Monday, February 17,
2014
side effects
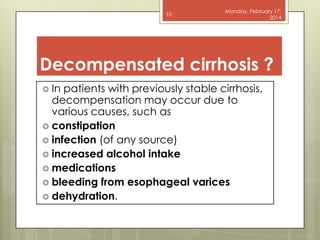
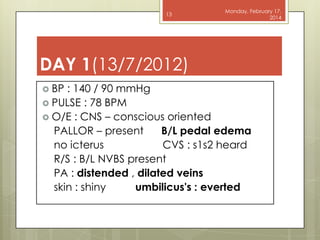
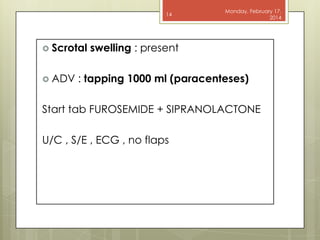
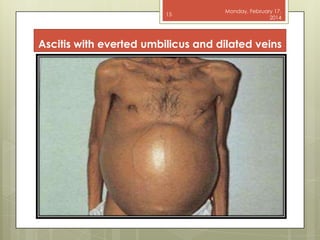
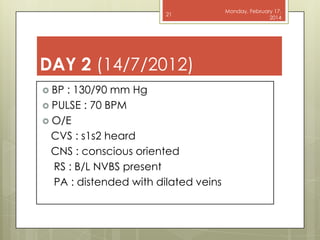
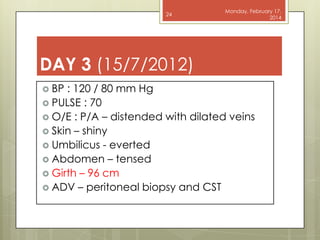
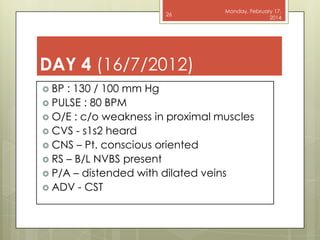
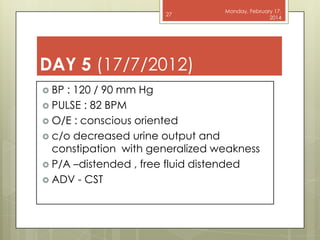
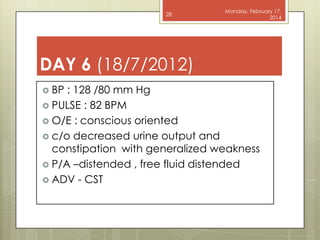
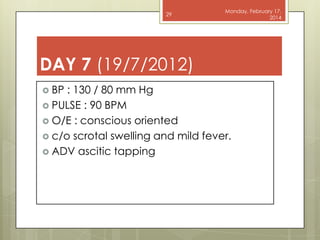
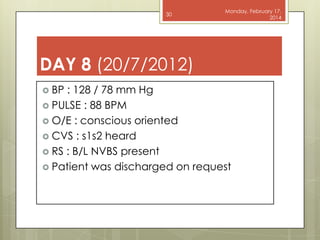
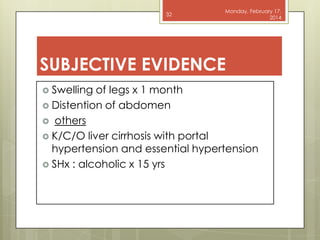
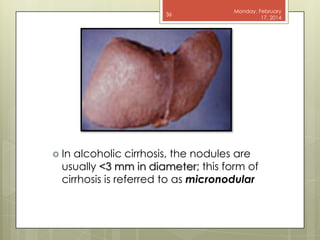
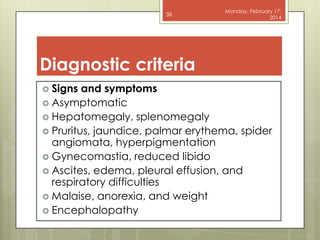
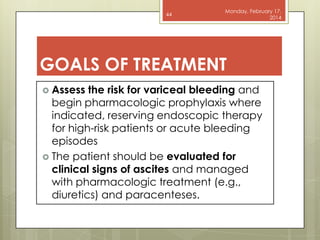
1) A 50-year-old male presented with swelling of the legs, abdominal distension, and constipation for 1 month and was diagnosed with liver cirrhosis with decompensation and portal hypertension based on his history of alcohol use for 15 years.
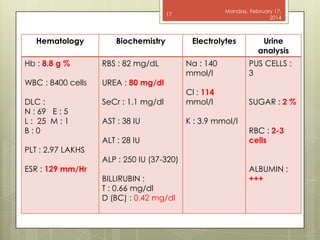
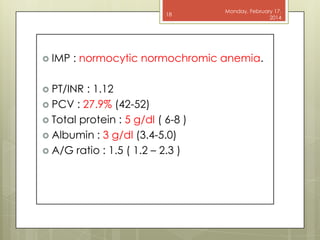
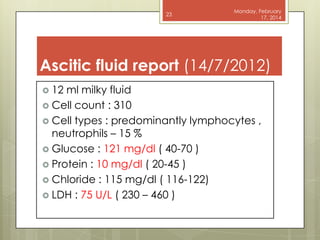
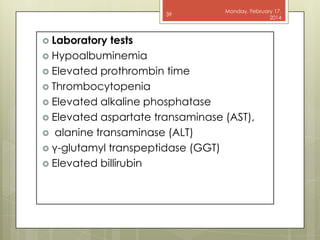
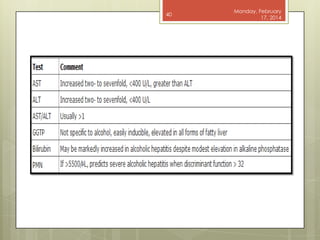
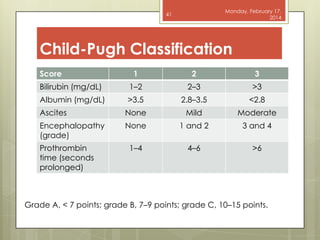
2) Laboratory tests showed anemia, elevated bilirubin and decreased albumin consistent with liver disease.
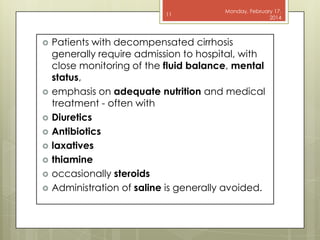
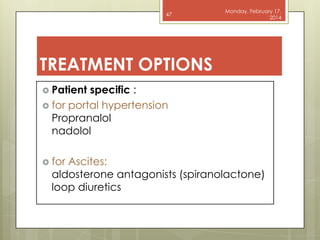
3) He was treated with paracentesis, diuretics, and discharged after 8 days of inpatient management with improvement of symptoms.