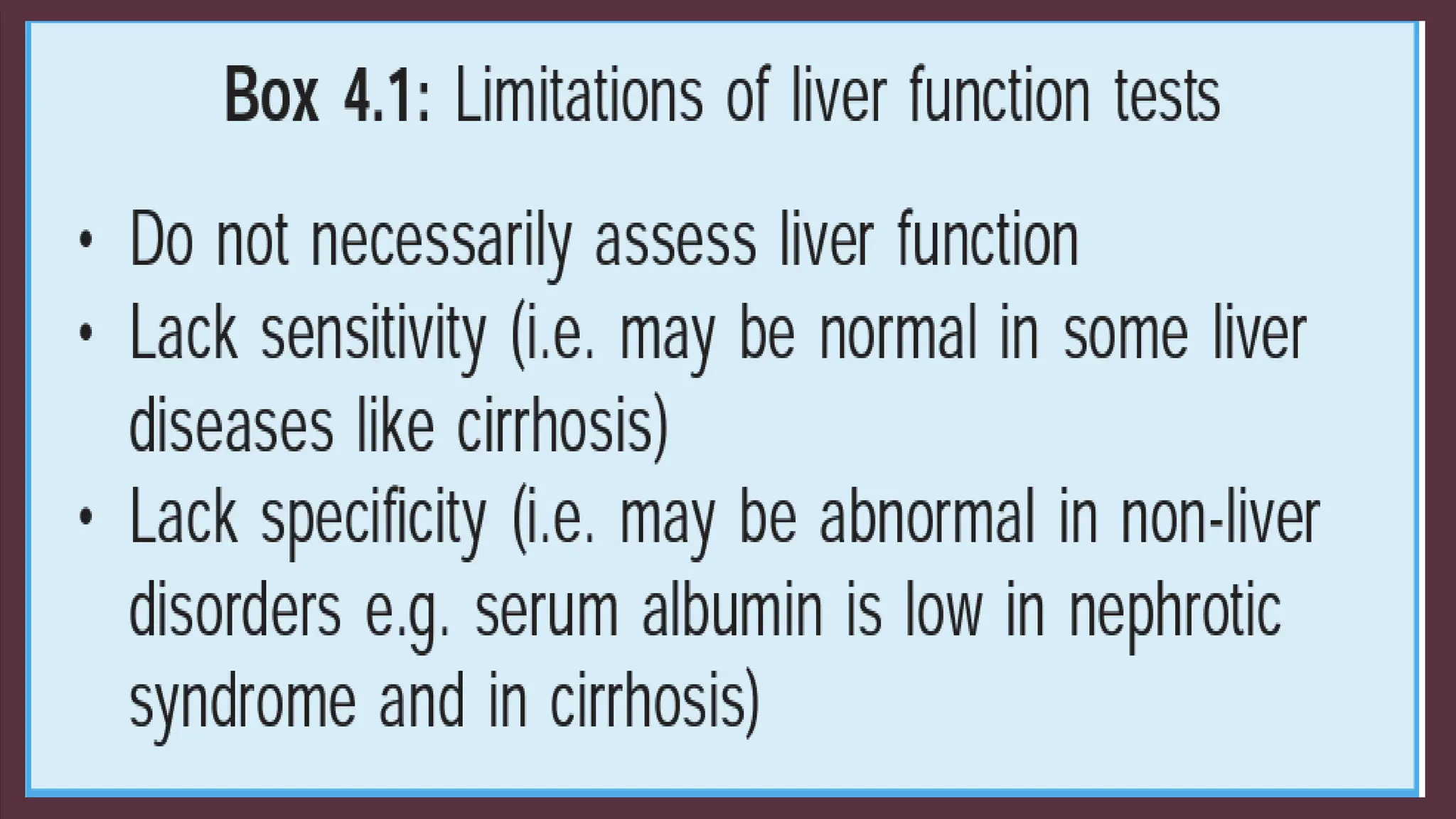
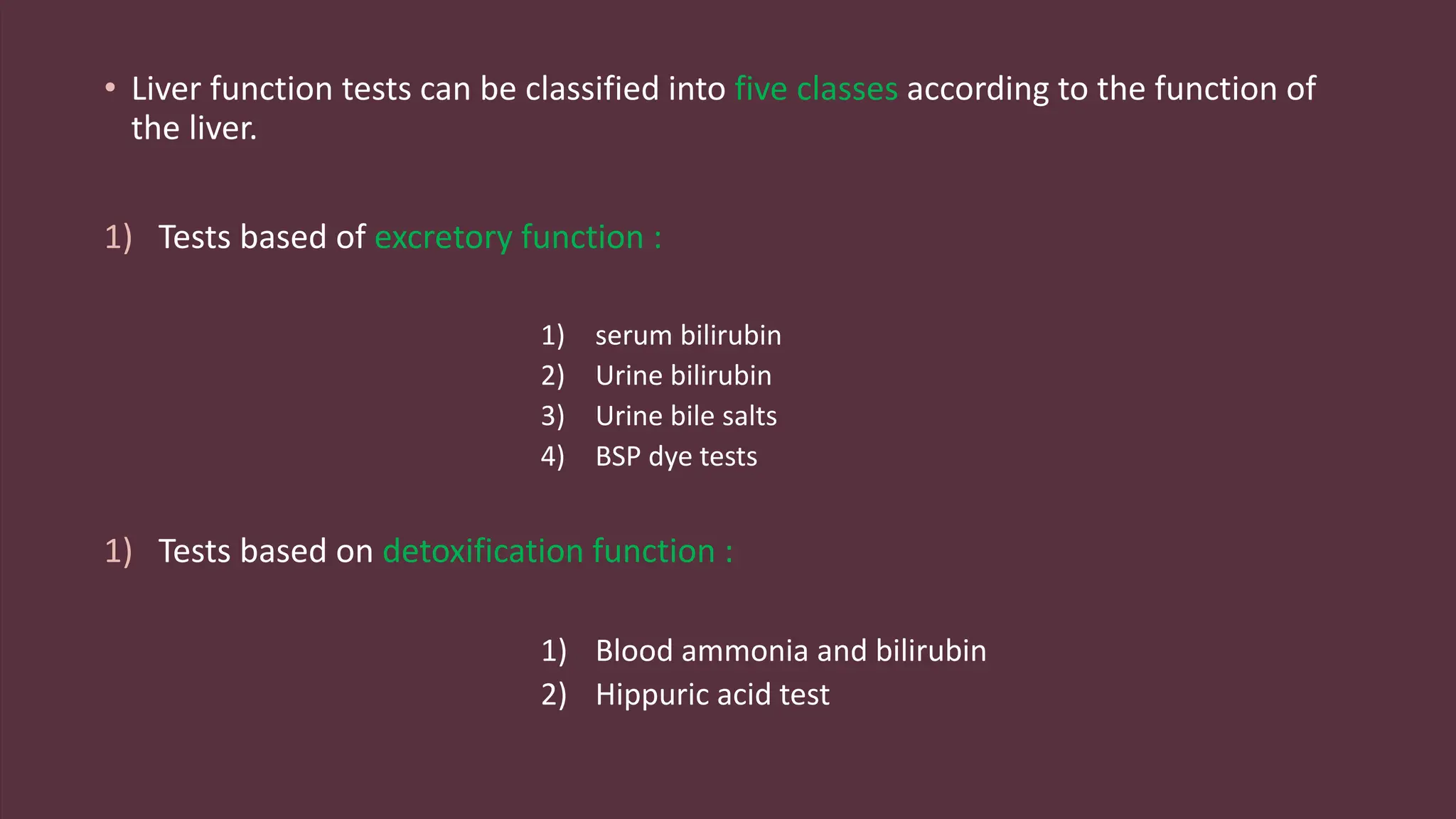
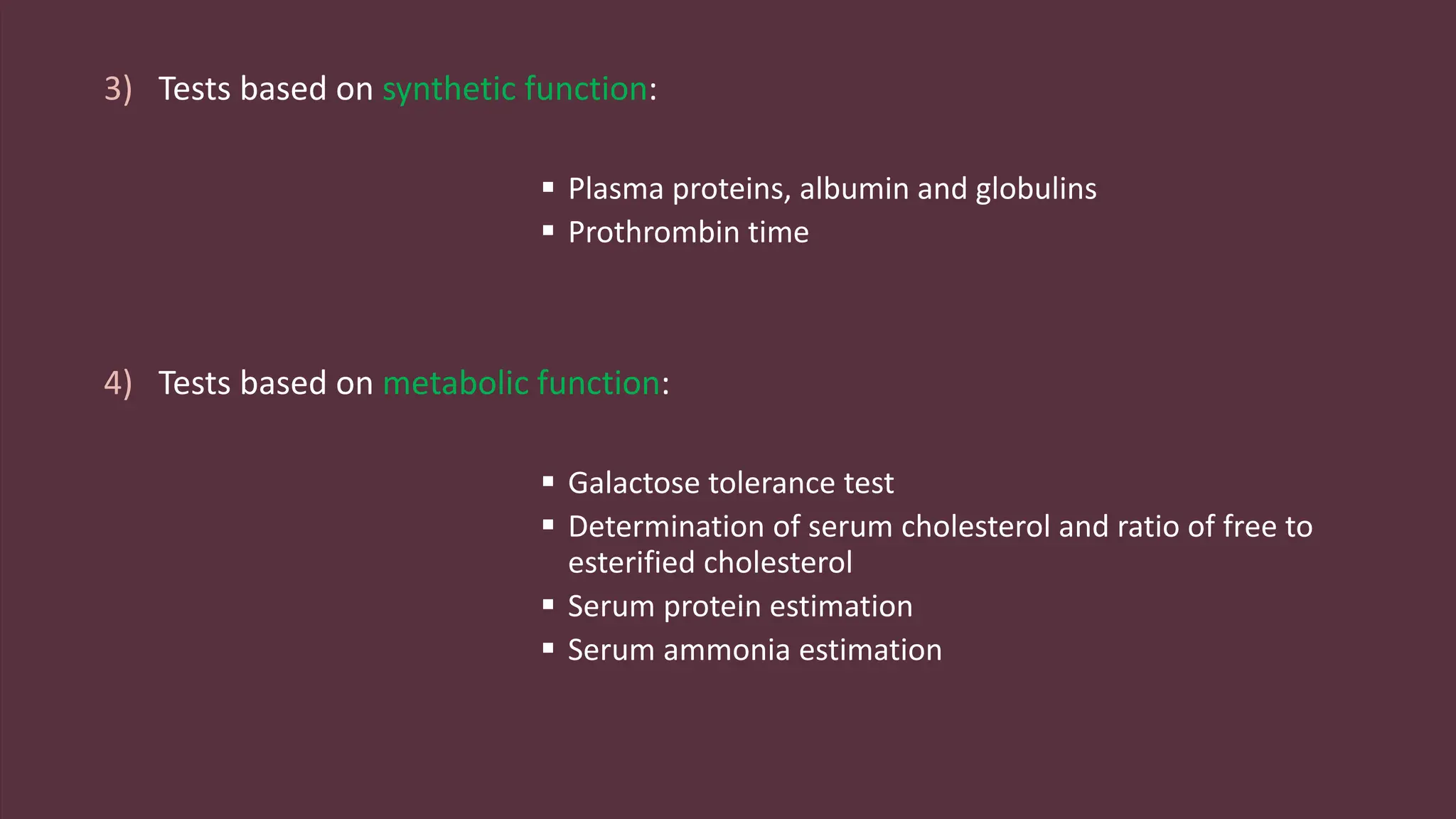
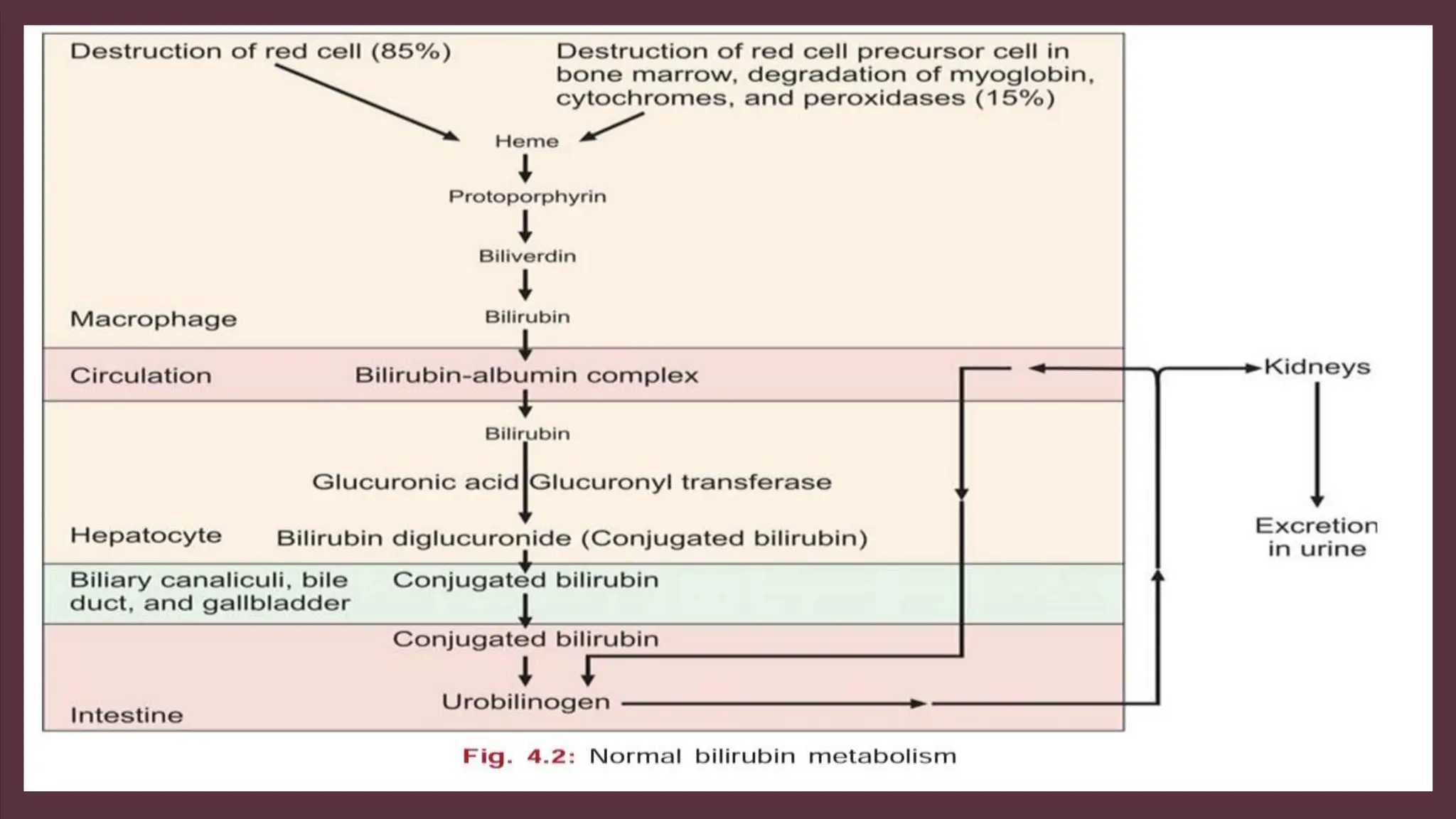
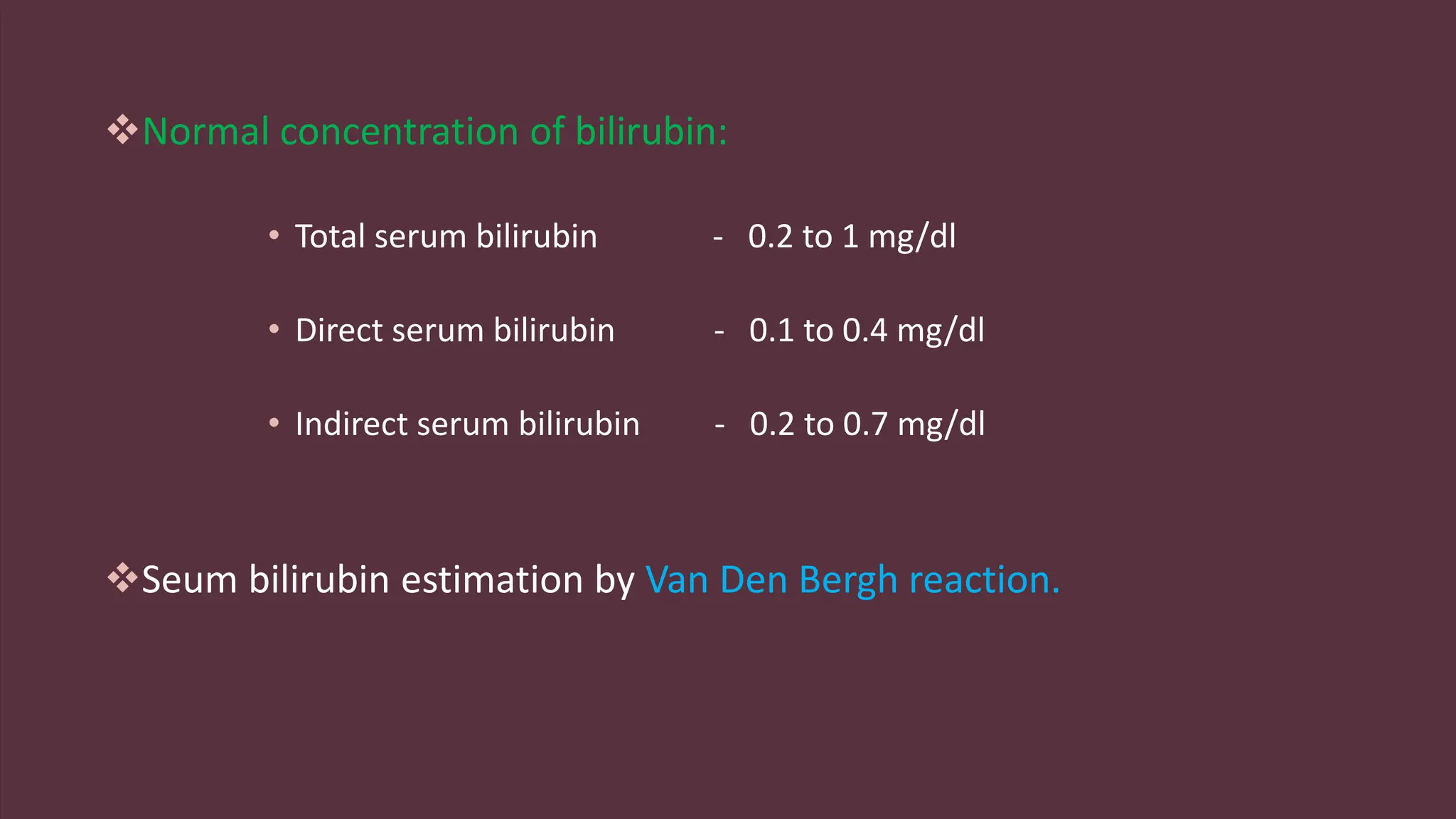
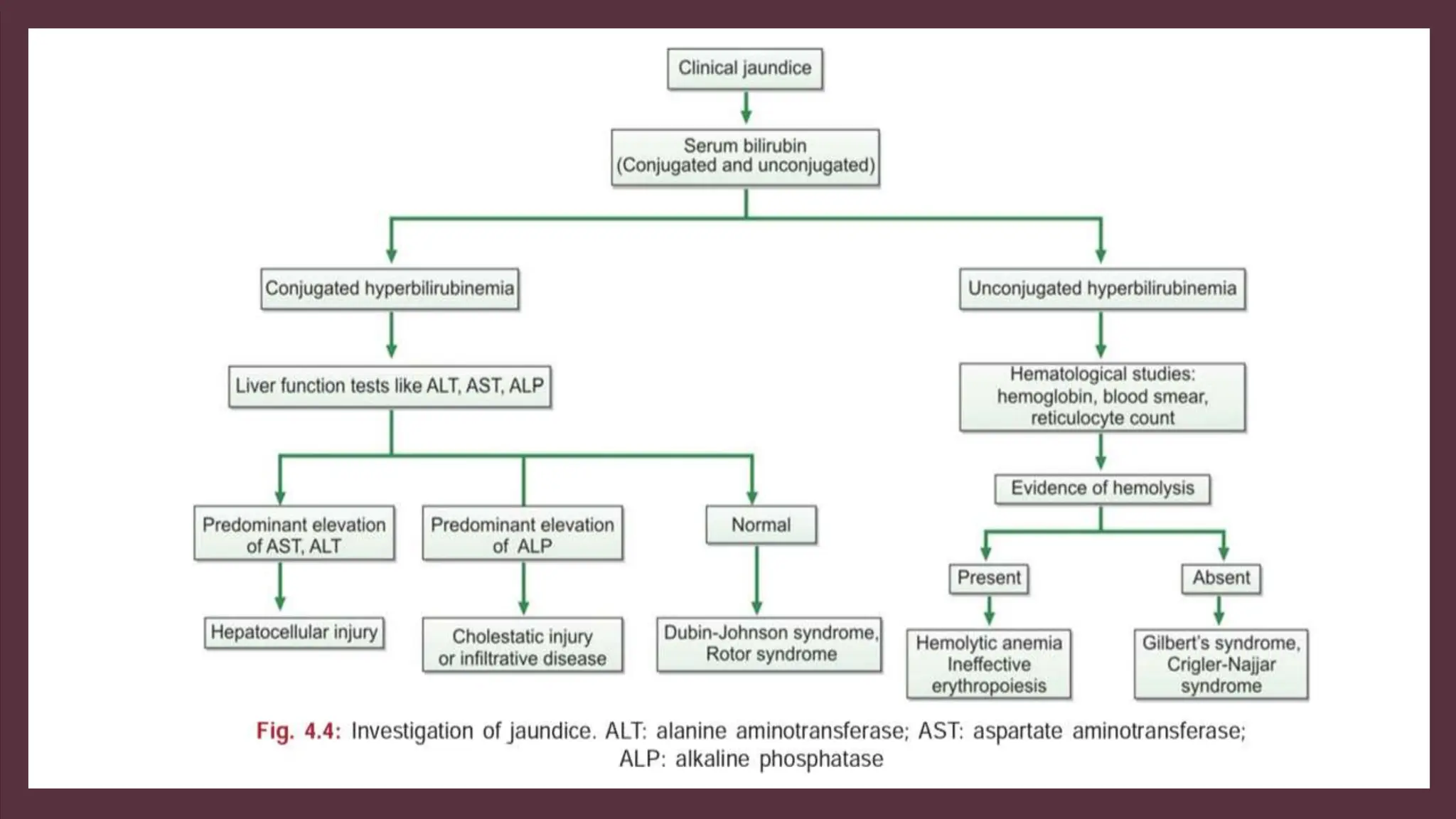
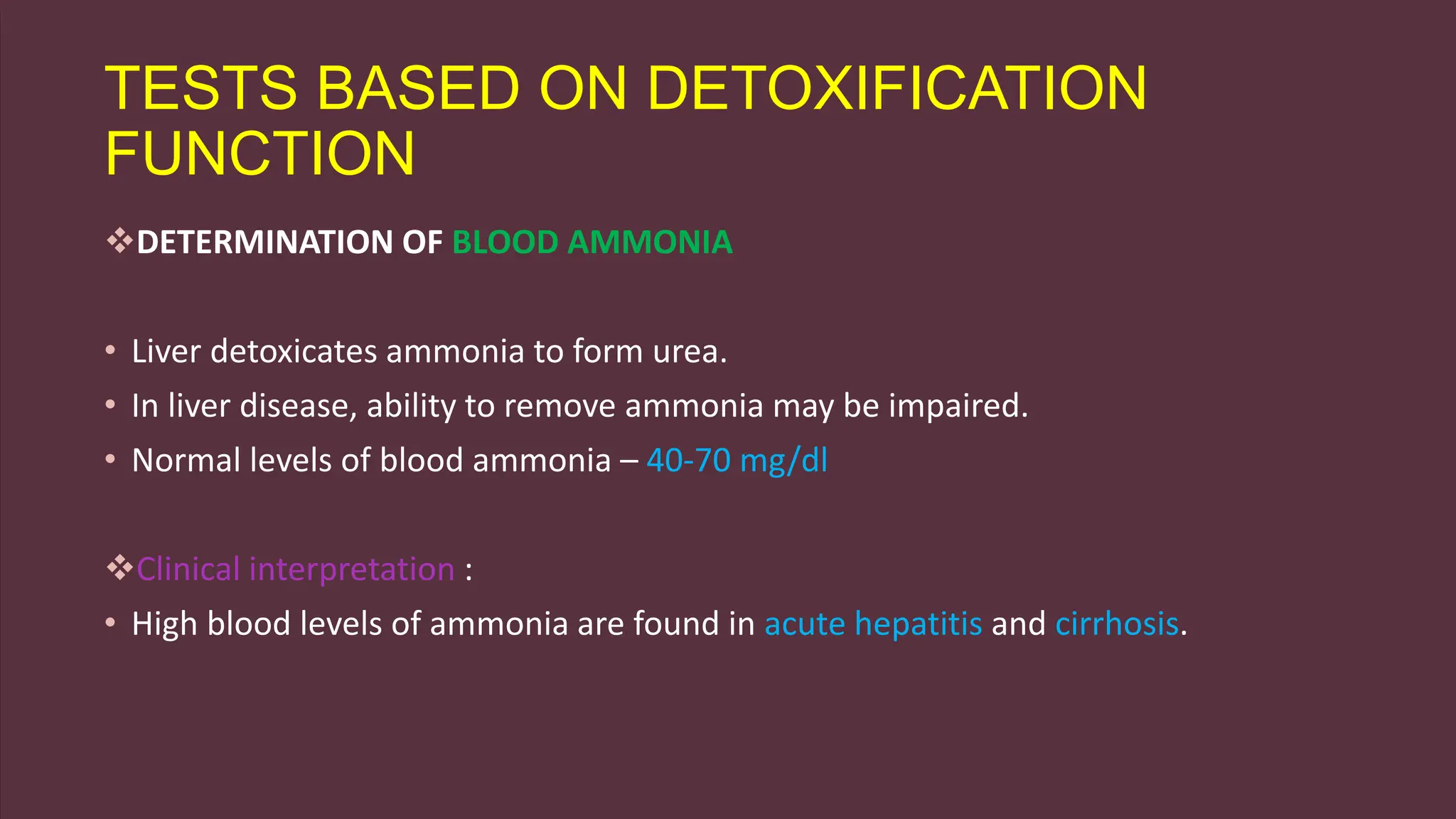
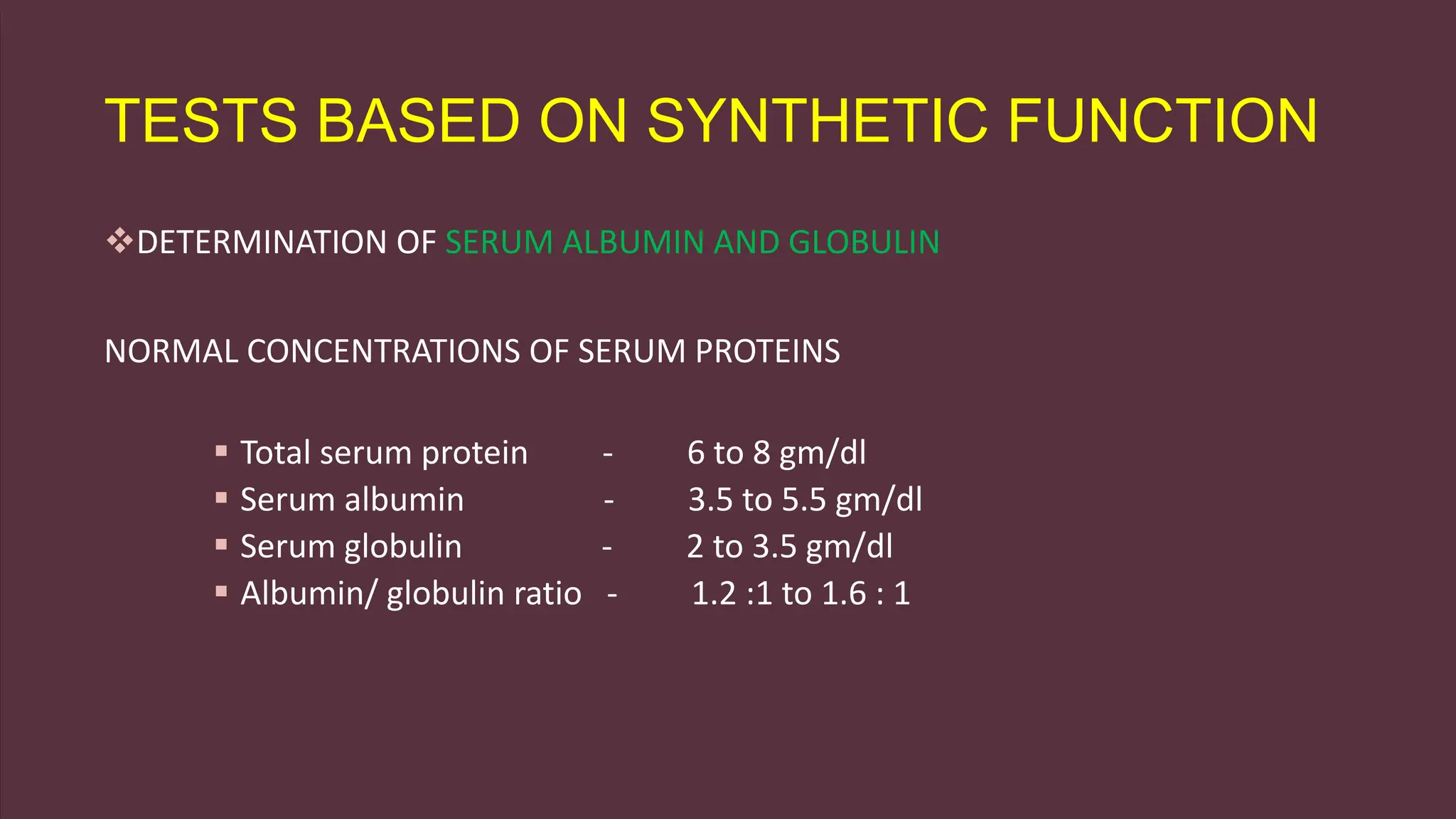
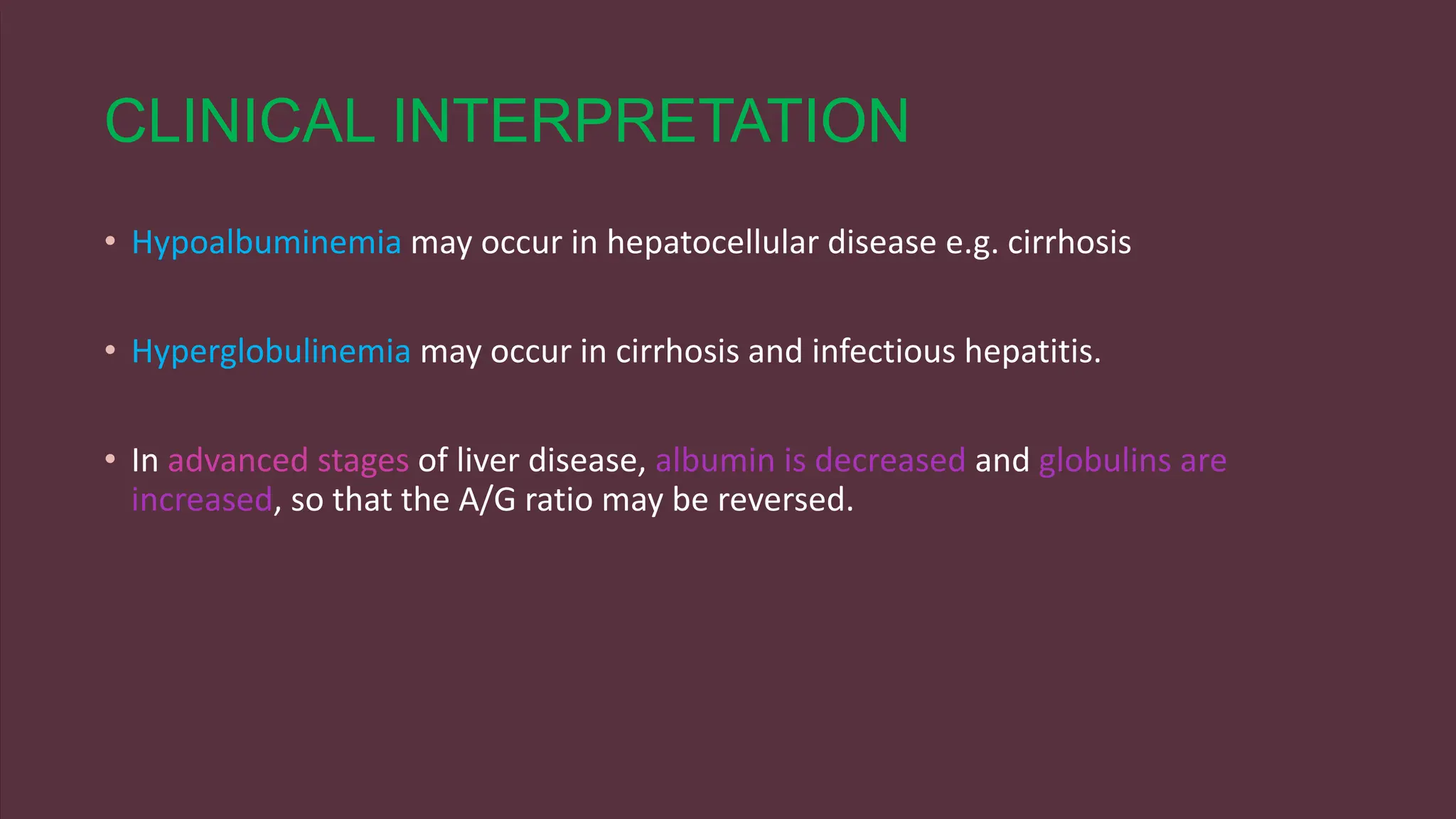
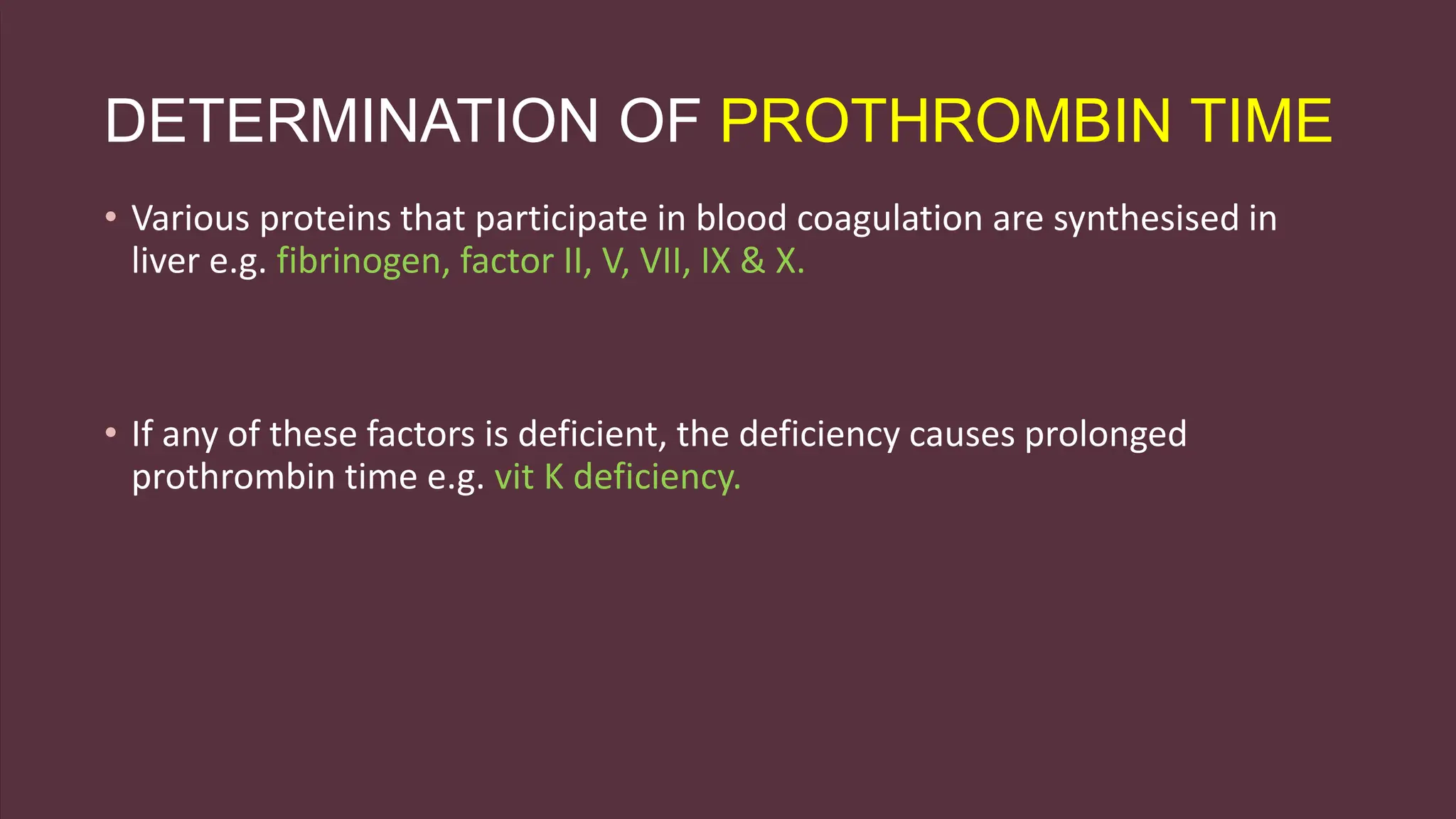
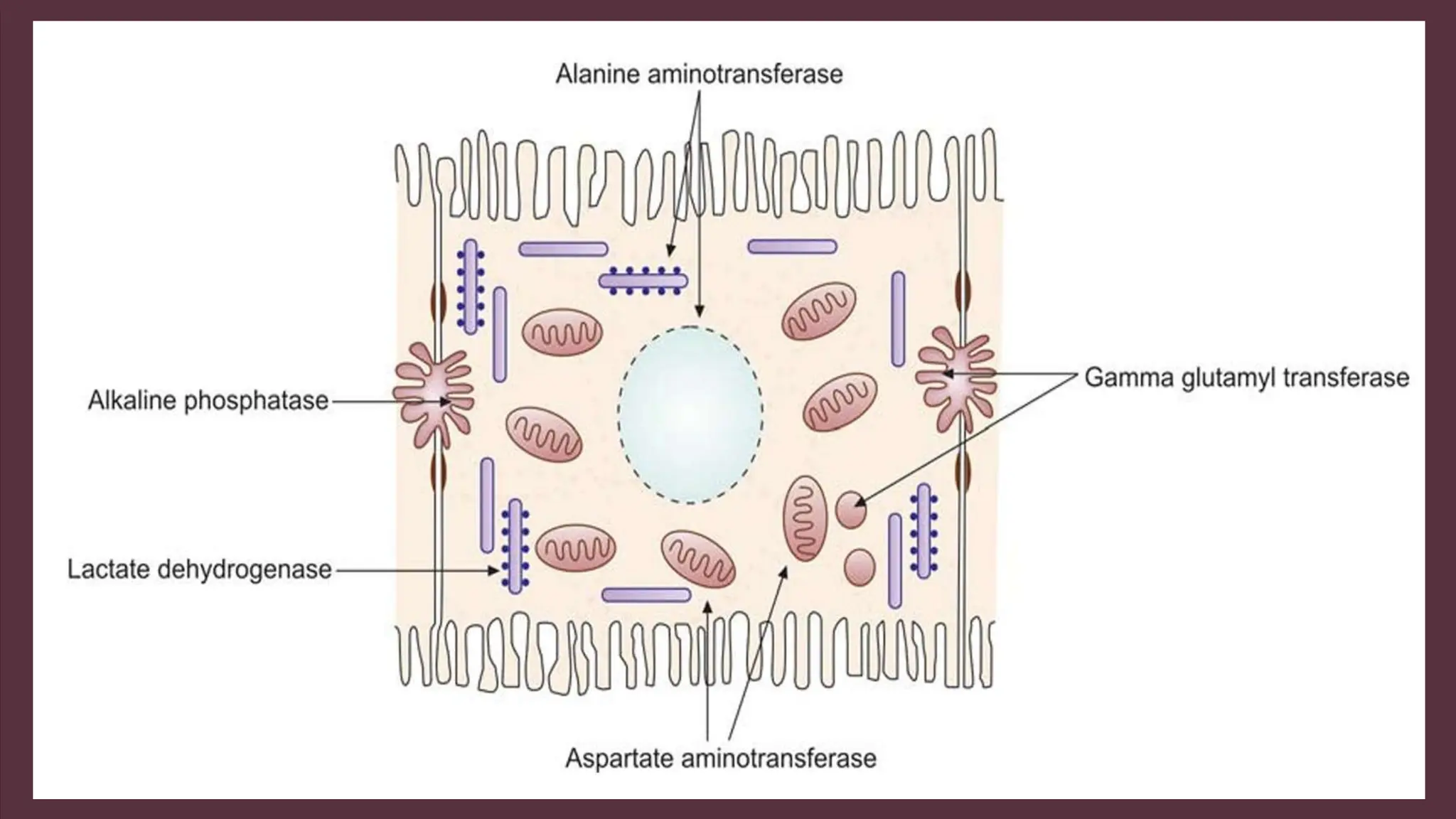
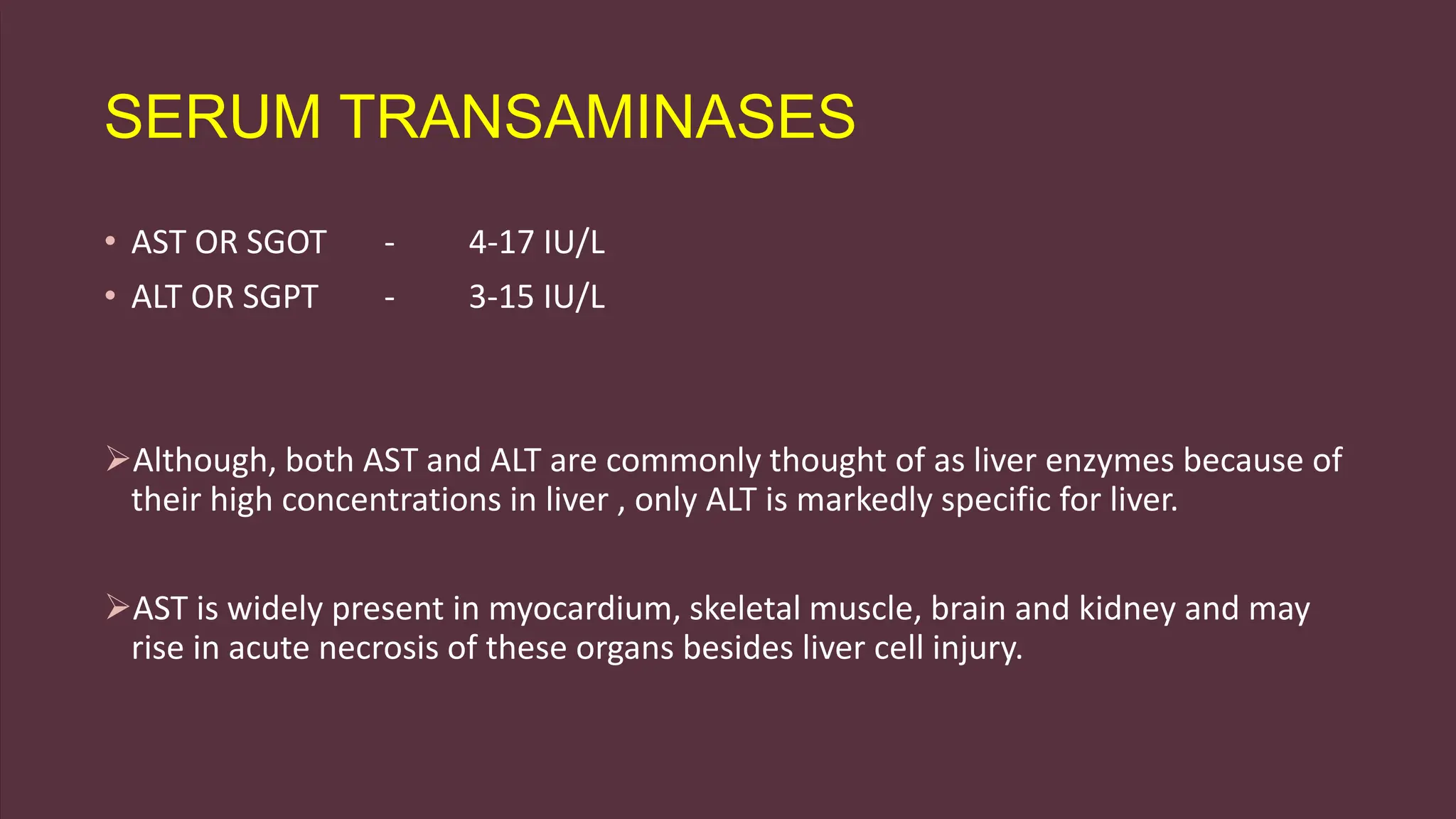
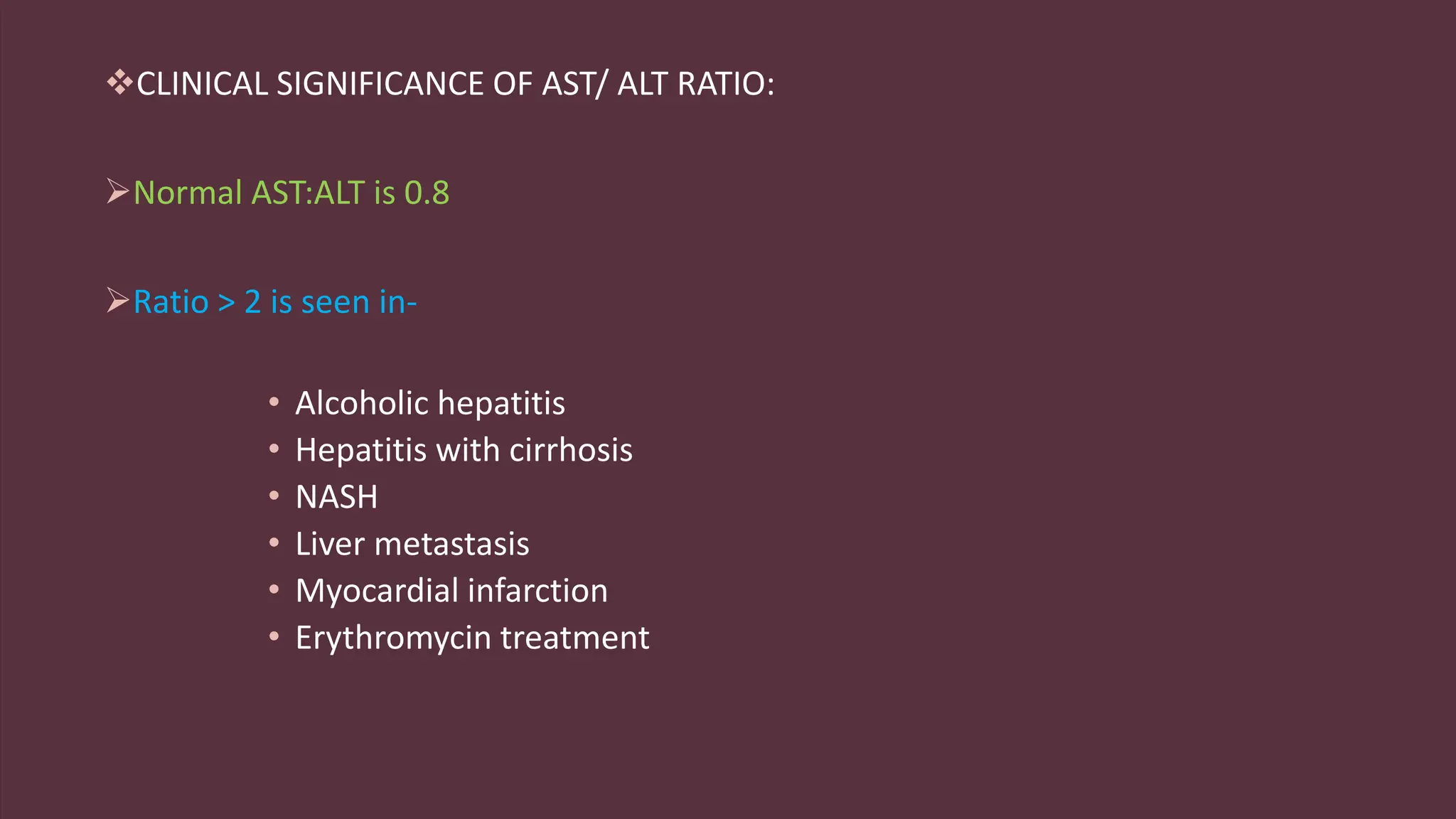
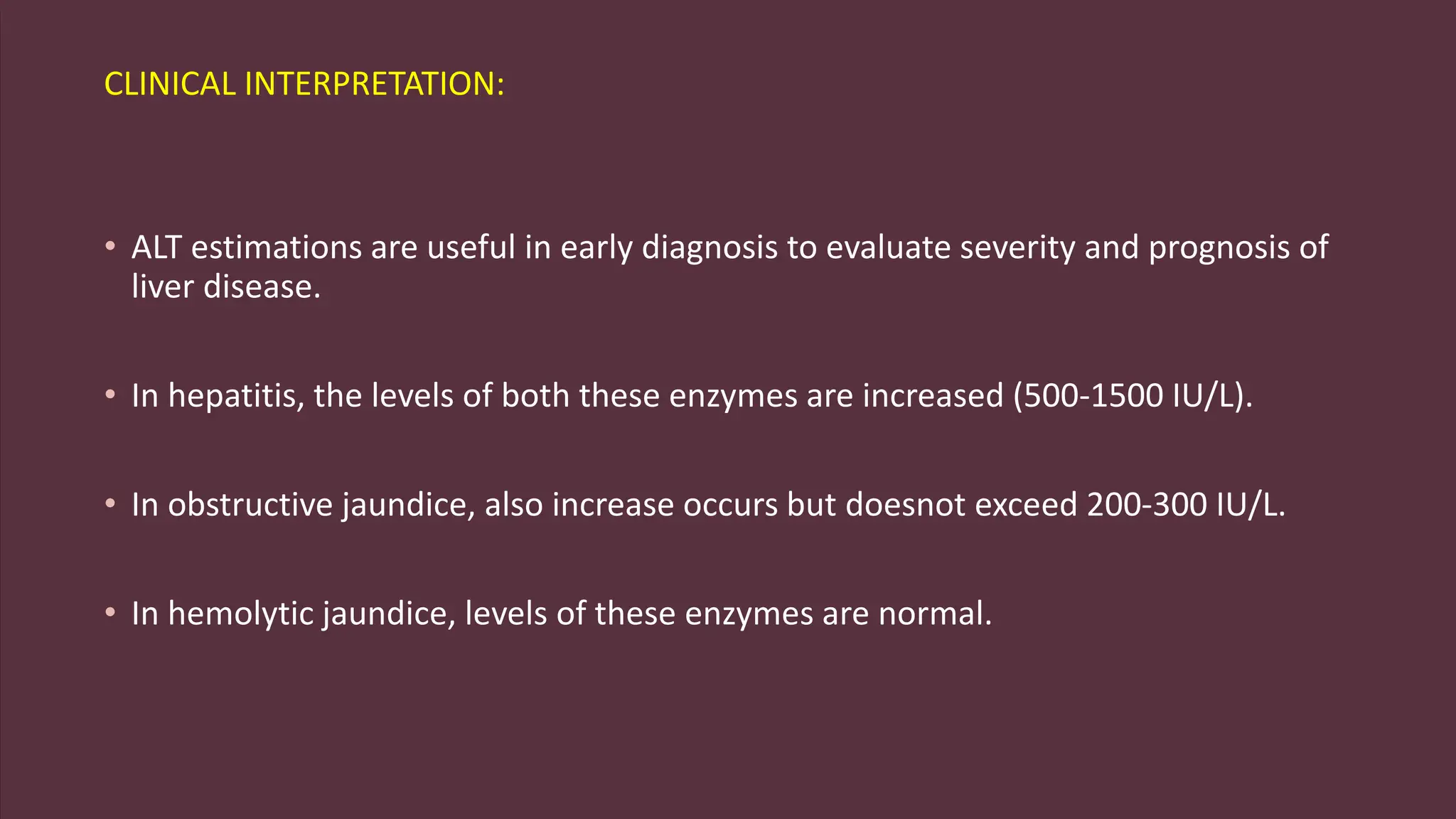
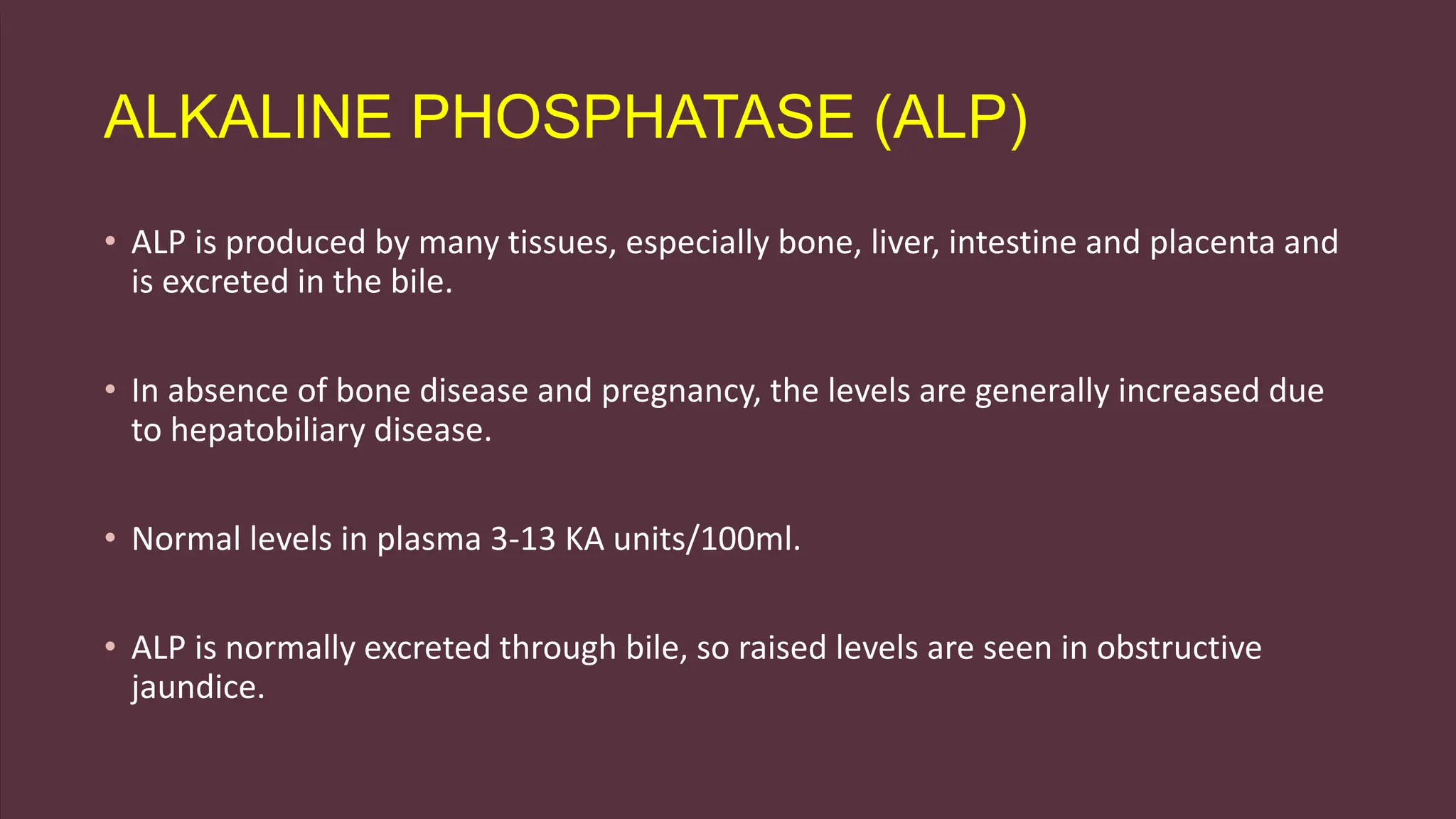
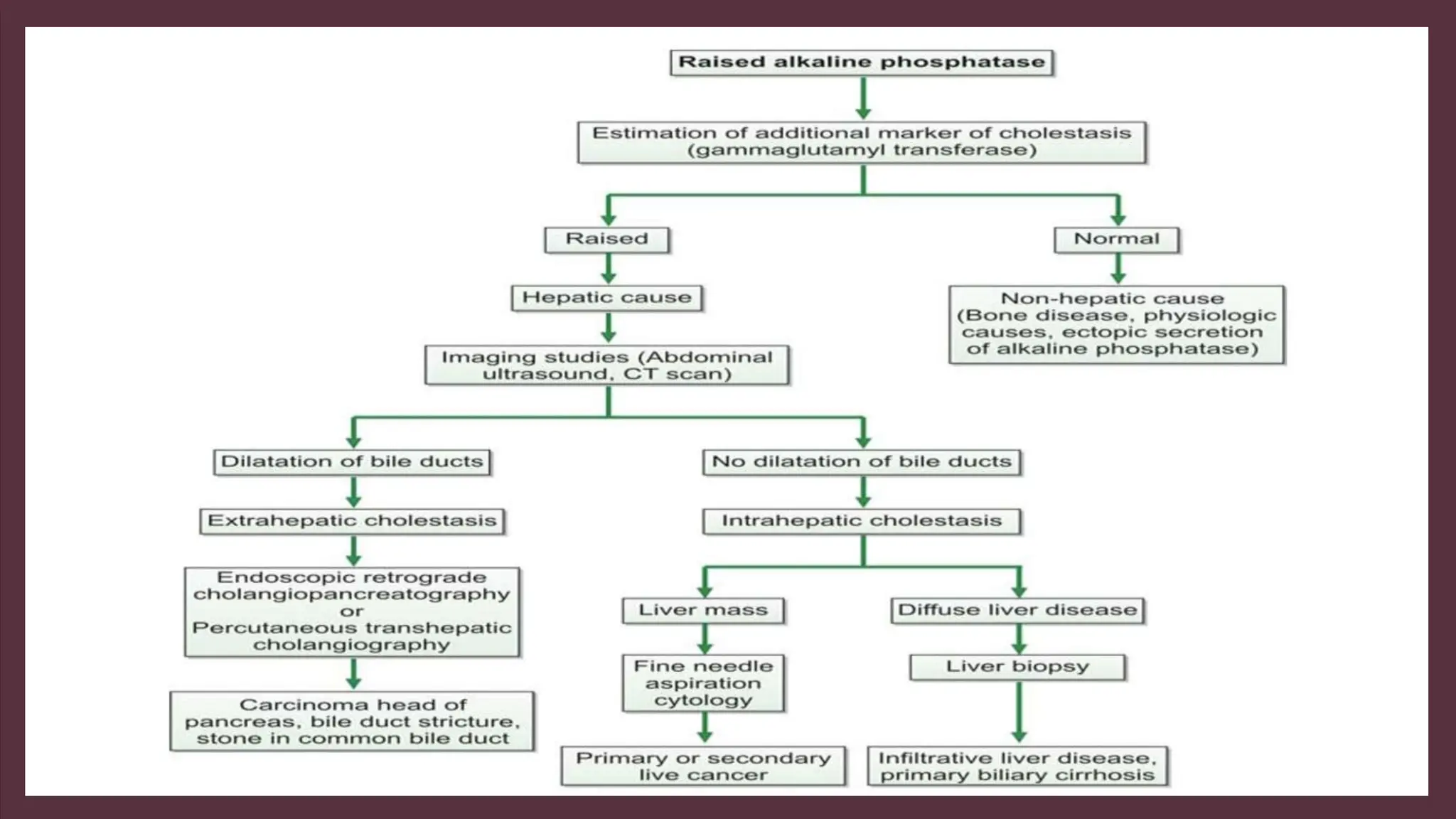
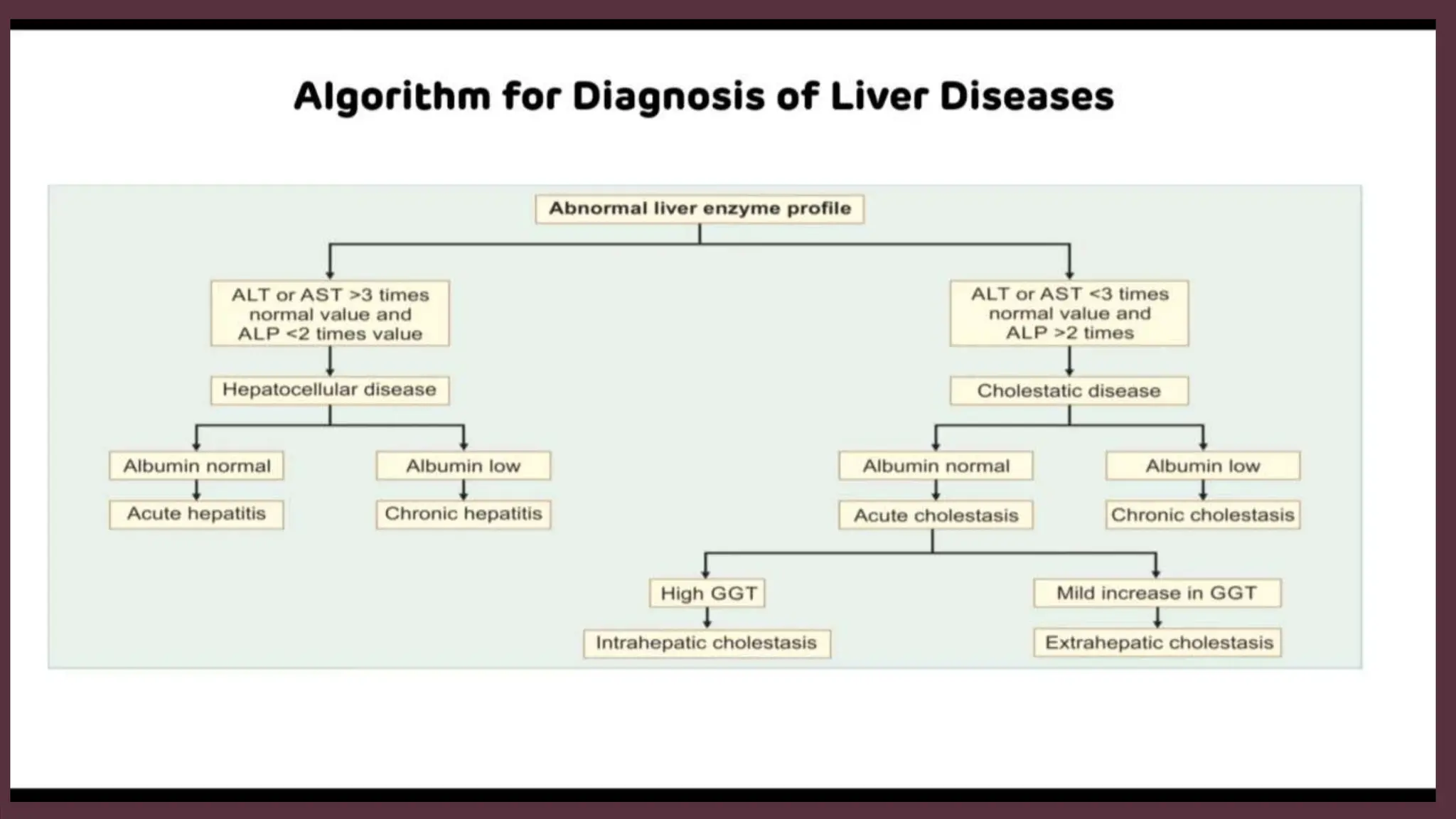
The document discusses liver function tests presented by Dr. Shruti Gera, detailing the liver's metabolic, synthetic, excretory, detoxification, regulatory, and storage functions. It outlines the various tests used to evaluate liver function, indications for testing, and the interpretation of results, specifically regarding bilirubin metabolism, ammonia detoxification, protein synthesis, and enzyme levels. The document emphasizes the significance of these tests in diagnosing and monitoring liver diseases, including their specific clinical implications.