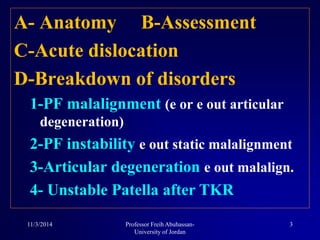
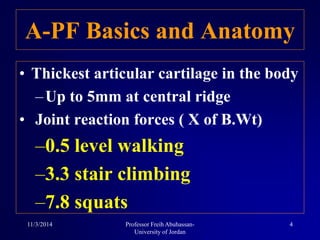
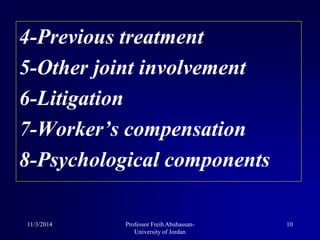
This document discusses patellofemoral pain syndrome (PFPS). It covers the anatomy of the patellofemoral joint, assessment of PFPS, acute patellar dislocation, and treatment options. The key points are:
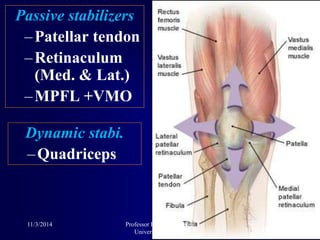
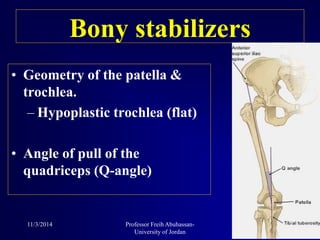
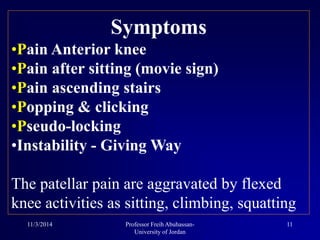
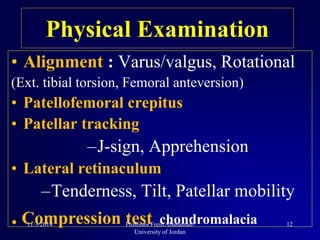
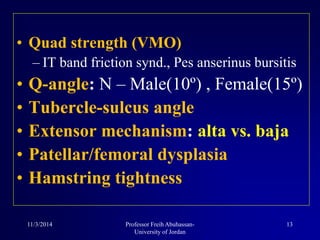
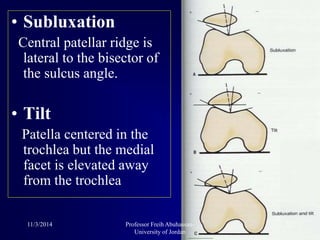
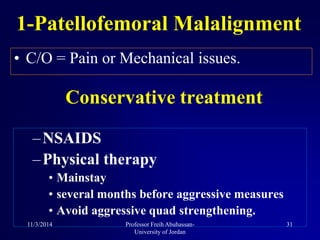
- PFPS is caused by abnormalities that affect patellar tracking, including malalignment, instability, and articular degeneration.
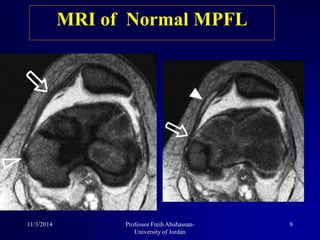
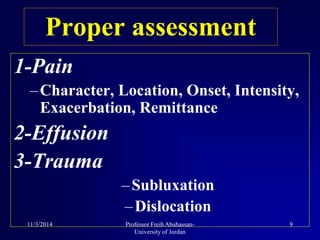
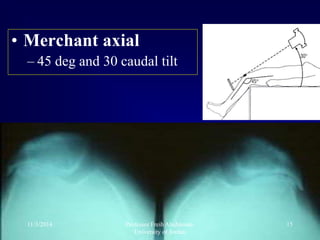
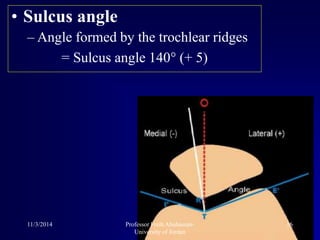
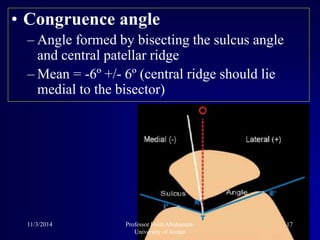
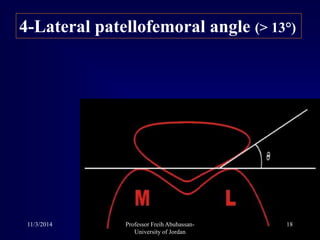
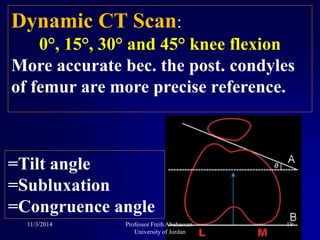
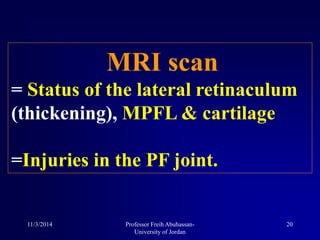
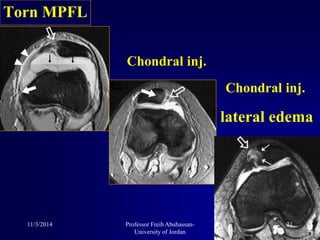
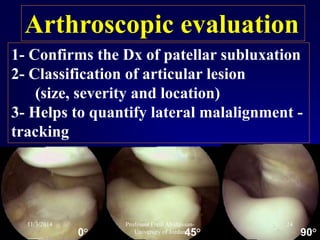
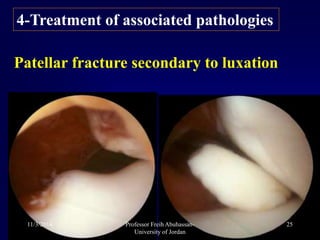
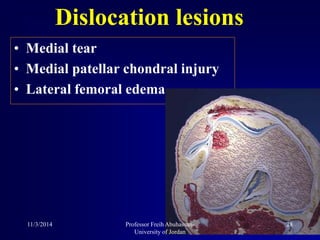
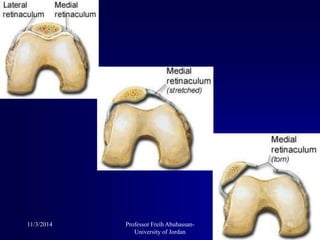
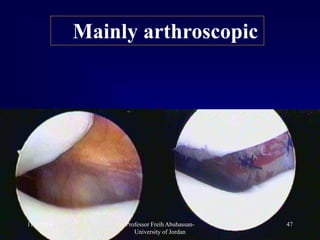
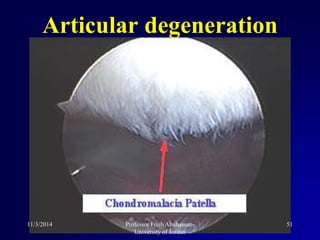
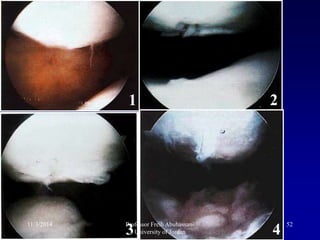
- Assessment involves physical exam, radiographs, MRI, and sometimes arthroscopy to evaluate soft tissues and cartilage damage.
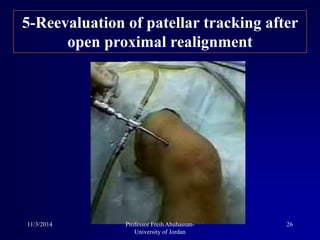
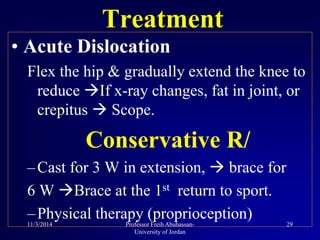
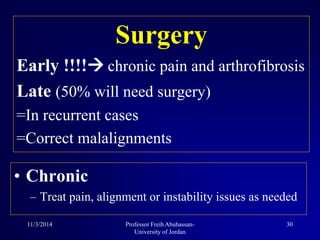
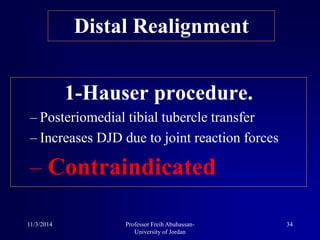
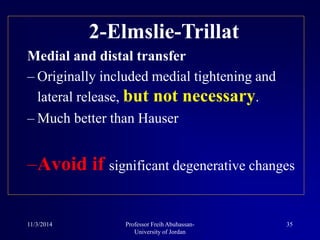
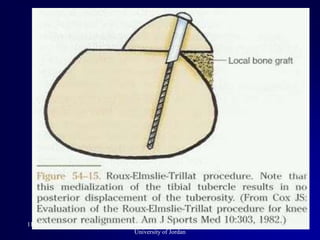
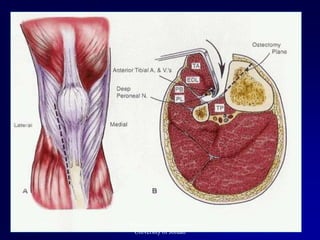
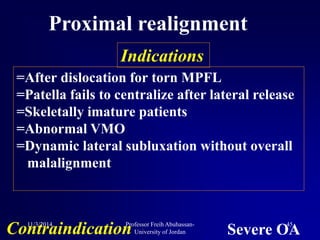
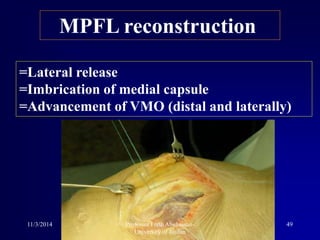
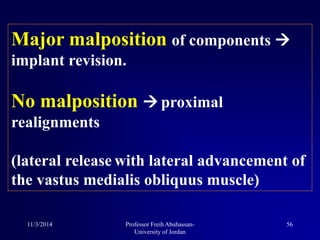
- Treatment progresses from nonsurgical options like physical therapy to realignment procedures like lateral release or tibial tubercle transfer if conservative treatment fails.