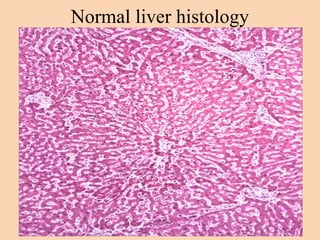
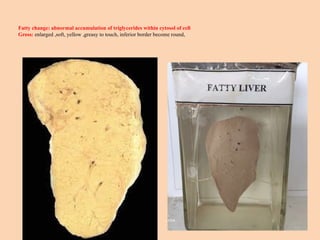
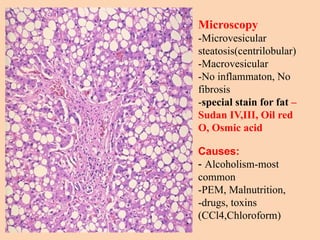
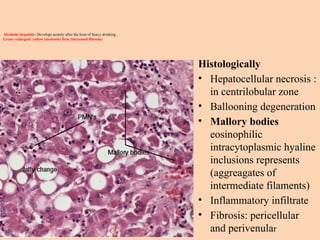
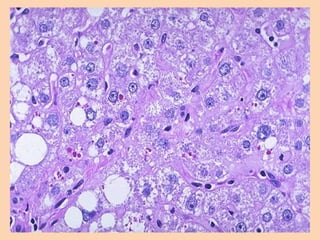
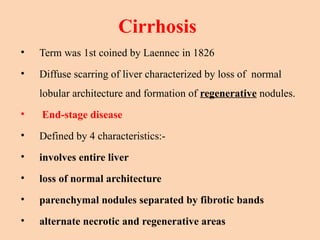
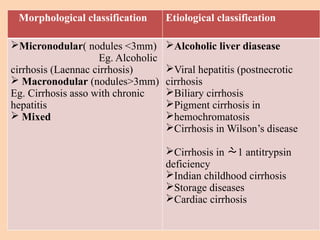
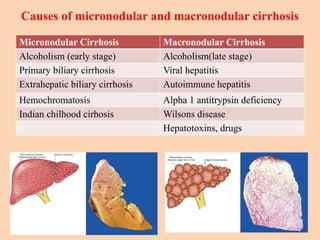
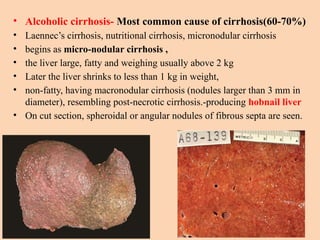
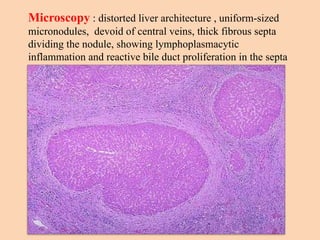
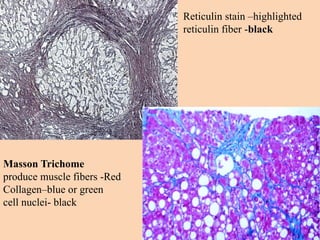
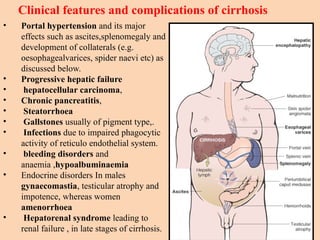
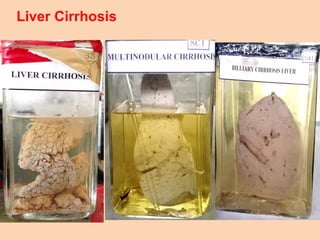
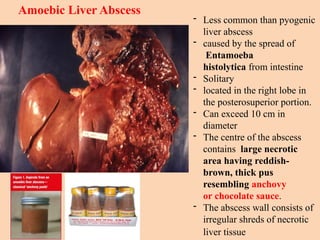
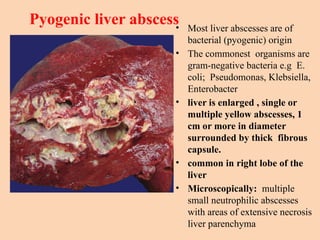
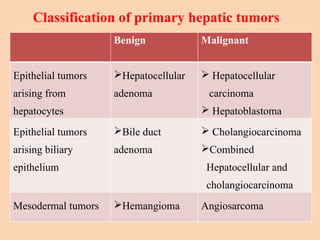
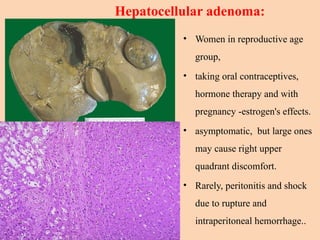
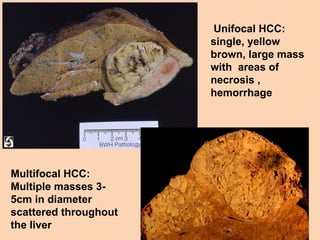
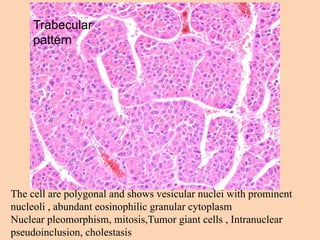
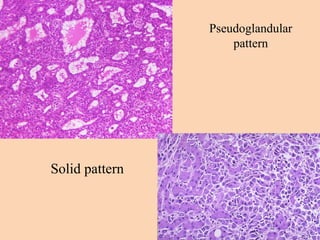
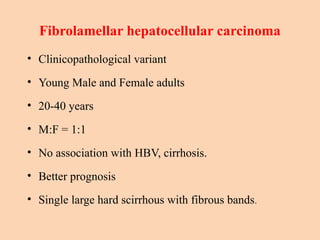
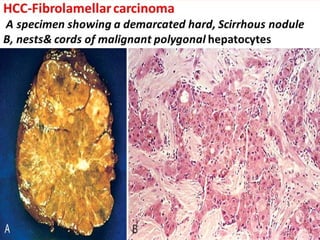
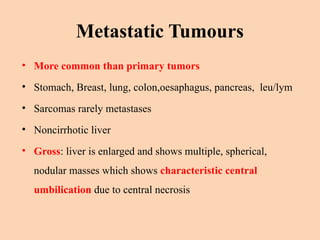
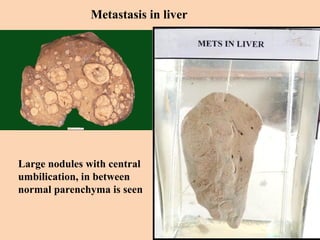
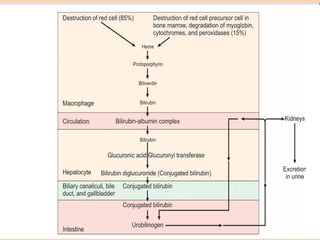
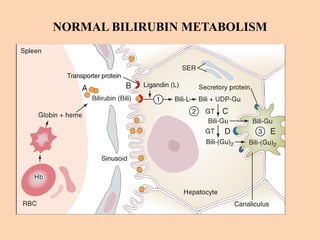
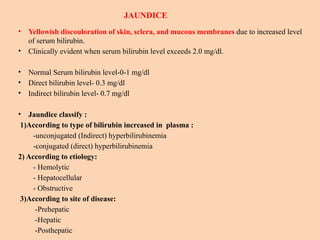
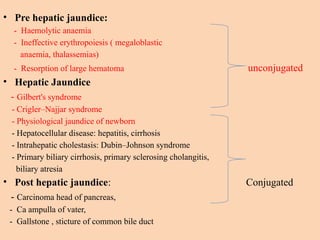
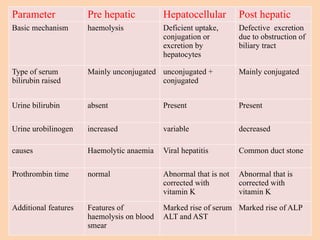
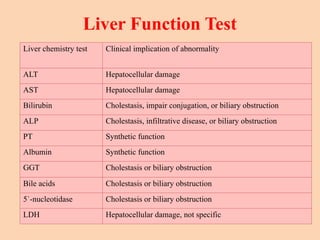
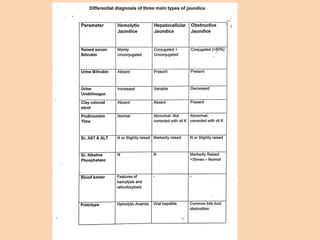
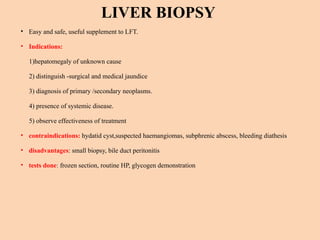
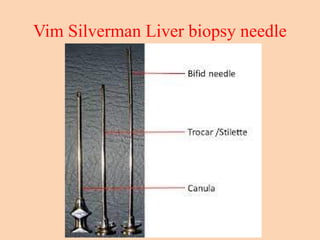
The document provides an overview of liver pathology, including conditions such as fatty liver, cirrhosis, alcoholic liver diseases, and liver tumors. It details the causes, histological features, and clinical implications of various liver disorders, as well as classifications of hepatic tumors. Additionally, it discusses liver function tests and indications for liver biopsy, emphasizing the importance of recognizing liver disease and its complications.