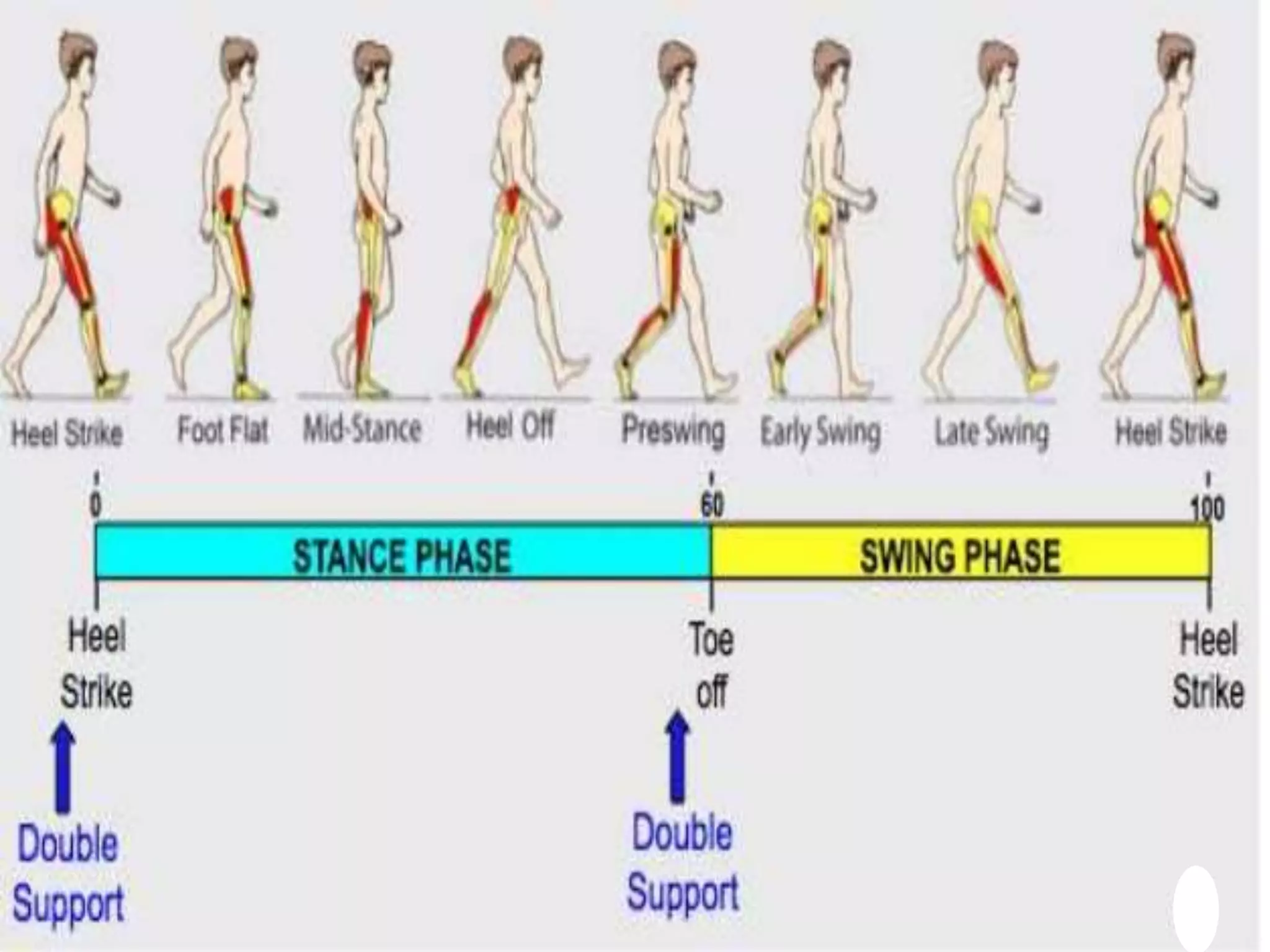
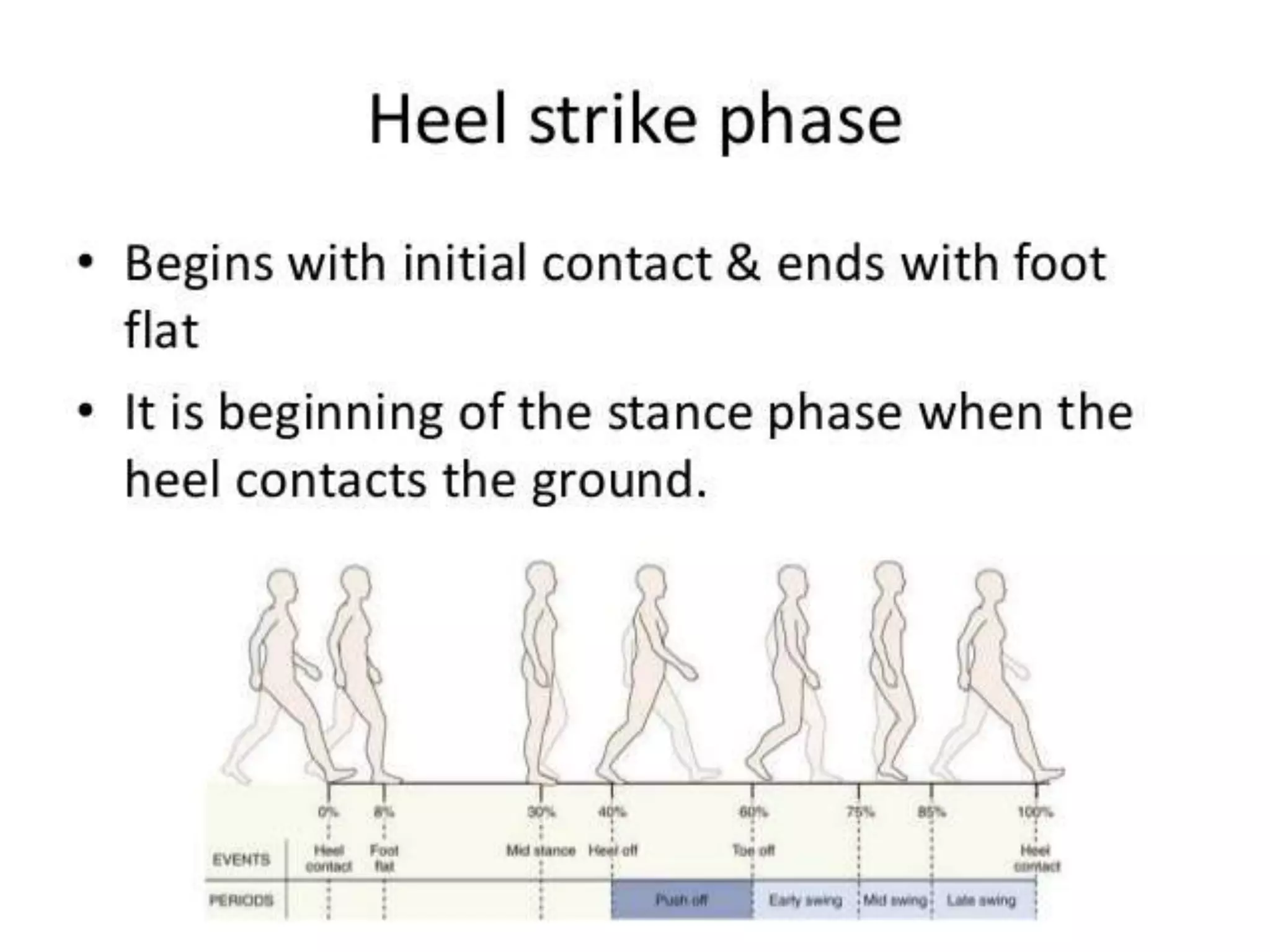
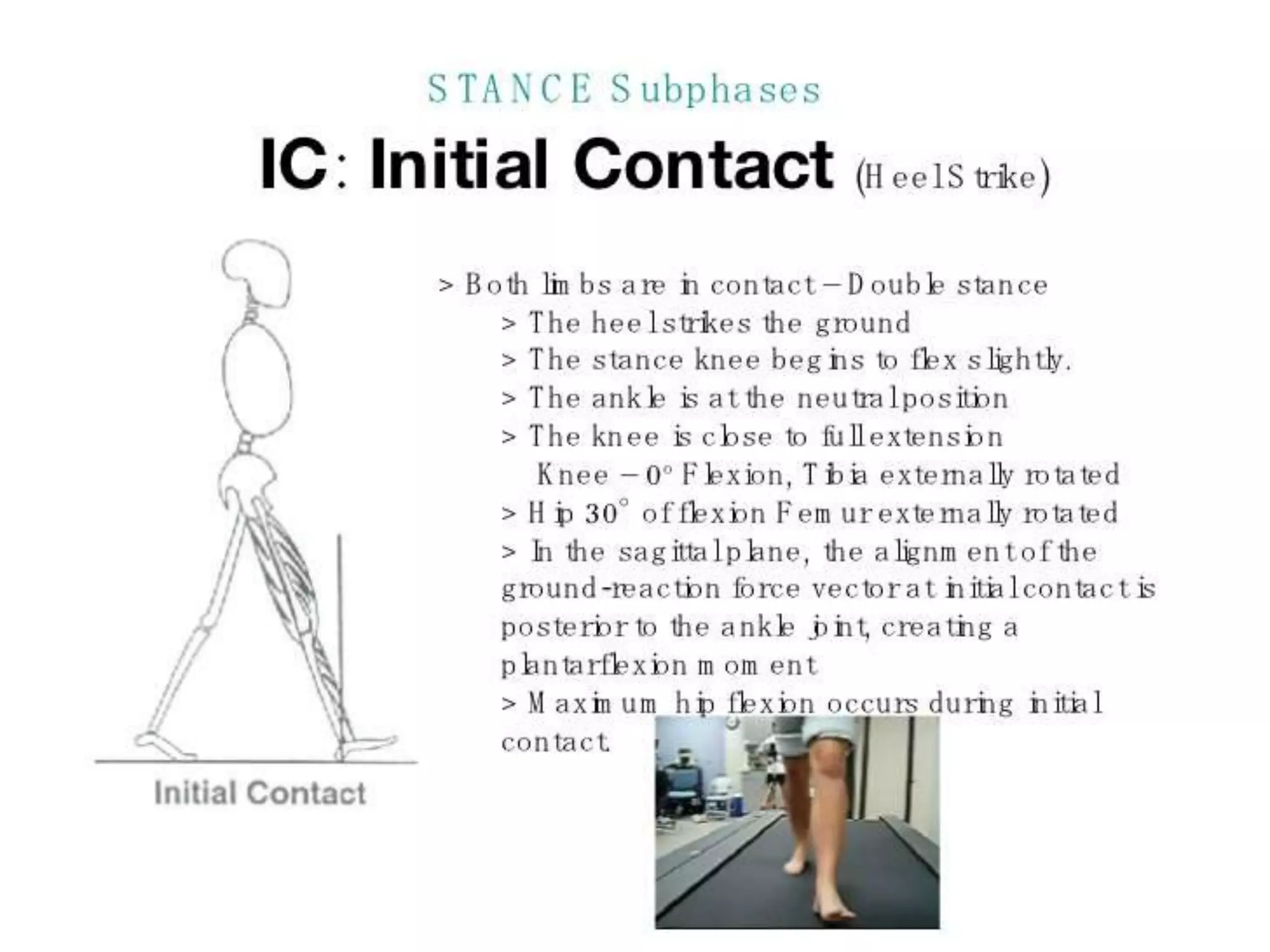
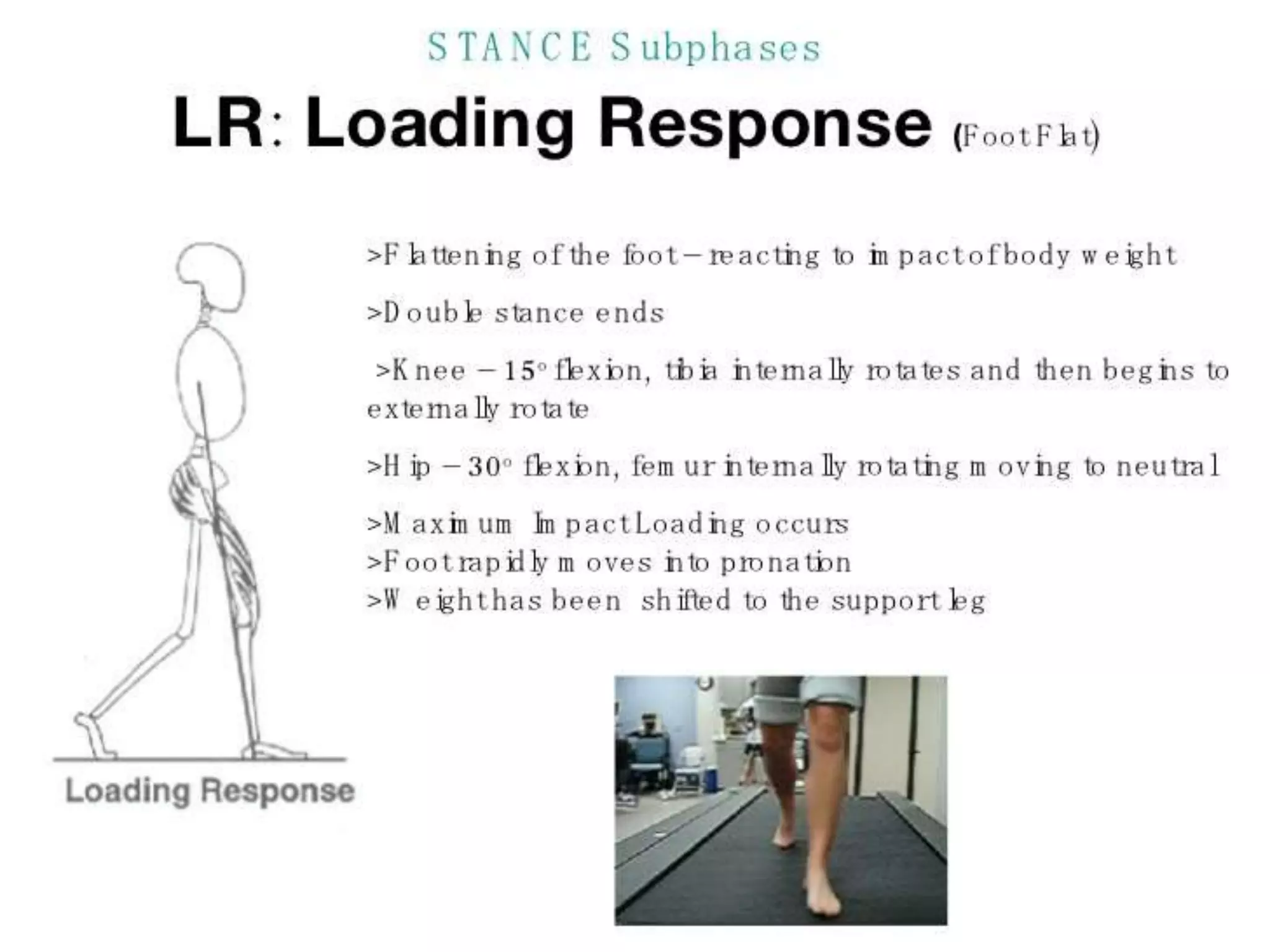
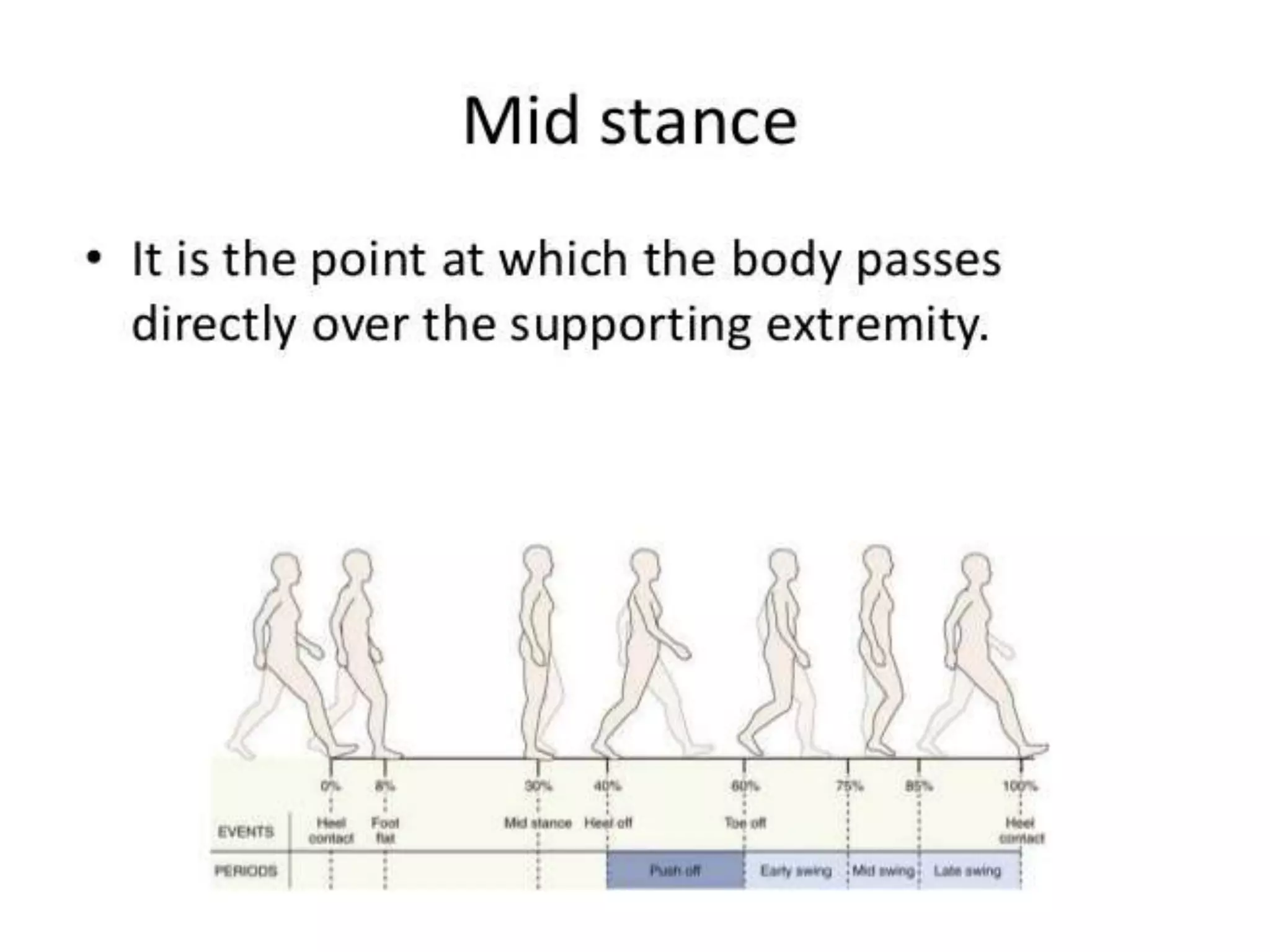
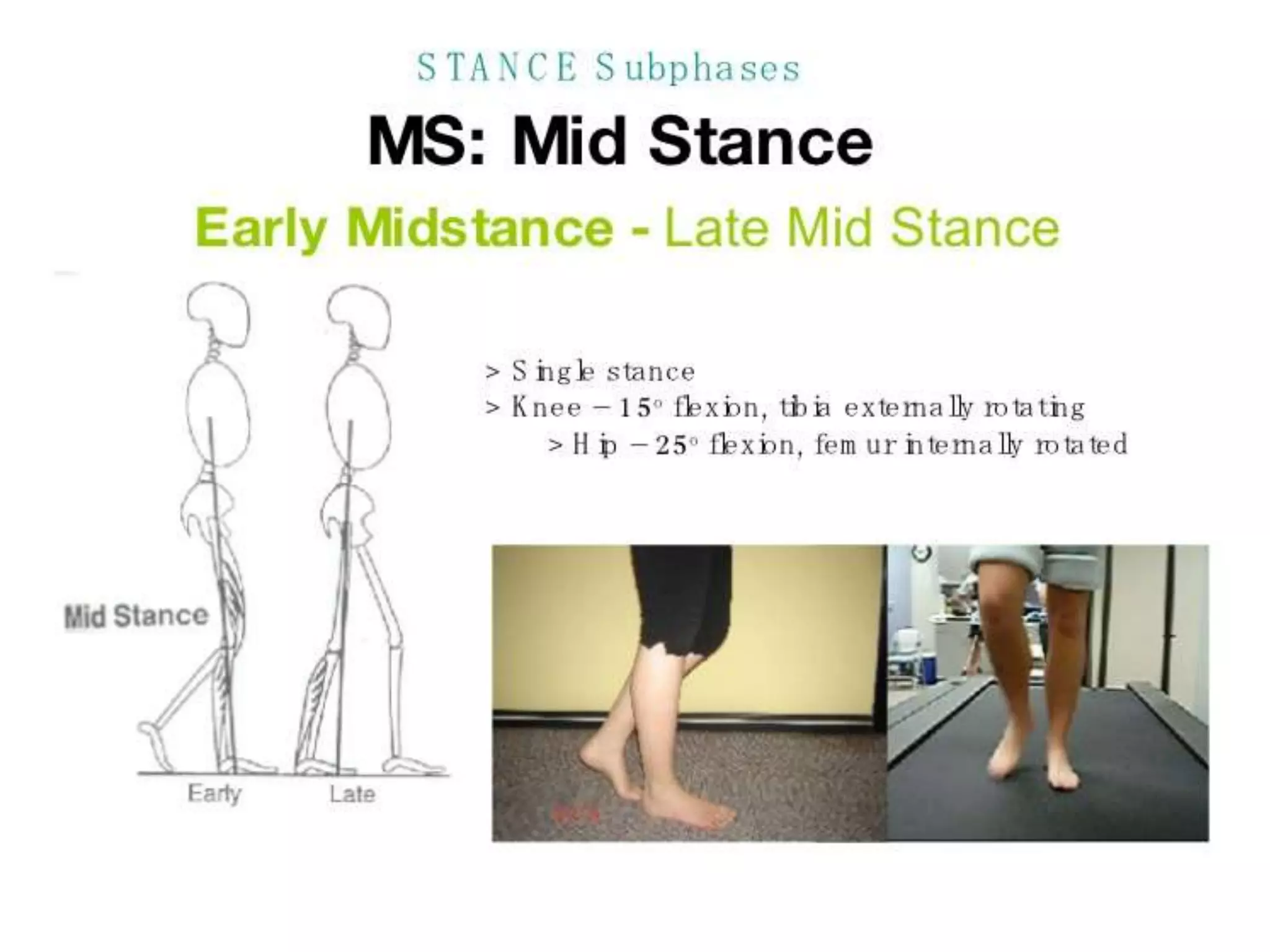
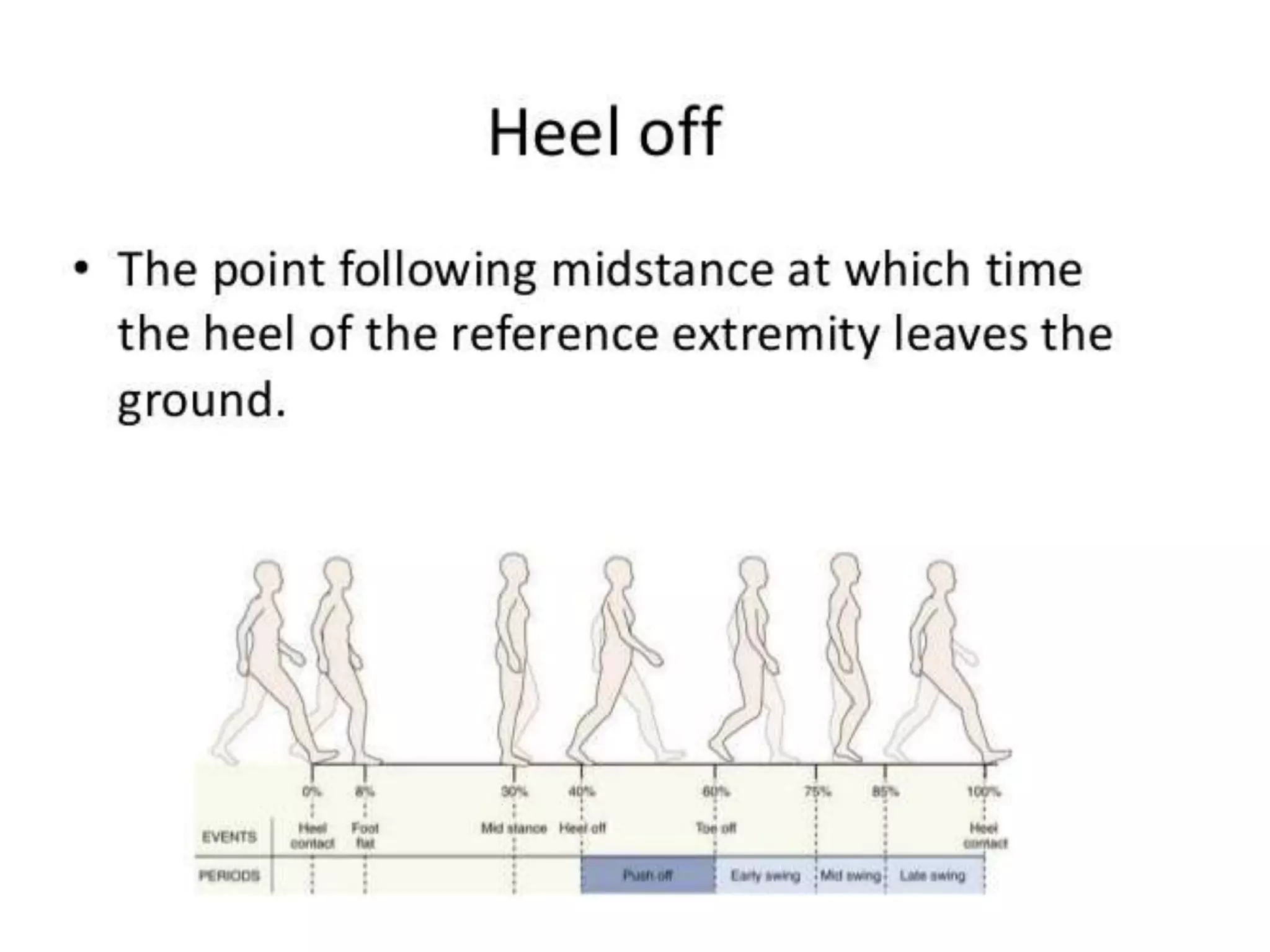
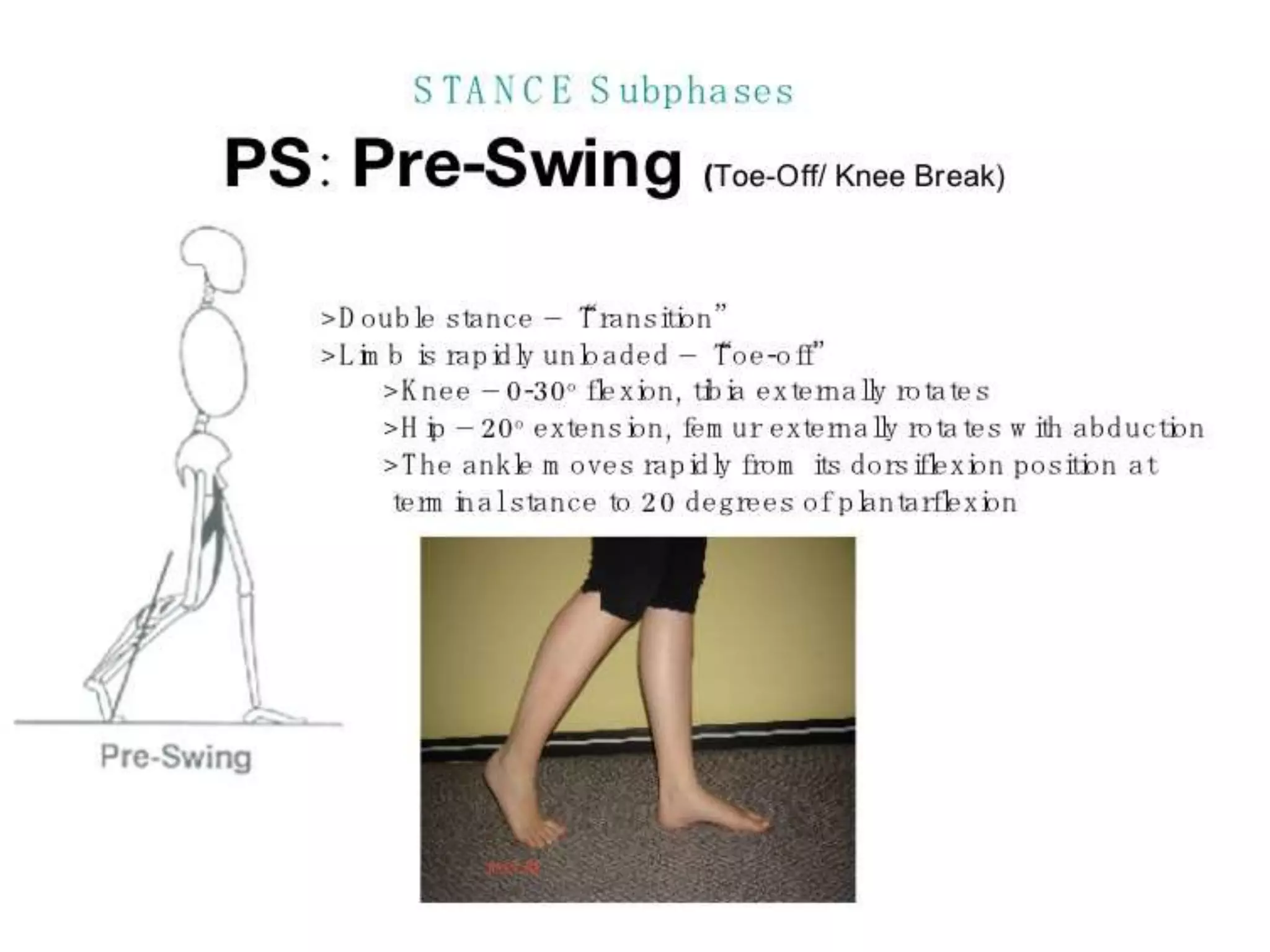
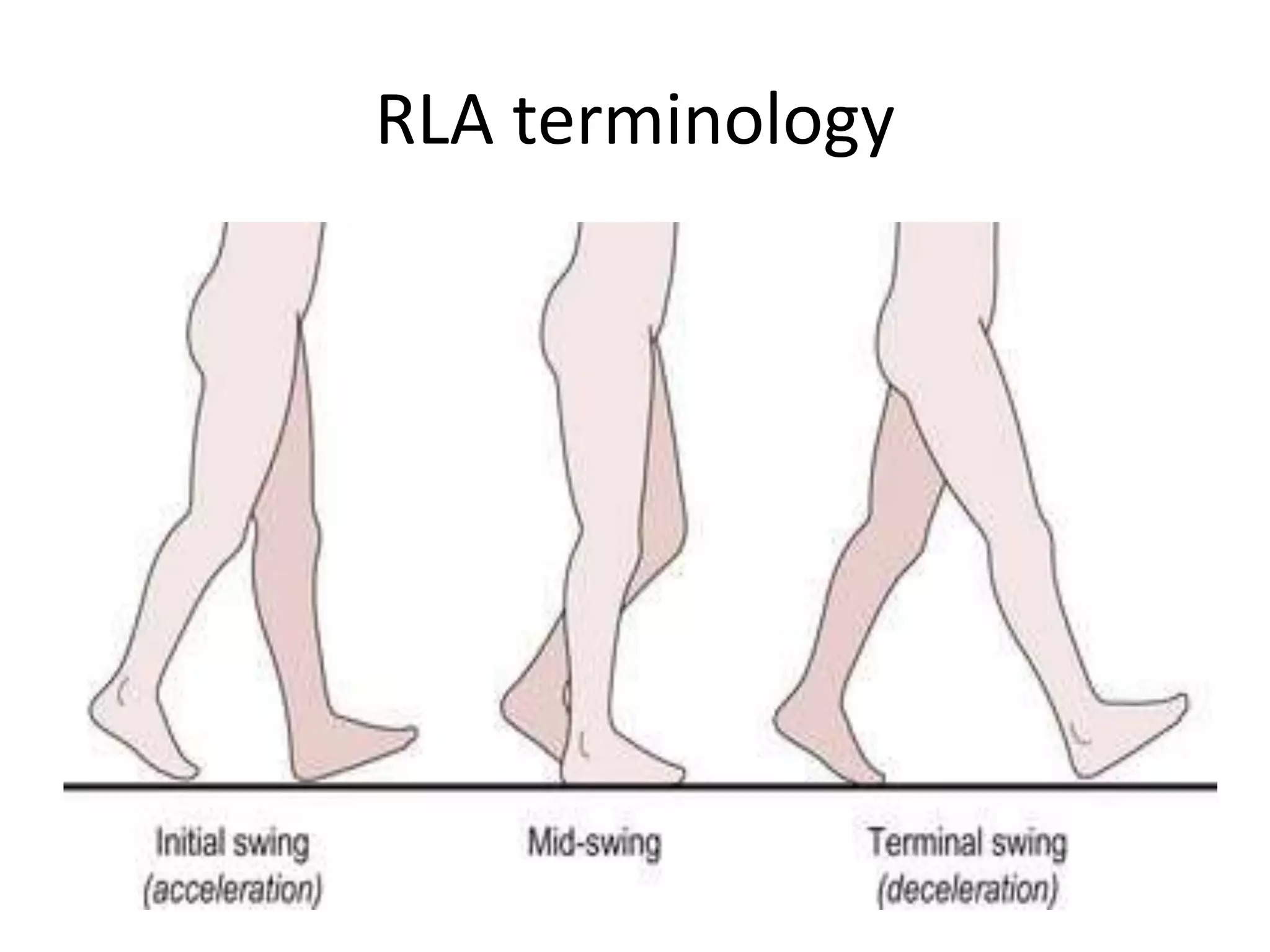
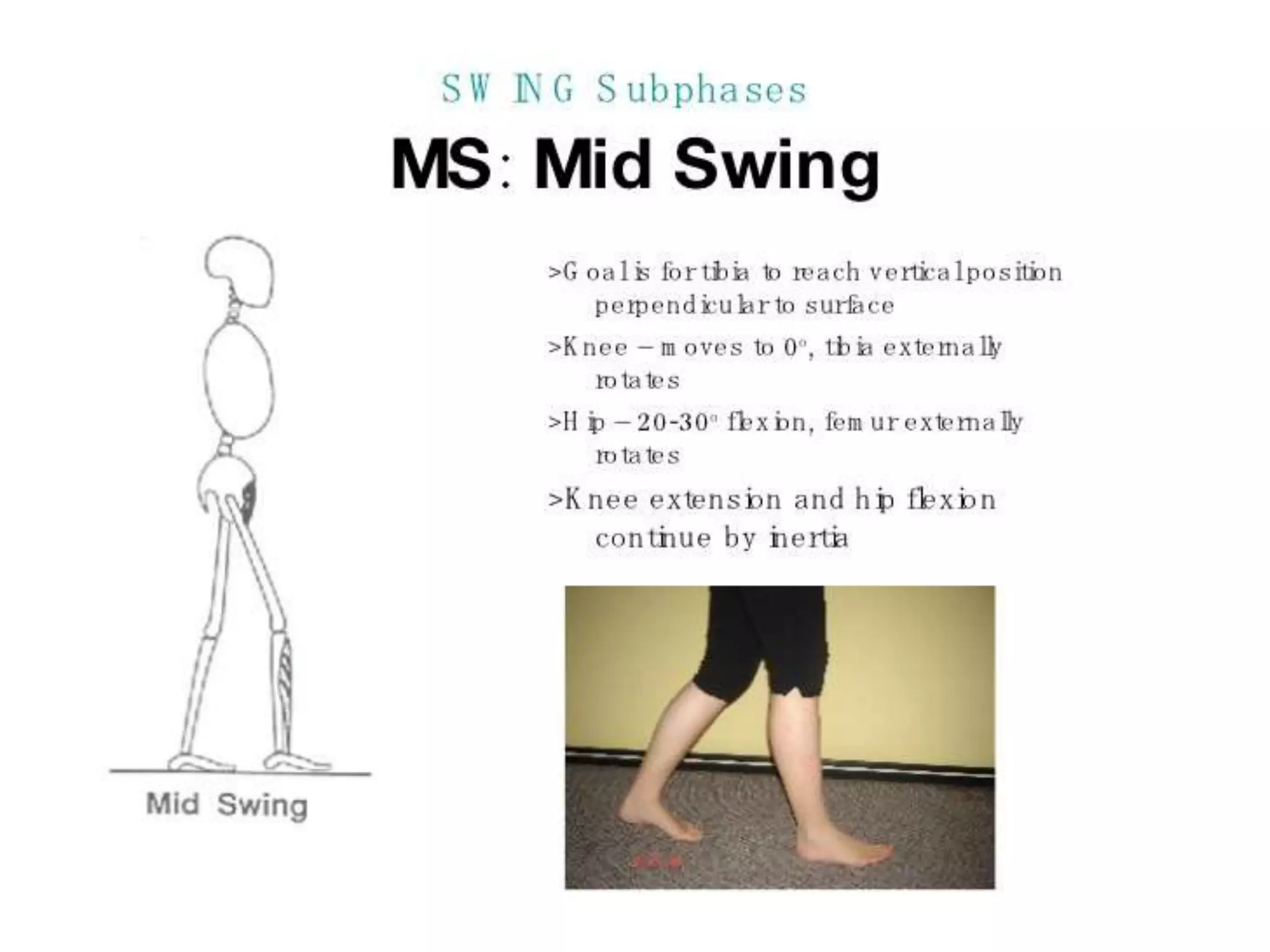
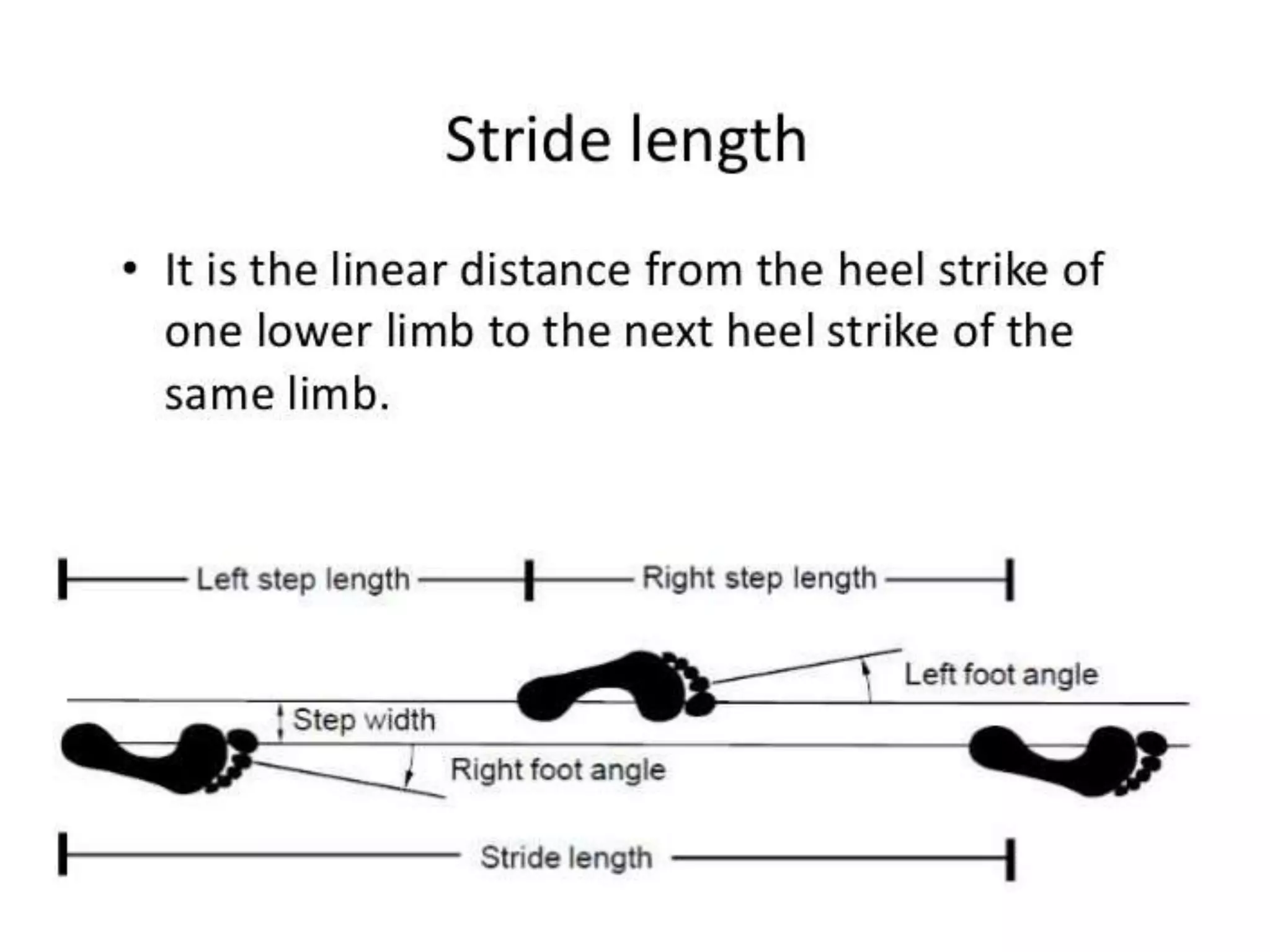
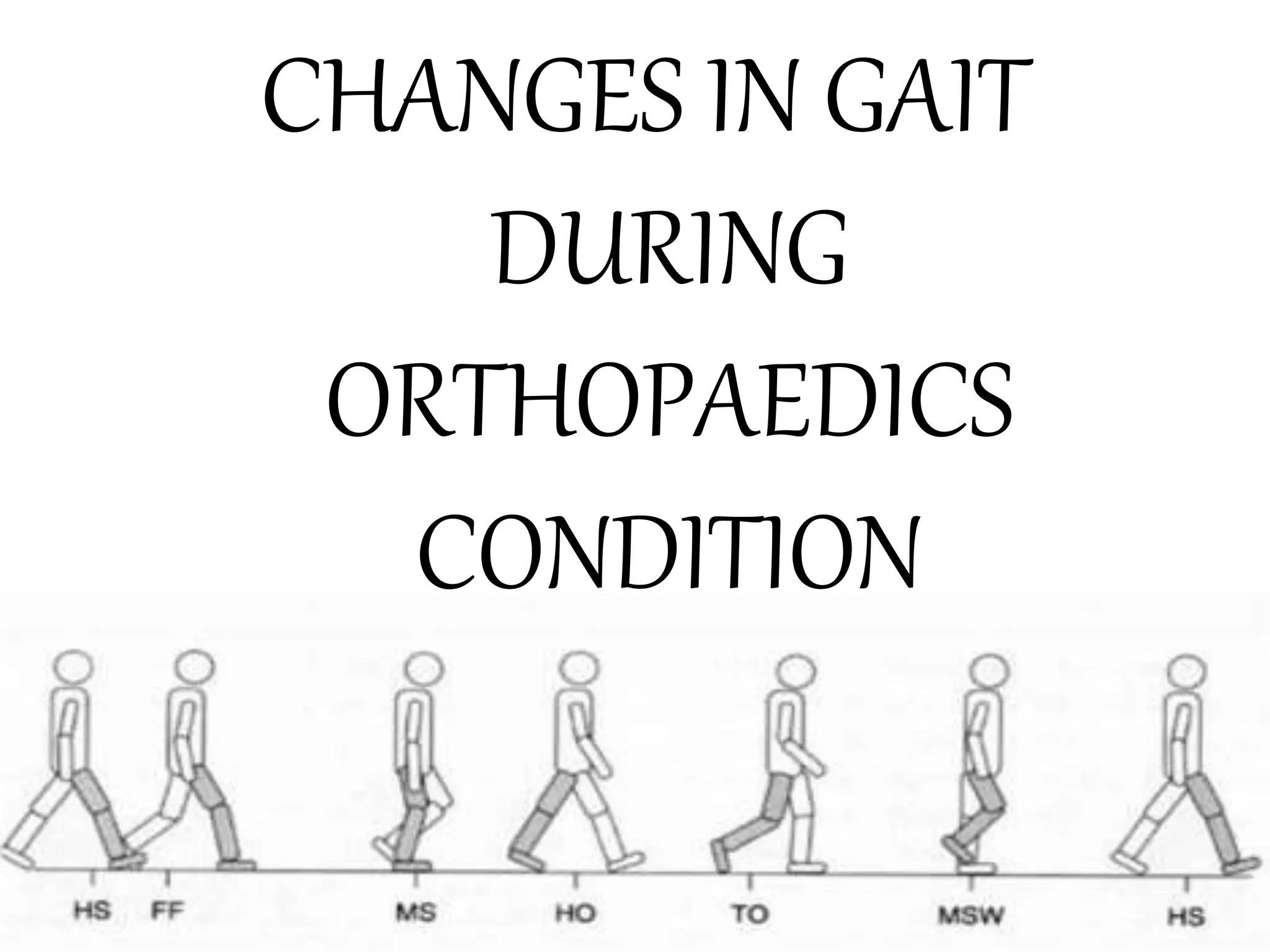
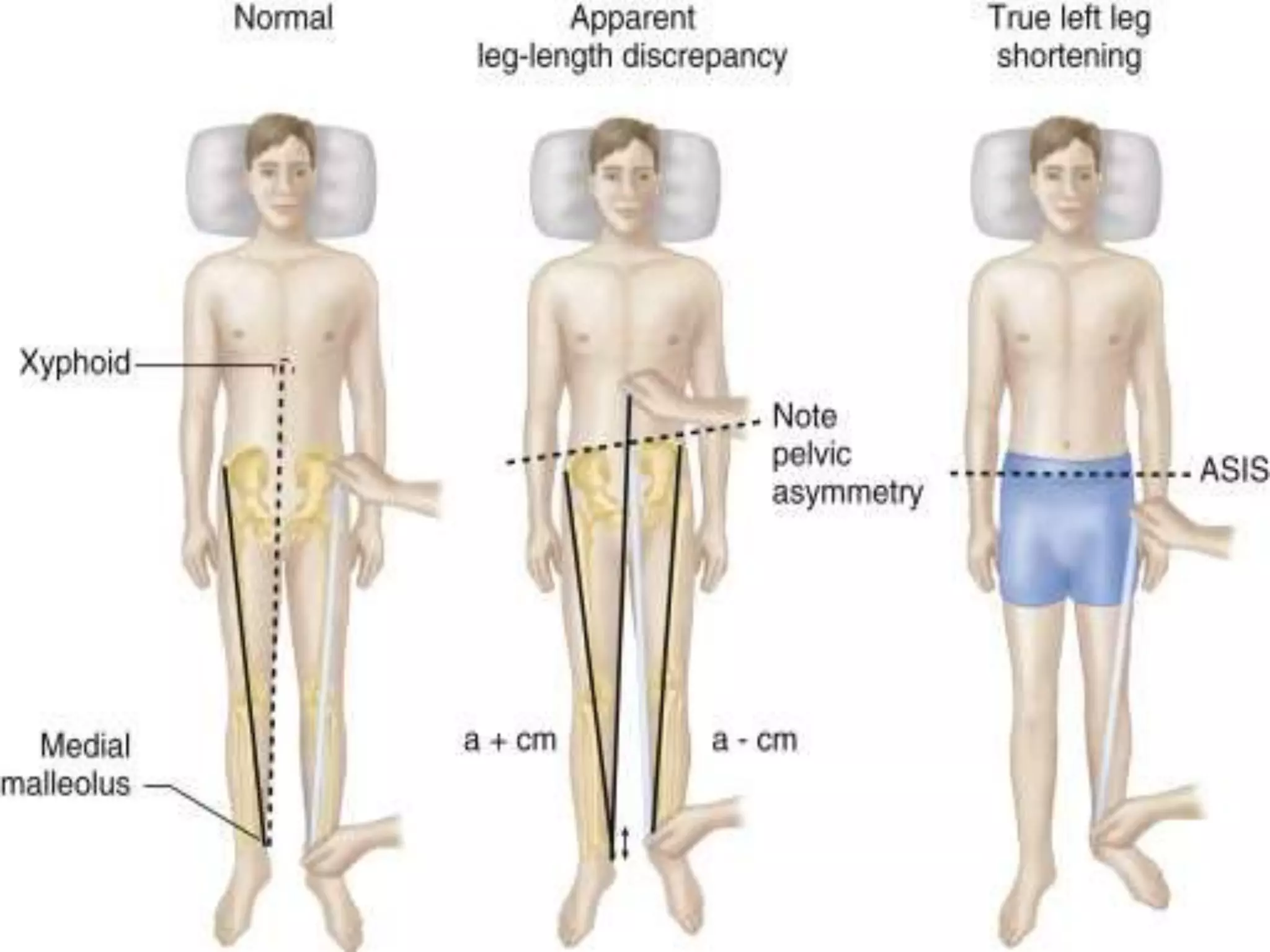
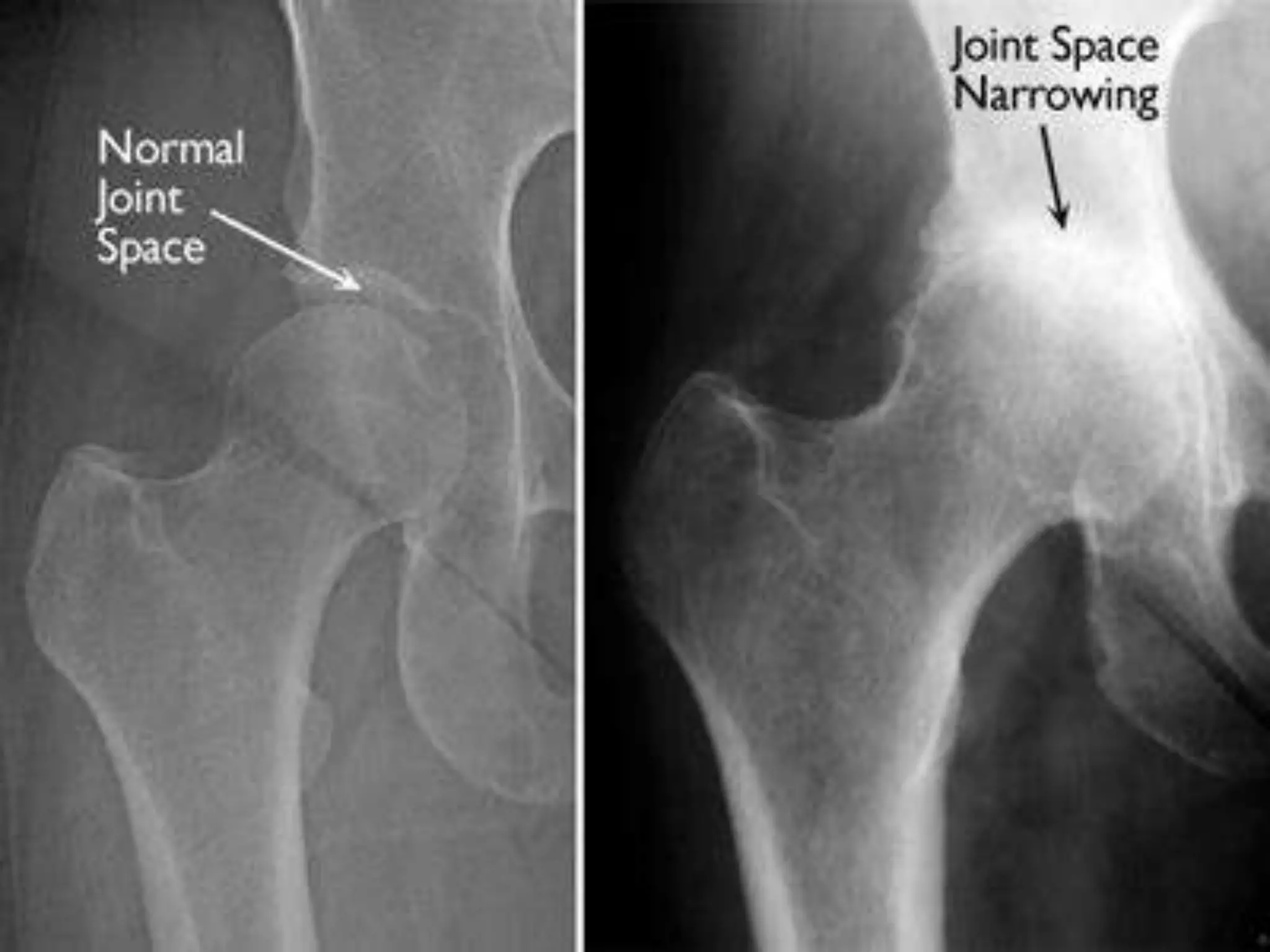
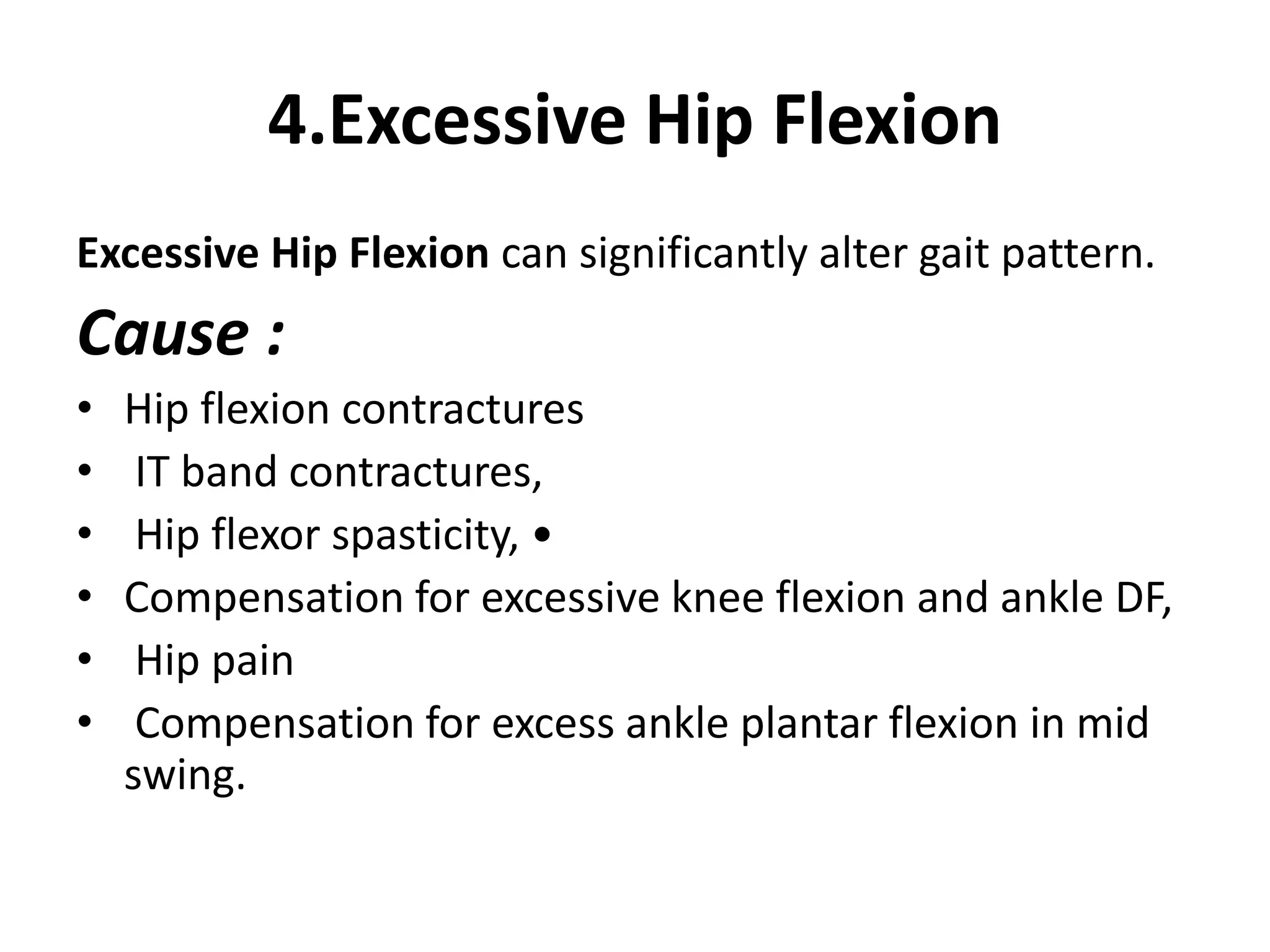
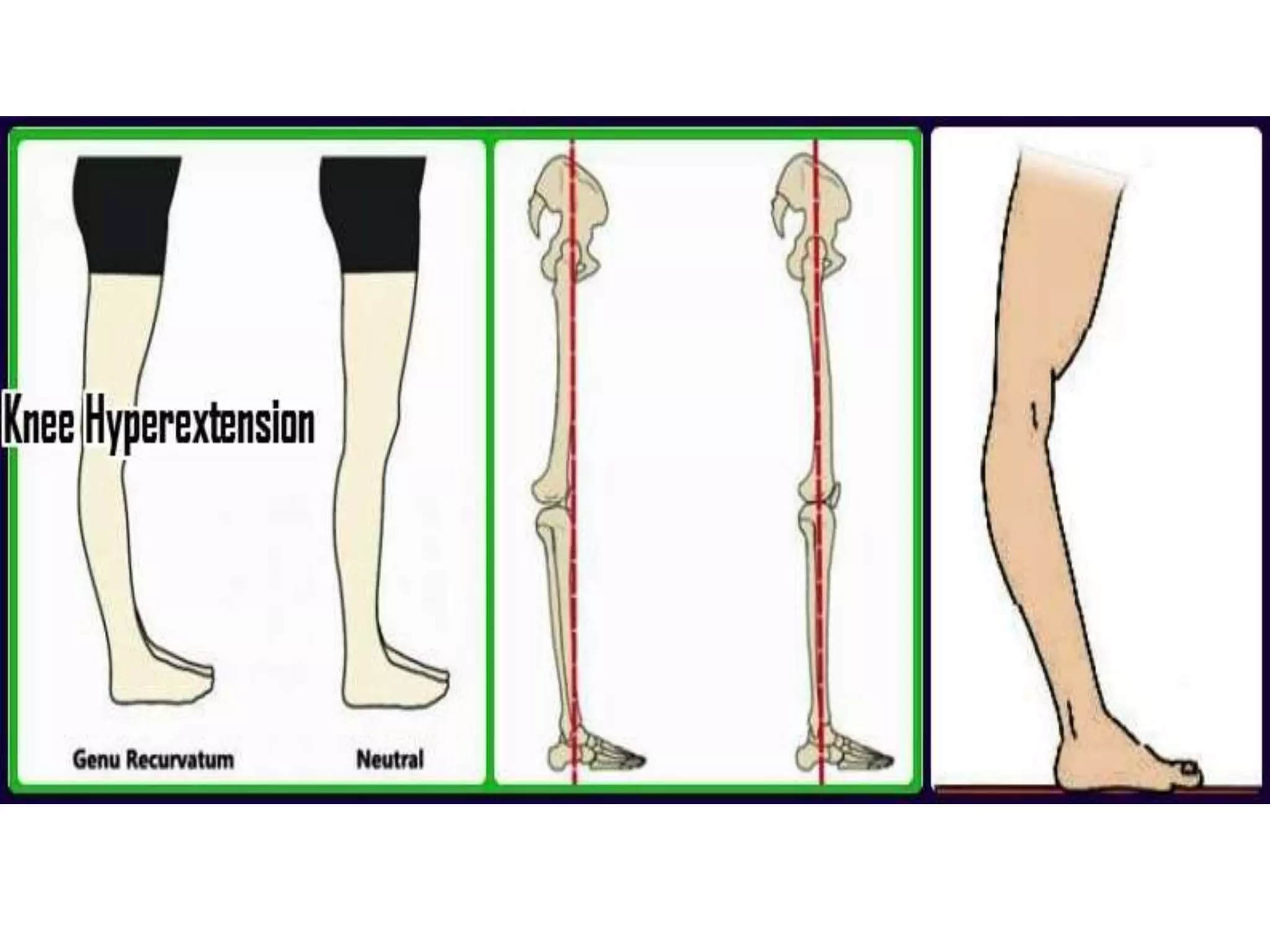
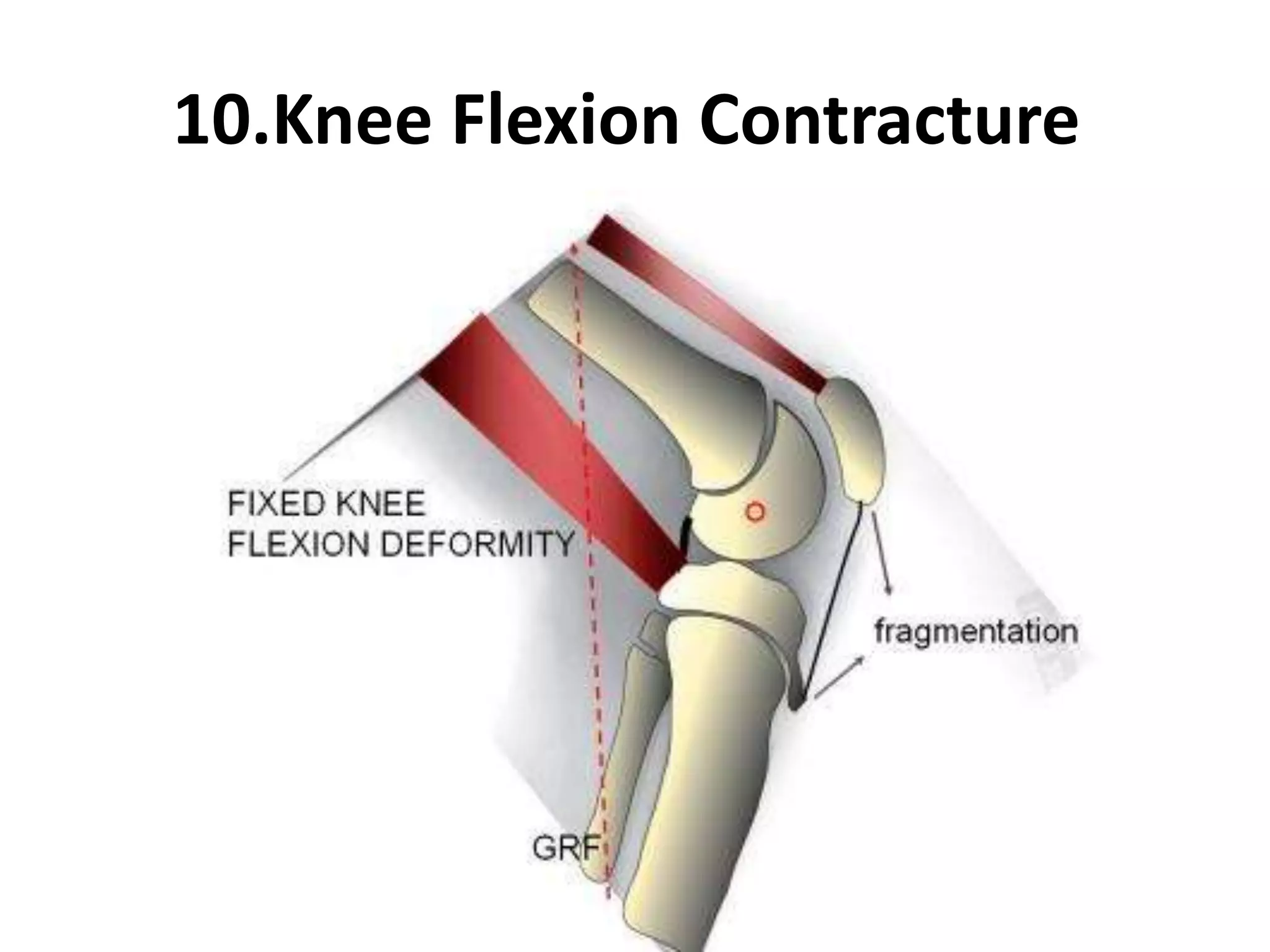
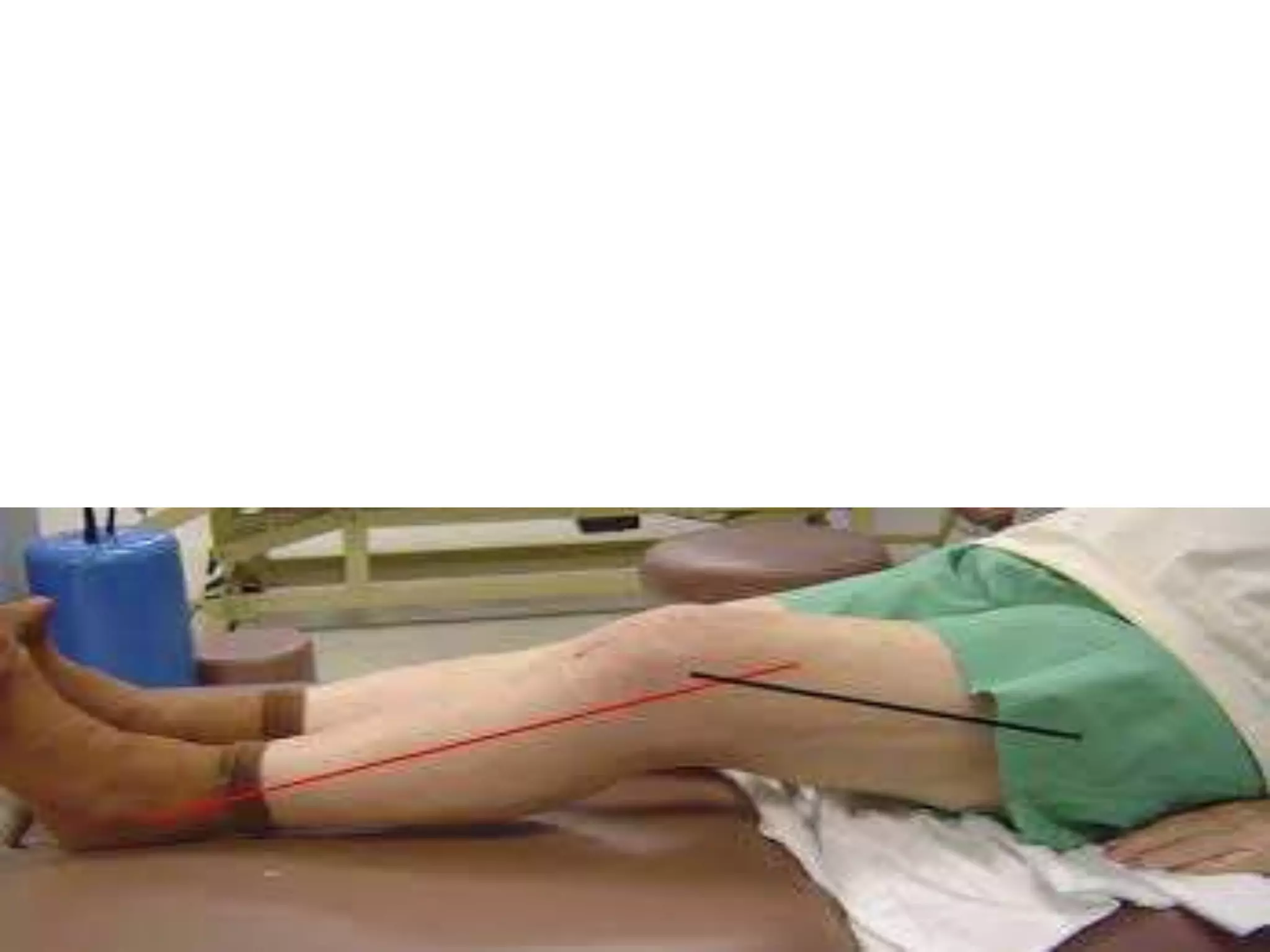
This document discusses changes in gait that can occur due to various orthopedic conditions. It describes 14 different pathologies including how they impact gait patterns, their causes and mechanisms, and examples of treatment approaches. The pathologies involve the hip, knee, ankle, and include conditions like arthritis, leg length discrepancies, contractures, and muscle weaknesses that can result in antalgic, Trendelenburg, toe walking and other abnormal walking patterns. The document provides detail on gait analysis and the phases and terminology used to describe normal and pathological walking motions.