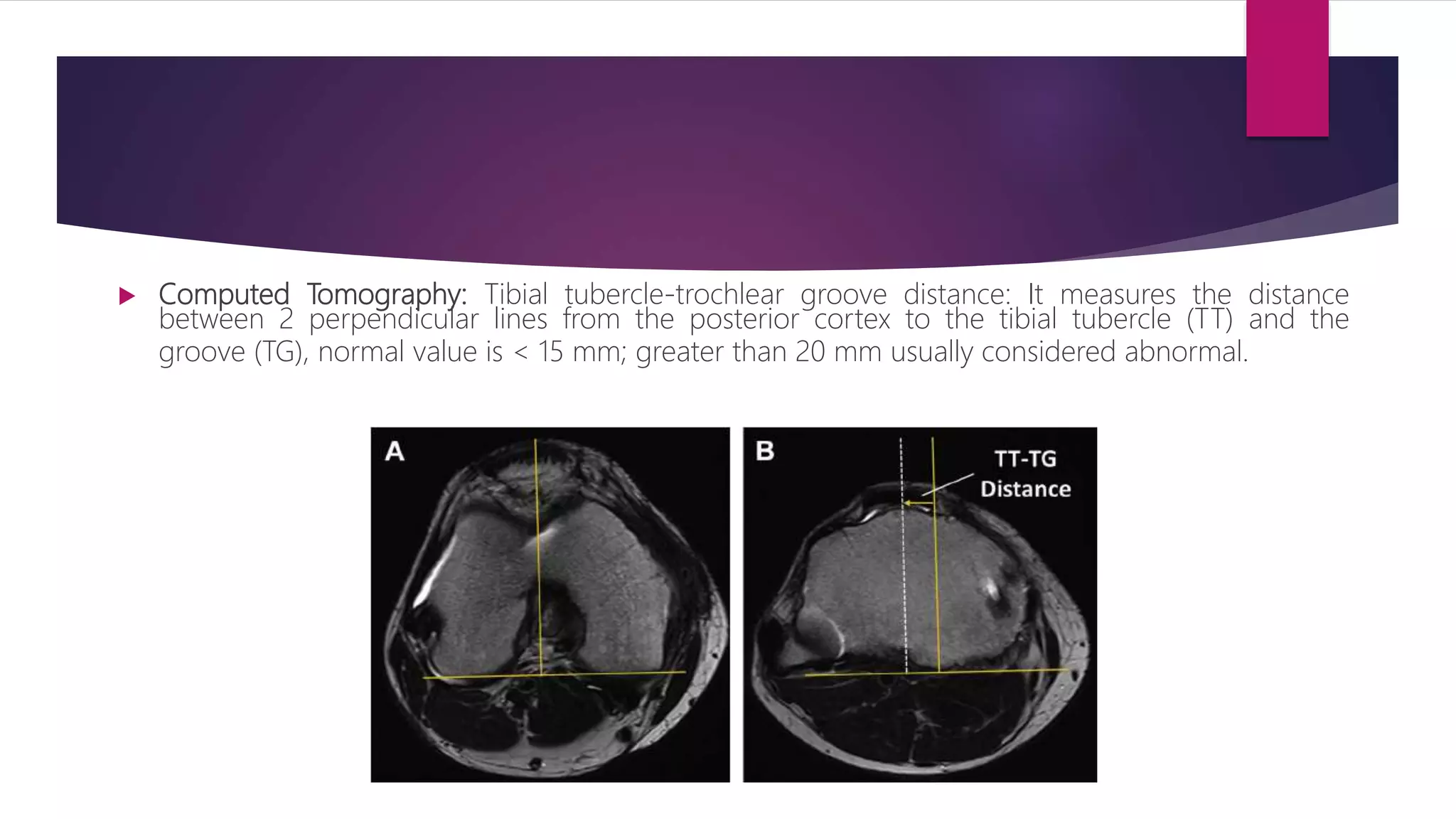
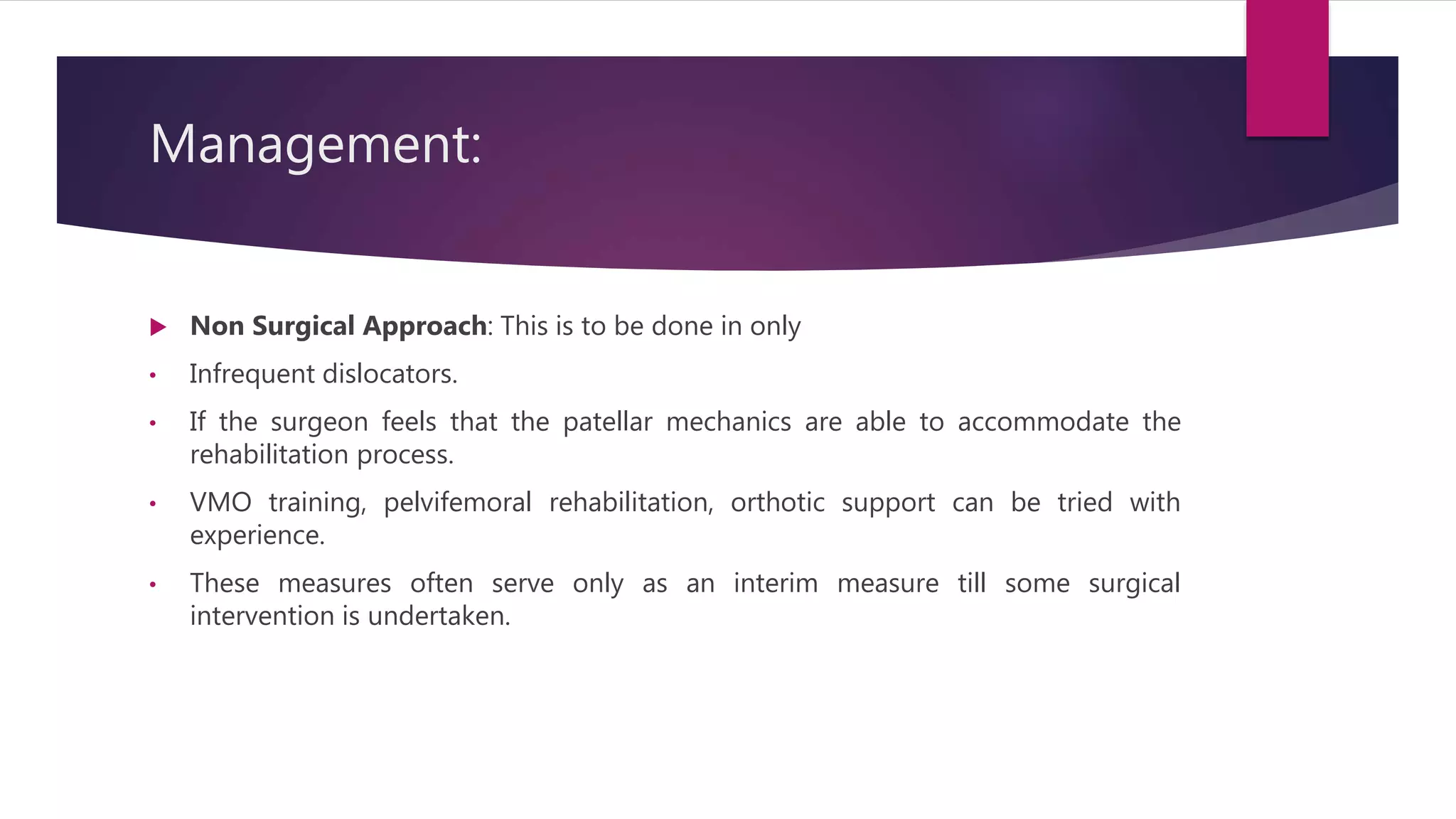
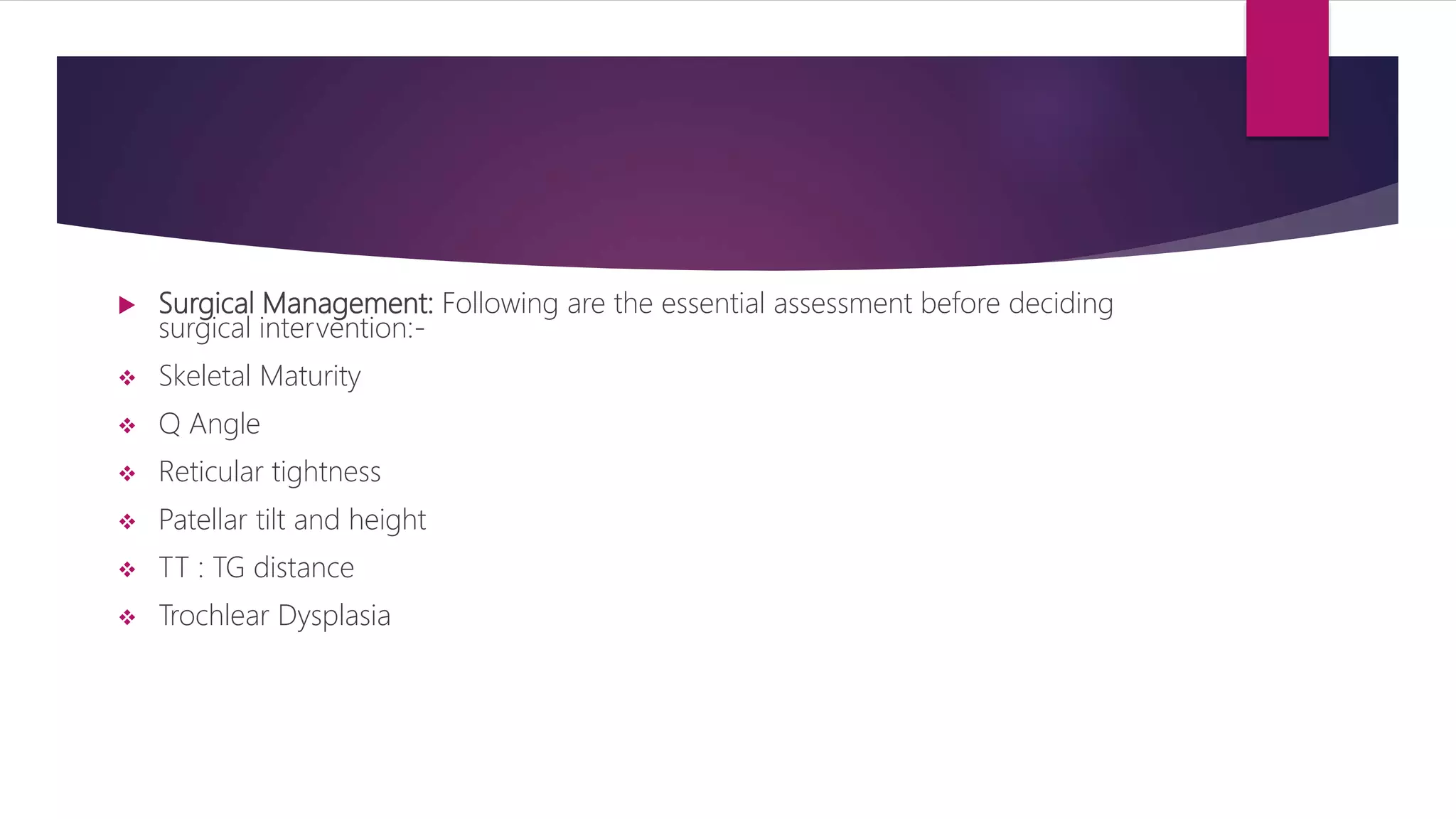
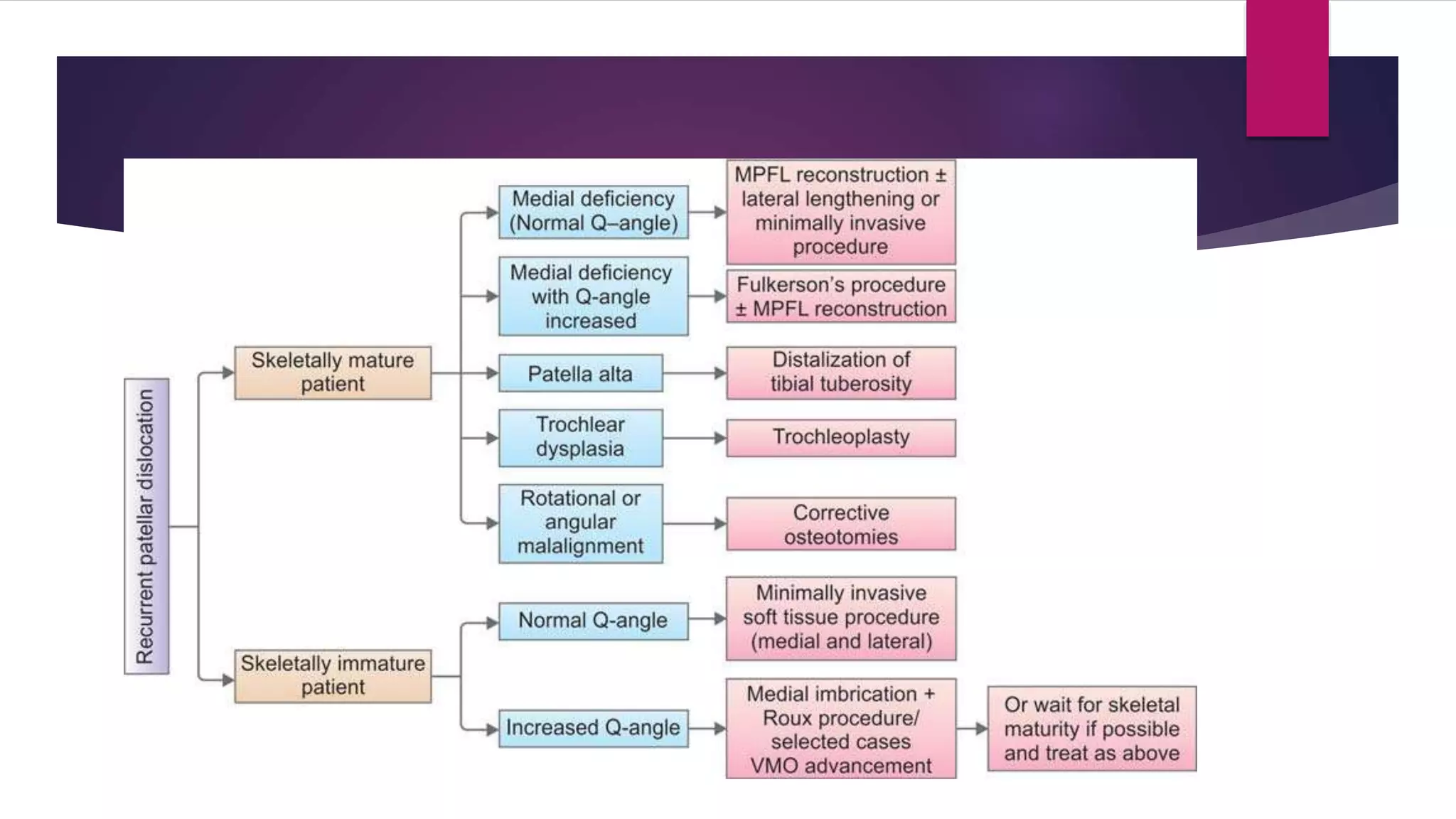
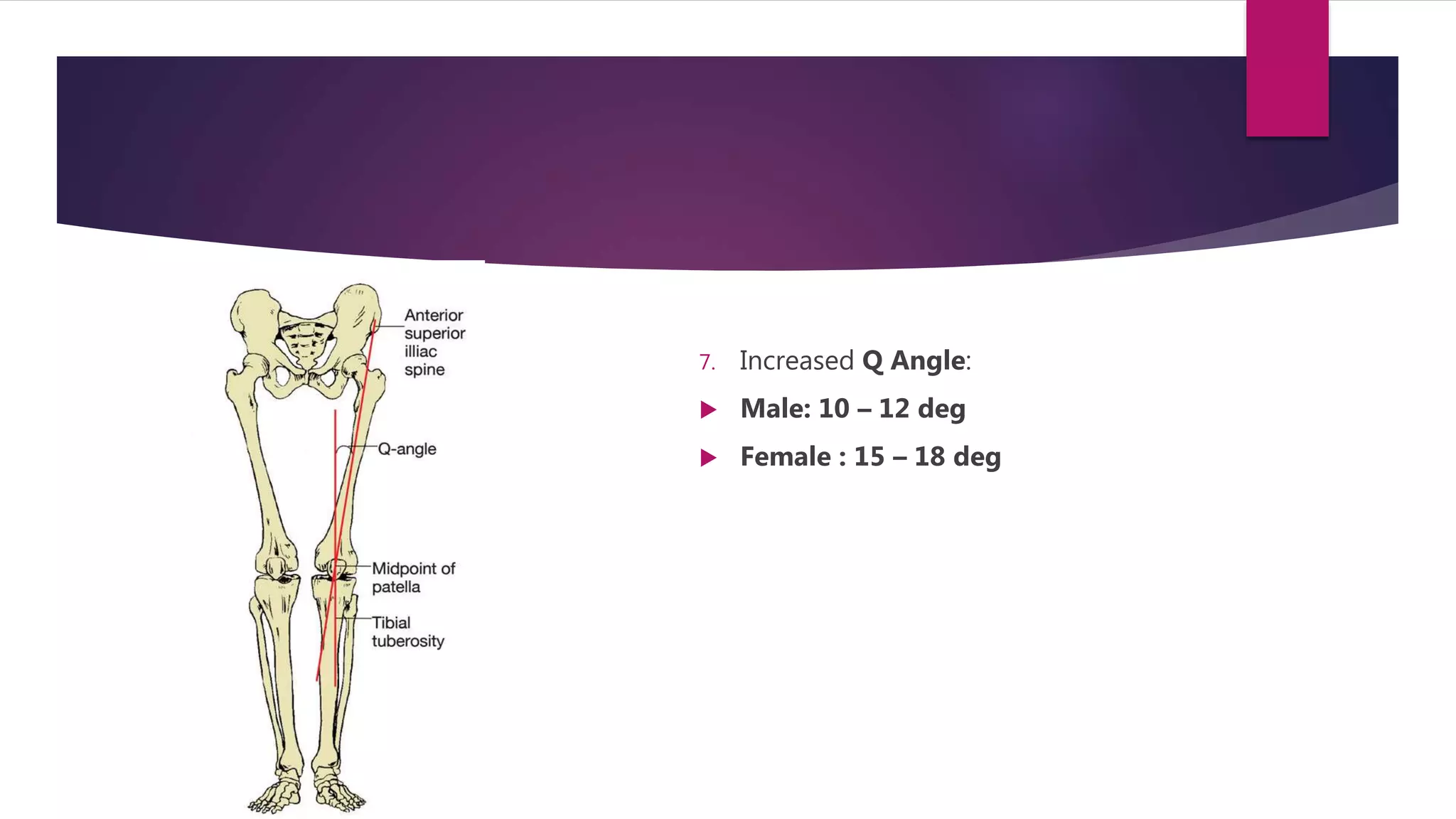
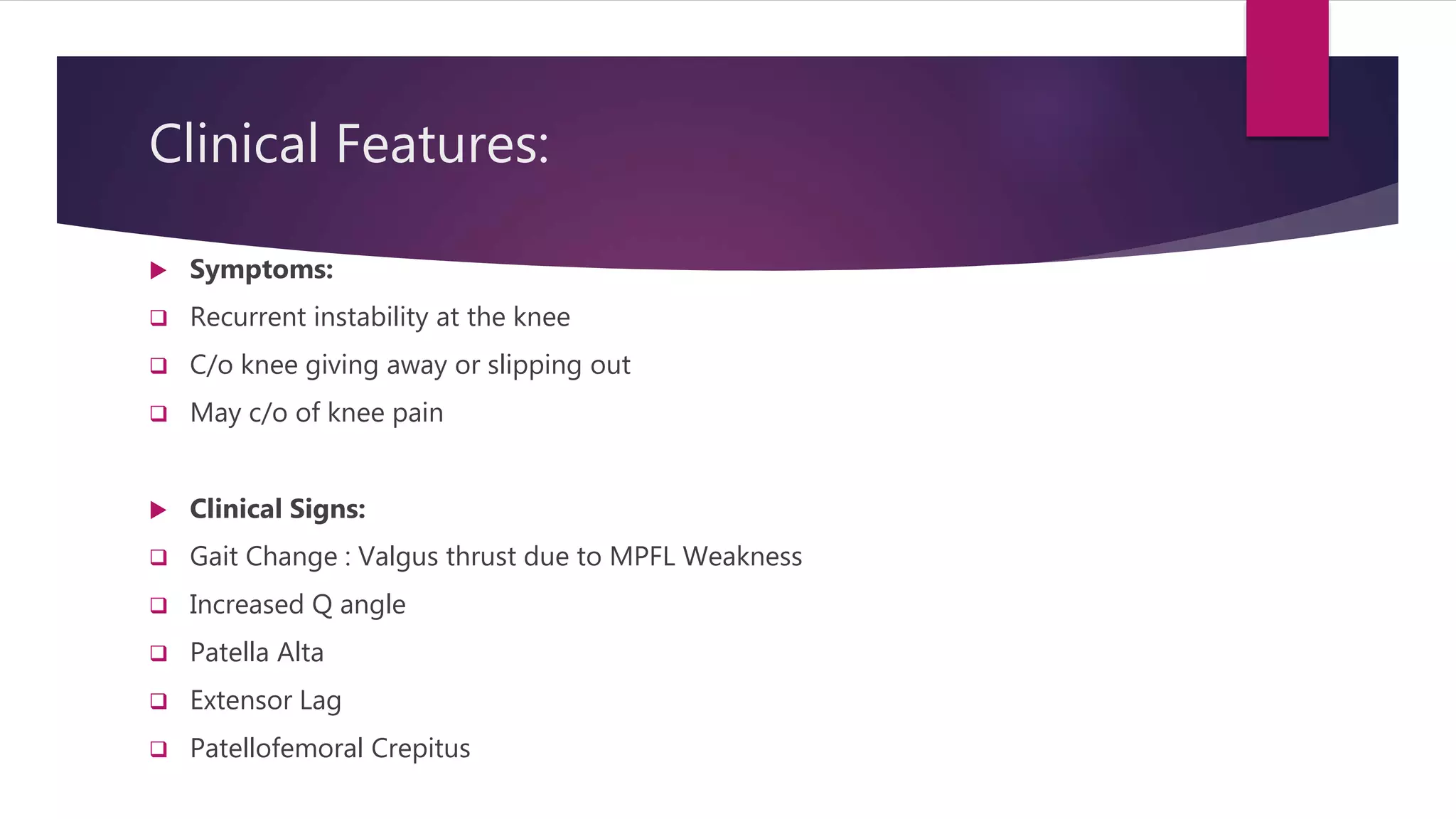
This document discusses patellar instability, including types, causes, clinical features, investigations, and management. It describes how the patella can subluxate or dislocate from the trochlear groove, with recurrent dislocation having higher risks of further episodes. Predisposing factors include previous injury, ligament laxity, alignment issues, and trochlear dysplasia. Clinical exams help assess for instability. Imaging can evaluate bony anatomy and alignment. Non-surgical management uses rehabilitation, while surgery considers skeletal maturity, alignment factors, and trochlear anatomy to determine the appropriate realignment procedure.





![ Apprehension test [Fulkerson relocation Test]:](https://image.slidesharecdn.com/patellarinstability-200511114209/75/Recurrent-Patellar-instability-14-2048.jpg)
![ Increased Passive patellar lateral translation [Patella Glide test]:](https://image.slidesharecdn.com/patellarinstability-200511114209/75/Recurrent-Patellar-instability-15-2048.jpg)