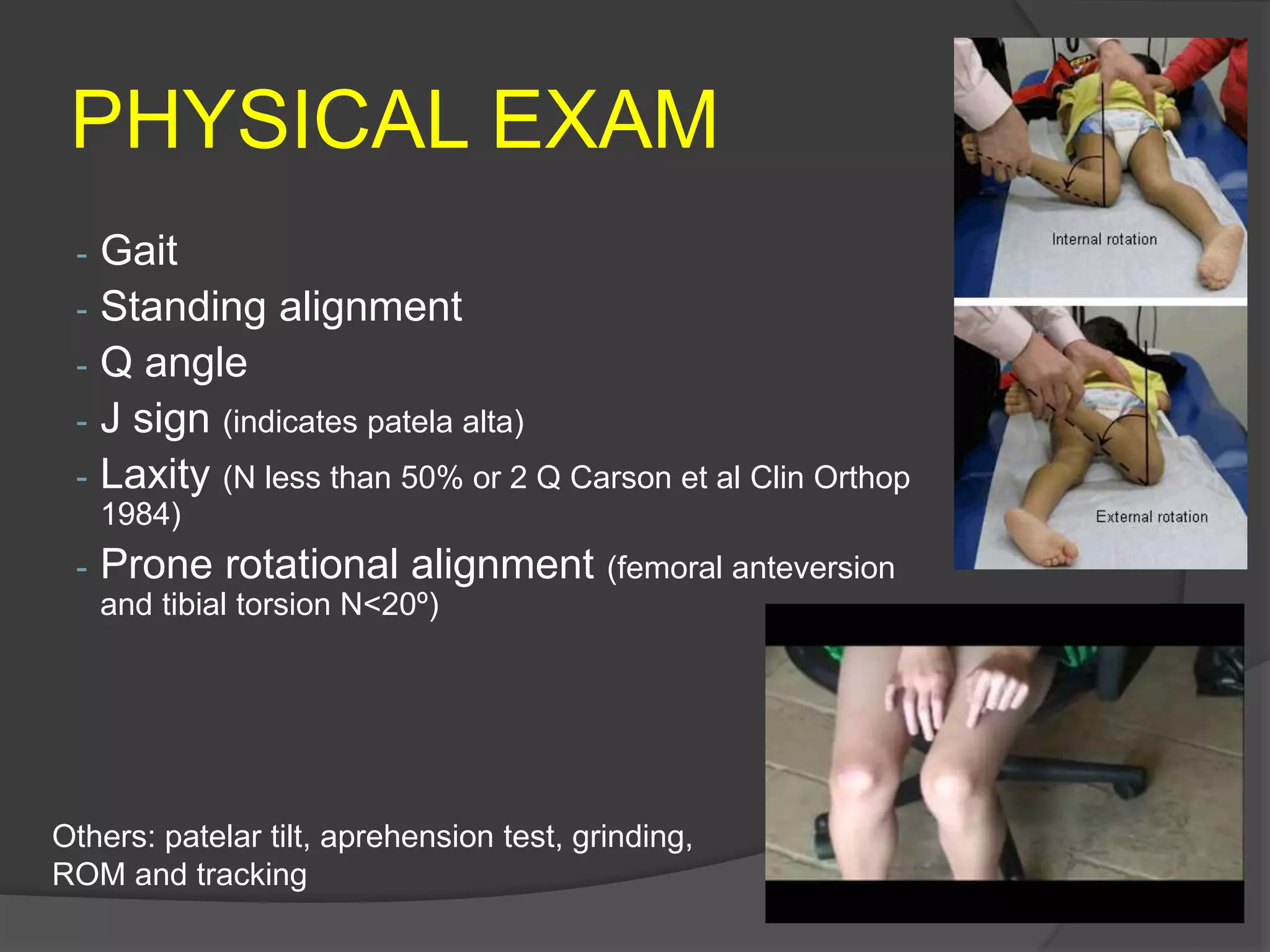
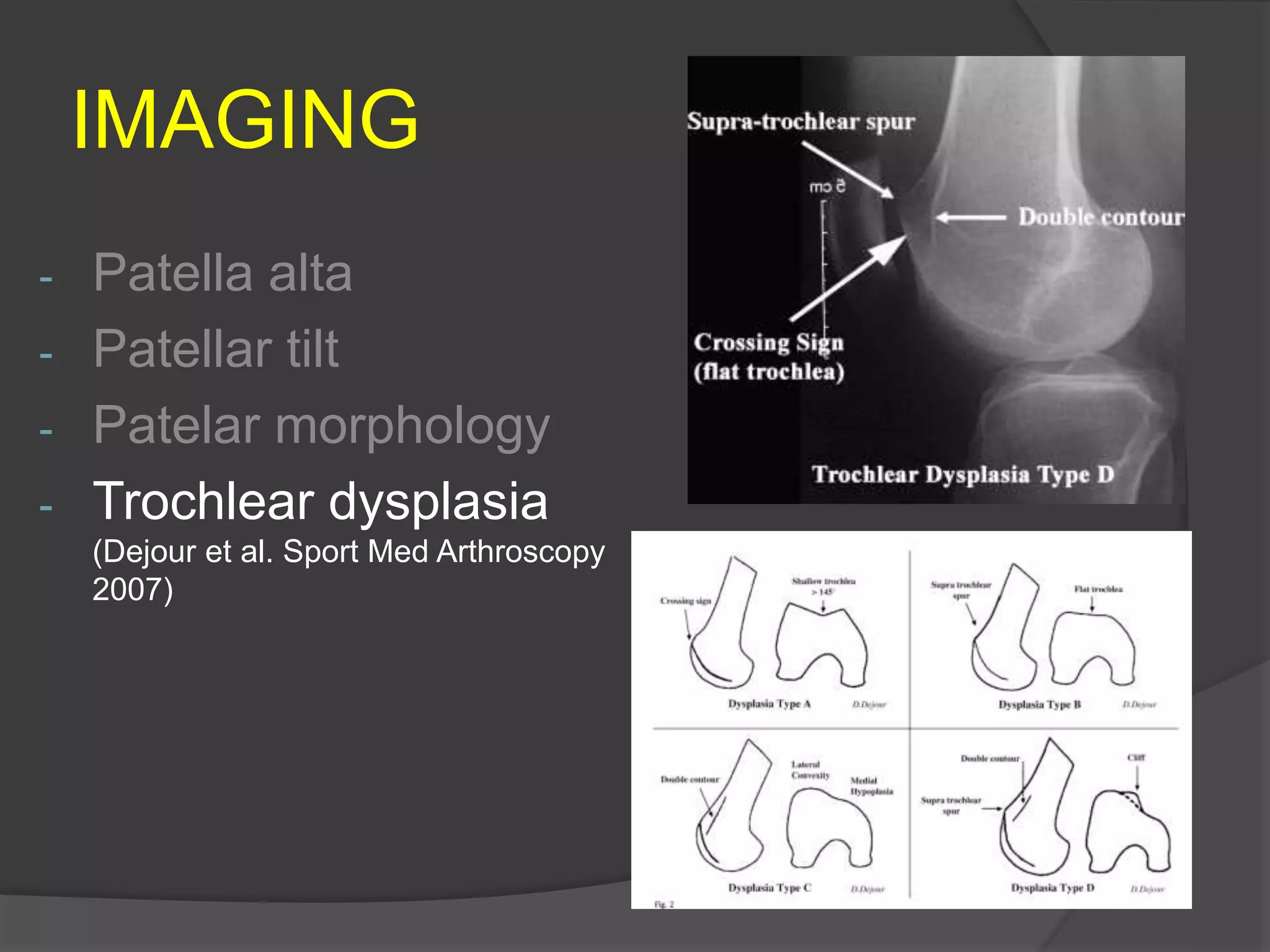
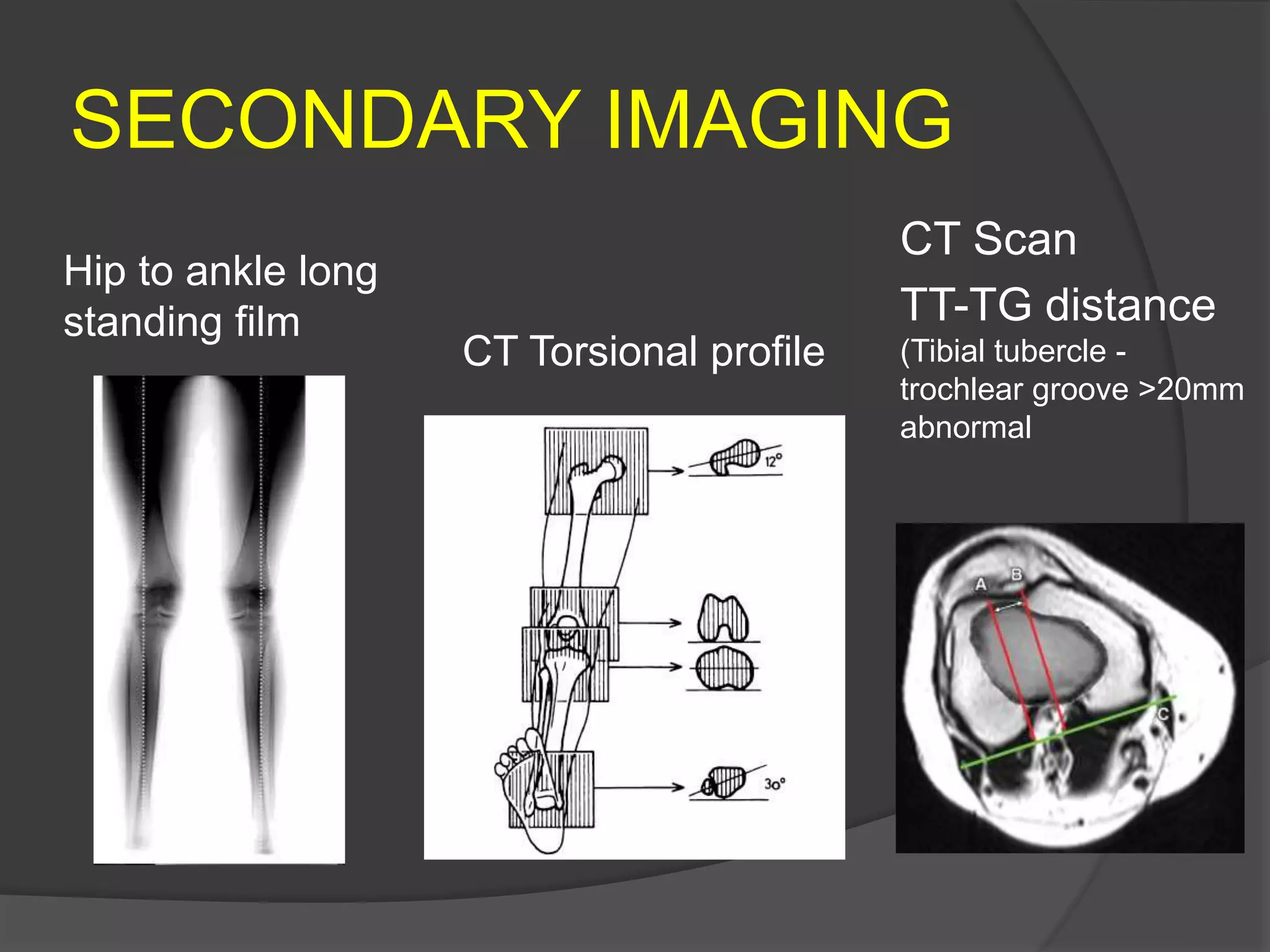
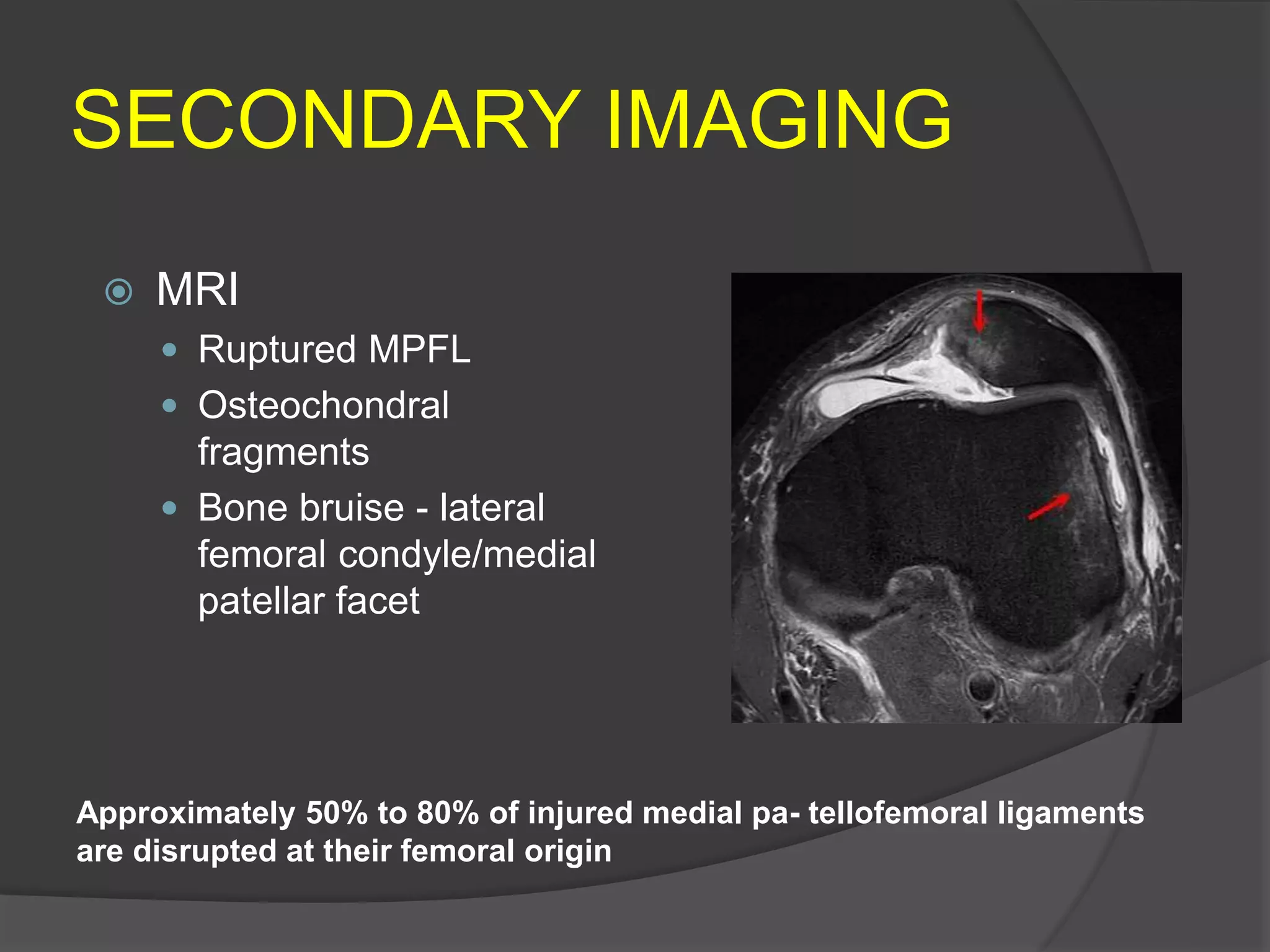
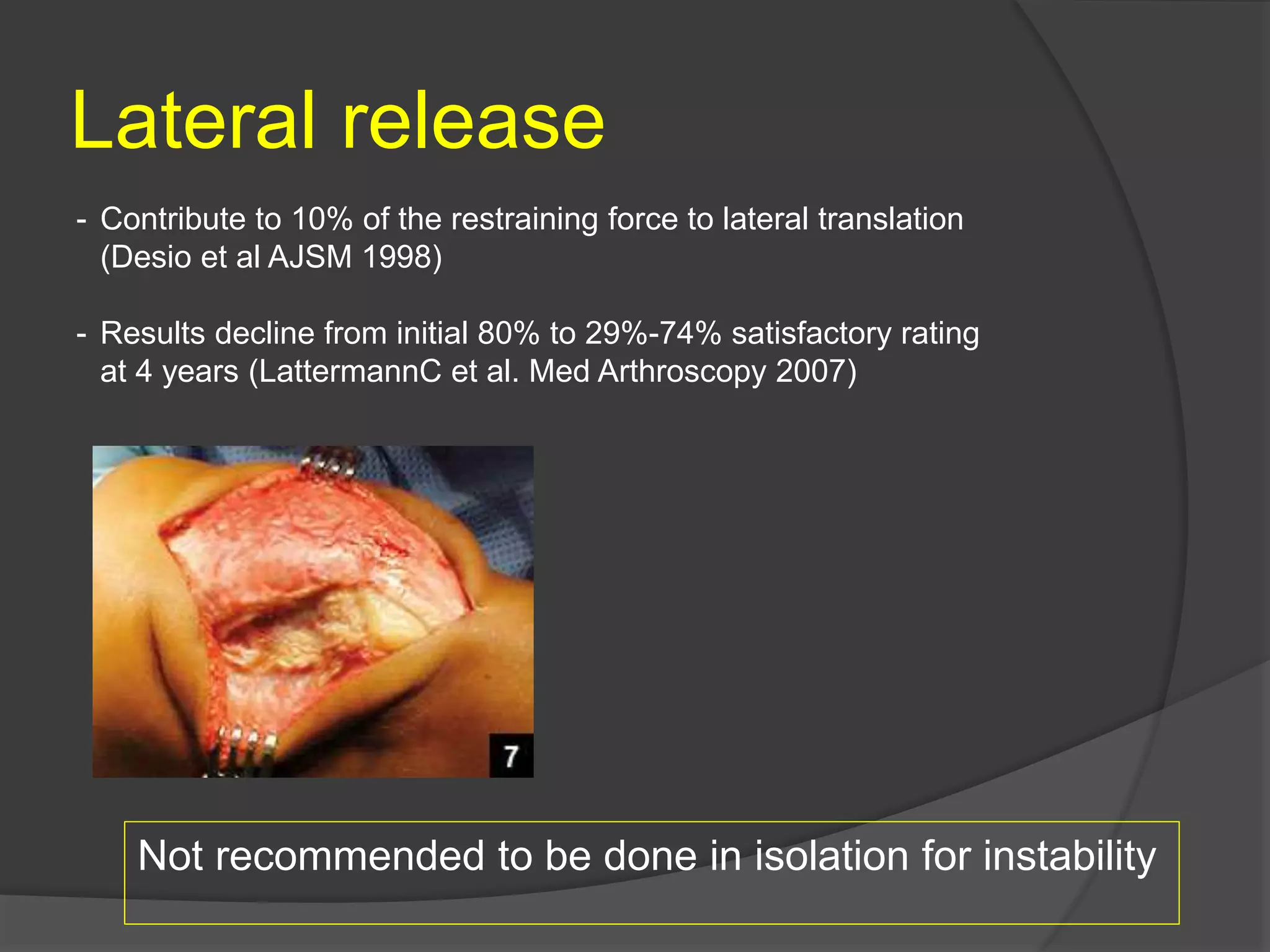
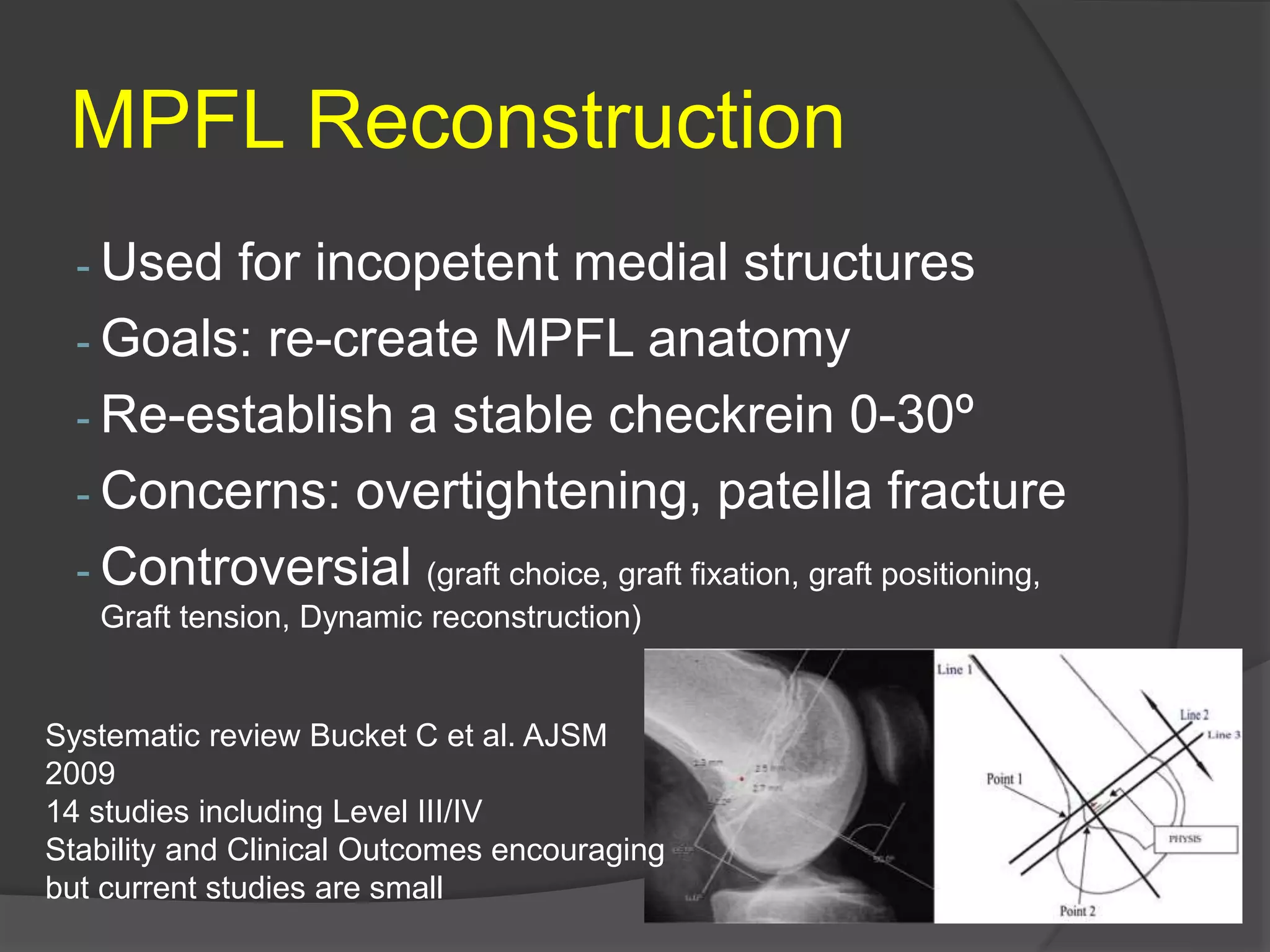
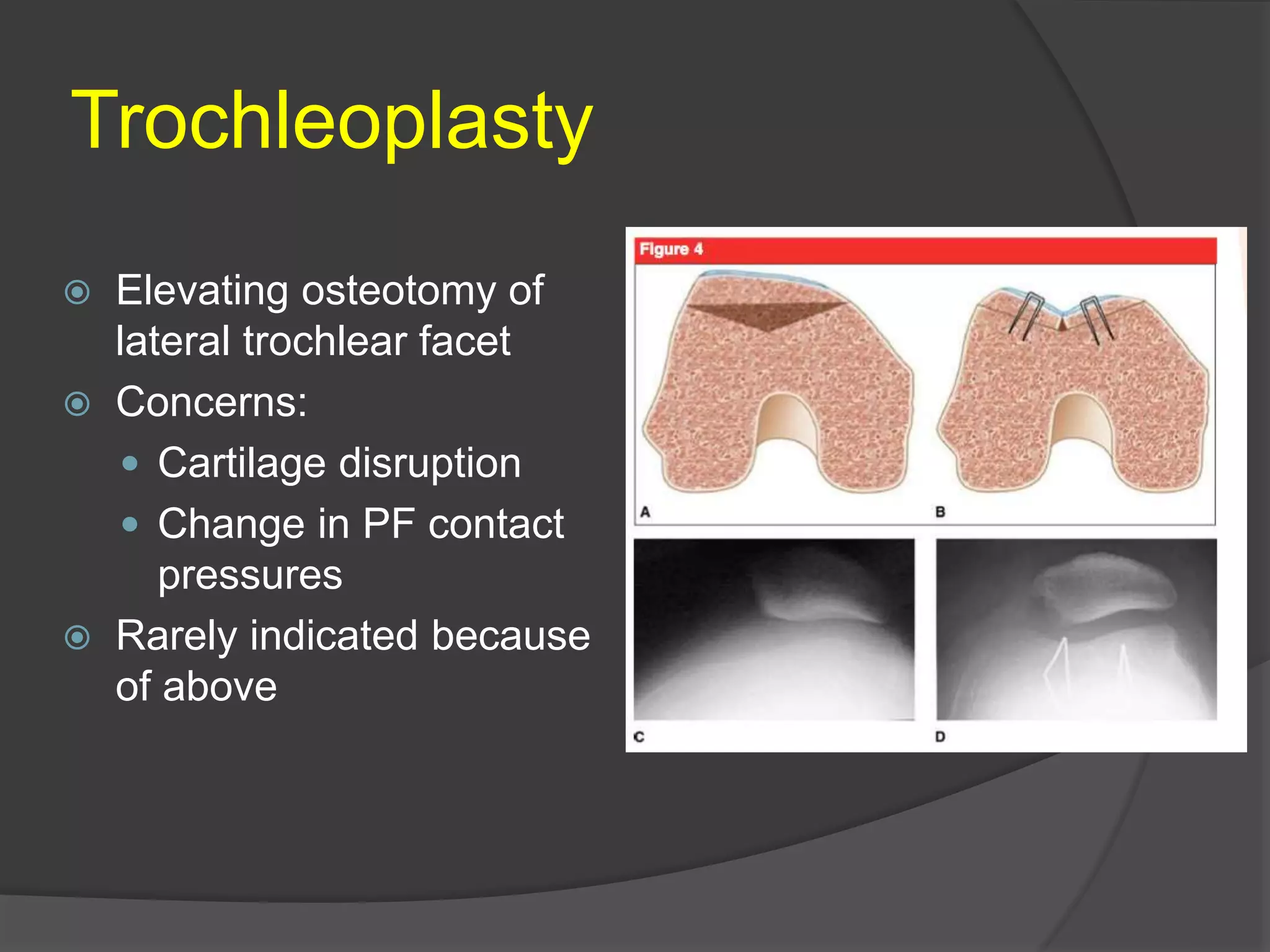
This document discusses the diagnosis and treatment of patellofemoral instability. It notes that instability can be traumatic or atraumatic, with recurrent dislocations having a 50% chance of further episodes. Non-operative treatments include physical therapy targeting muscles like the VMO. Surgical options include soft tissue procedures like medial repair or MPFL reconstruction, and bone procedures like trochleoplasty, tubercle osteotomies, or distal realignment. MPFL reconstruction is commonly used for incompetent medial structures but studies on techniques are limited. Treatment should be customized based on the underlying anatomical abnormalities or soft tissue insufficiencies identified in each individual case.