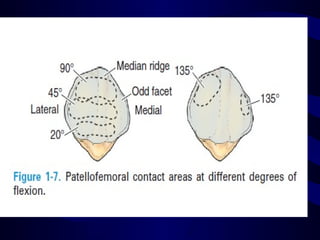
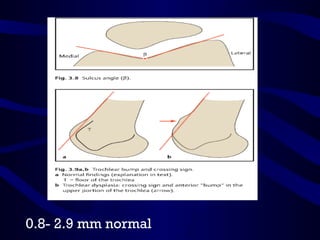
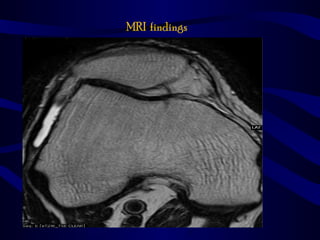
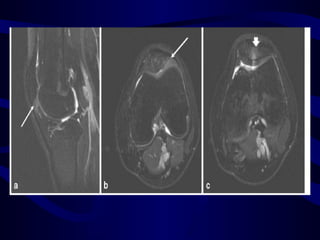
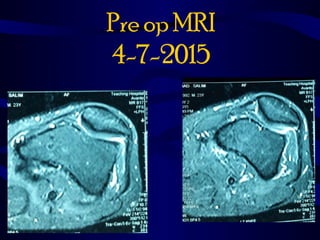
Lateral patellar compression syndrome is caused by improper tracking of the patella in the femoral trochlear groove without instability. It is associated with increased pressure on the lateral facet due to tight lateral soft tissues. Patients present with chronic anterior knee pain that is exacerbated by activities like stairs and sitting. Examination reveals tenderness over the lateral patella. Treatment begins with physical therapy focusing on vastus medialis strengthening. For refractory cases, arthroscopic lateral release can provide relief by correcting the lateral tilt.