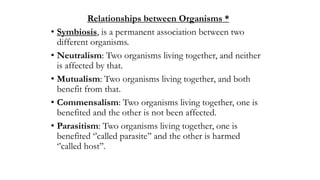
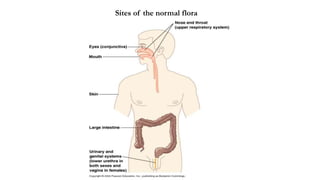
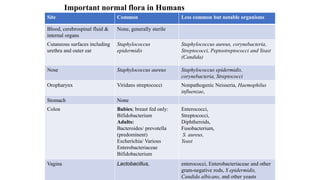
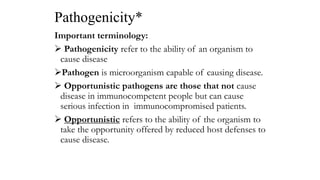
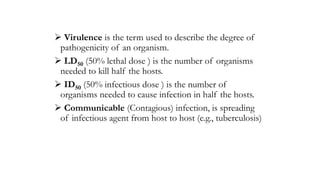
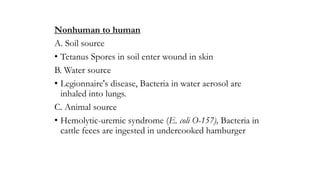
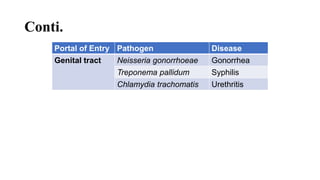
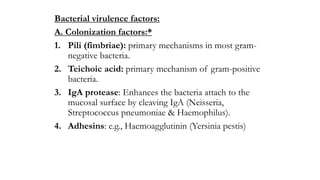
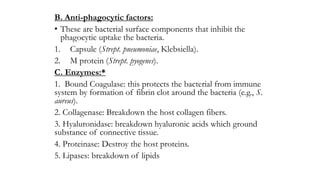
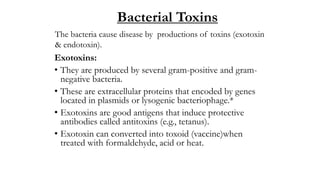
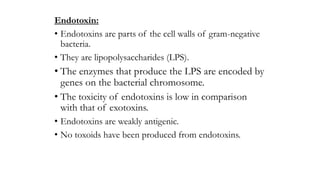
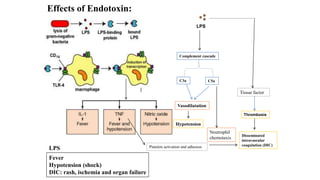
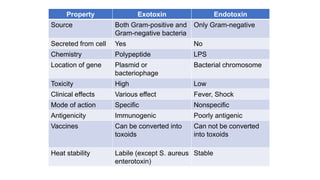
This document discusses normal flora and bacterial pathogenesis. It defines normal flora as microorganisms regularly found on body surfaces and outlines the groups of permanent and transient residents. Microflora plays both protective and nutritional roles for the host but can also cause opportunistic infections under certain conditions. The document then examines bacterial pathogenicity factors like virulence and modes of transmission. It describes common bacterial virulence mechanisms including colonization factors, anti-phagocytic factors, and exotoxins. Finally, it differentiates between exotoxins produced by bacteria and endotoxins, which are structural components of gram-negative bacteria.